FIGURE 35-1. Vascular anatomy of the pelvis (From Callaghan JJ, Rosenberg AG, Rubash HE. The Adult Hip 2/e. Philadelphia, PA: Lippincott Williams & Wilkins; 2006, with permission).
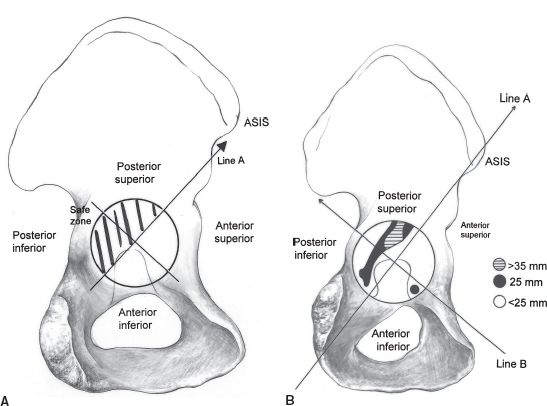
FIGURE 35-2. A: The acetabulum may be divided into four quadrants using an imaginary line drawn from the anterior superior iliac spine to the ischium (Line A) and a perpendicular line (Line B). The posterior superior quadrant provides the safest screw placement and the best bone. B: Screws placed perpendicular to the cup surface into the anterior quadrants risk vascular injury (From Callaghan JJ, Rosenberg AG, Rubash HE. The Adult Hip 2/e. Philadelphia, PA: Lippincott Williams & Wilkins; 2006, with permission).
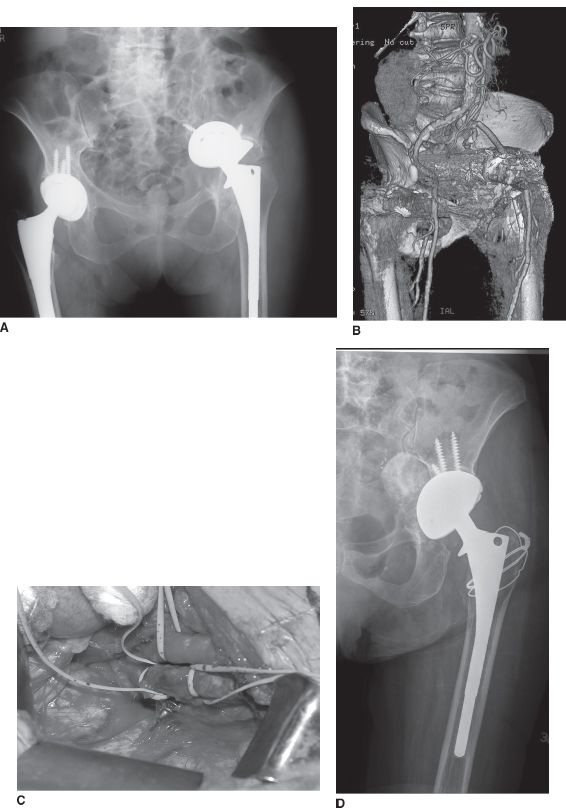
FIGURE 35-3. A: Radiograph demonstrating failed left THA with marked intrapelvic acetabular component protrusion. The cup had migrated acutely and the surgeon was concerned it might abut intrapelvic vascular structures. B: A computed tomography scan was performed with intravascular contrast, metal artifact suppression, and three-dimensional reconstruction. The acetabular screw abuts the iliac vein. C: A retroperitoneal approach was performed to protect the pelvic vasculature during implant extraction. The screw is next to the iliac vessels. D: Radiograph of the same hip after revision (Courtesy of M. Cabanela).
Femoral artery or vein injury may occur during revision from retractors, sharp injury, or cerclage. Prompt vascular surgery intervention is required. Perforating vessels from the profunda femoris artery can cause brisk bleeding around the femoral shaft, most commonly associated with placing femoral cerclage cables or wires. These vessels can be identified and then controlled with electrocautery or ligation; sometimes this requires extra exposure to identify the bleeding vessels, by opening the linea aspera.
Intraoperative Fracture Intraoperative fracture of the acetabulum can occur during component removal or component implantation. Excessive undersizing of the cup compared to the reamed size of the acetabulum predisposes to fracture.3 Minor fractures of the acetabular rim may be ignored. Fractures of an entire acetabular wall or a pelvic column, or fractures producing acute pelvic discontinuity fortunately are uncommon and usually are treated with plate fixation.
Intraoperative greater trochanteric fractures may occur during implant removal, femoral preparation, femoral component implantation, or hip reduction.4 Patients with very poor bone quality and those with bone defects in the greater trochanter or at the base of the greater trochanter are at greatest risk. Treatment involves trochanteric fixation with wires, a claw, or hook plate depending on the fracture pattern and surgeon’s preference.
The frequency of intraoperative femur fractures associated with revision THA varies with the method of hip exposure, type of implant removal, and type of implant inserted.4–8 In a report from the Mayo Clinic, the risk of intraoperative fracture during revision THA in 6,349 cases was 7.8%.9 Intraoperative femoral shaft fracture may occur during exposure, failed implant extraction, femoral preparation, or implant insertion. In a series of 22 intraoperative fractures reported by Johanson et al.10 before widespread use of uncemented implants, 11 occurred during cement removal, 5 during implant removal, 3 during hip dislocation, and 2 during femoral reaming. Five of ten intraoperative fractures reported by Christensen occurred during hip dislocation.11 Poor bone quality is the most common risk factor. The risk of fracture during hip exposure may be reduced by careful and patient exposure of the femur before hip dislocation is attempted. Modern uncemented femoral implants may be associated with a higher risk of intraoperative femur fracture: Meek et al.12 reported 64 intraoperative femur fractures in 211 revisions with extensively coated uncemented stems. Issack et al.6 reported intraoperative fractures in 9 of 175 revisions treated with an extensively coated uncemented stem.
Intraoperative fractures of the proximal femur usually can be treated with reduction using cerclage followed by insertion of a long stemmed femoral component (usually uncemented). Fractures of the distal femur most commonly occur during insertion of an uncemented component. Some fractures may be avoided by prophylactic placement of a cerclage cable or wire before implant impaction. If an extended greater trochanteric osteotomy has been used, routine placement of prophylactic cerclage just distal to the osteotomy may reduce the risk of fracture (Fig. 35-4). Fracture risk also can be minimized by careful implant sizing and judicious impaction force during implantation. Most proximal intraoperative femur fractures can be managed by bypassing the fracture with a longer femoral component (if needed) that gains fixation distal to the fracture and stabilizing the fracture with cerclage (Fig. 35-5).
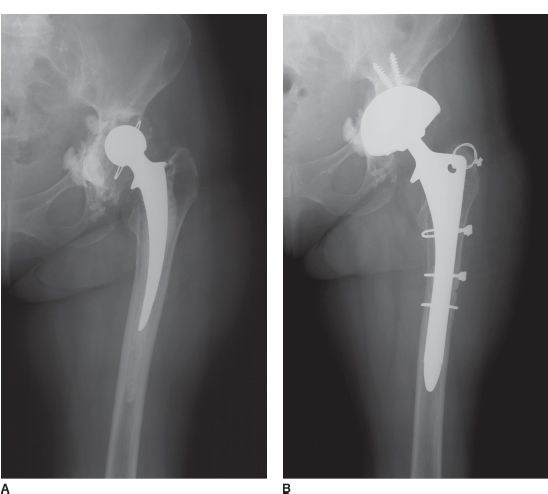
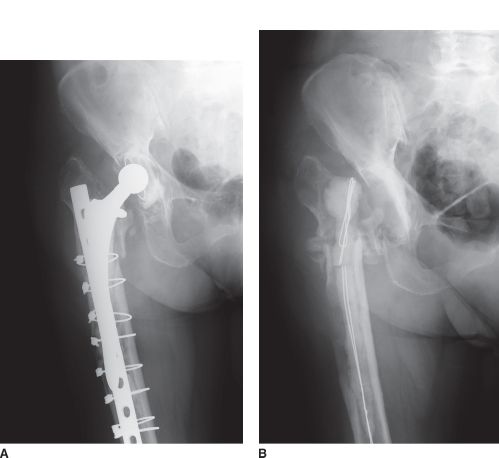
FIGURE 35-4. A: Radiograph of failed THA. B: Radiograph after revision THA with extended greater trochanteric osteotomy and uncemented extensively porous coated stem. Note a prophylactic cerclage cable was placed just distal to the osteotomy before implant impaction to minimize the risk of intraoperative fracture.
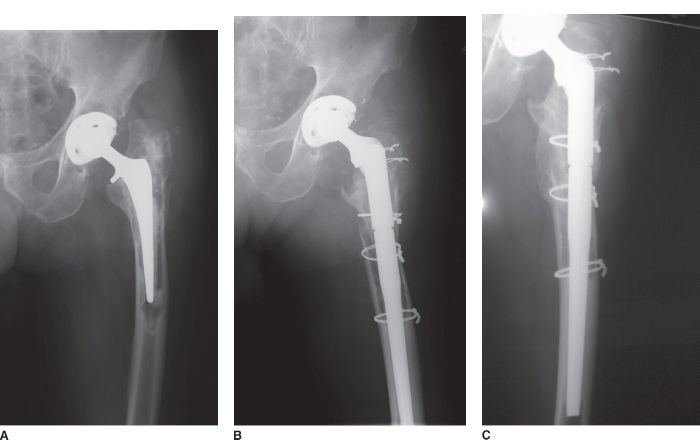
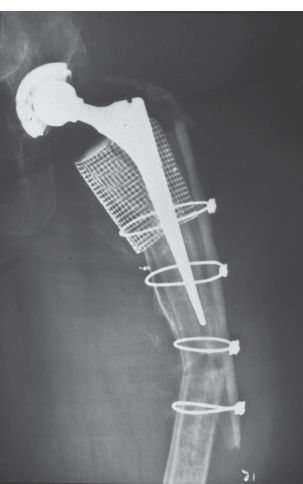
FIGURE 35-5. A: Hip radiograph of patient with failed THA with marked femoral osteolysis and varus femoral remodeling. B: An extended greater trochanteric osteotomy was performed to facilitate exposure and implantation of a new stem. During the operation, the weak proximal medial femoral bone fragmented—not unexpectedly. As had been planned preoperatively, a fluted tapered modular femoral component, which gains axial and rotational stability distal to the fragmented proximal bone was placed. The proximal bone was repaired with cerclage using the prosthesis as a scaffold. C: Radiograph demonstrating fracture healing and a stable implant.
Most distal fractures are longitudinal cracks. If identified during surgery, fractures of this pattern are best treated with cerclage. In the series of Meek et al.,12 from Vancouver, the risk factors for intraoperative fractures with an extensively coated uncemented stem included more severe prerevision bone loss, a low femoral cortex to canal ratio, and use of a large diameter stem. Importantly, these intraoperative cracks did not have a negative effect on the radiographic or clinical outcome of the procedure. If not identified until after surgery, nonoperative management with protected weight bearing may be considered unless the fracture appears potentially unstable, in which case return to the operating room for stabilization is advisable.13
Complete fractures that clearly disrupt femoral continuity are best treated with stabilization using cerclage, strut allografts, or plates, depending on the fracture pattern and location. Optimal treatment of an intraoperative fracture during an operation can prevent a great deal of subsequent trouble (Fig. 35-6).11
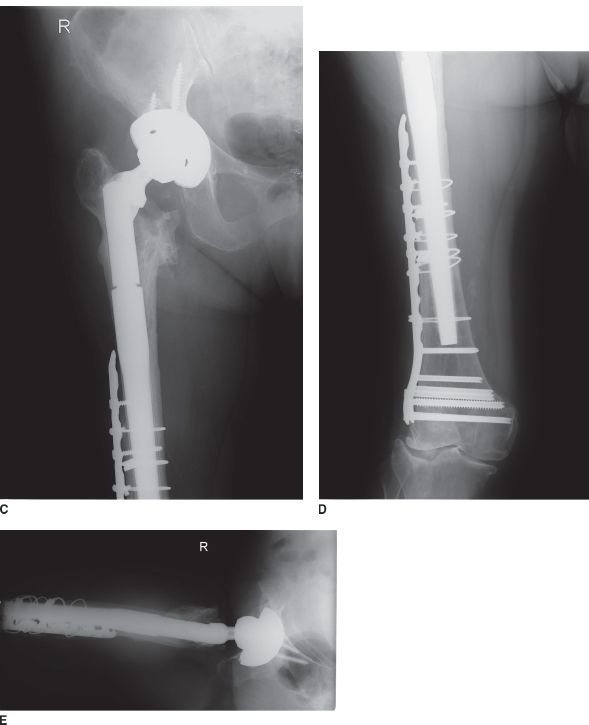
FIGURE 35-6. A: Preoperative radiograph of patient with failed revision THA due to infection and previous periprosthetic femur fracture. B: Radiograph after first stage of treatment with implant removal and antibiotic-loaded cement spacer placement. C, D, and E: Radiographs 2 years after revision THA. At the time of femoral implant placement, an unstable distal fracture occurred at the stem tip through an old screw hole. Internal fixation with a locking condylar plate was performed. The fracture healed and the stem remained stable.
Intraoperative Instability When intraoperative hip stability is suboptimal, the source of the problem should be sought and treatment should follow accordingly.14 Suboptimal implant position should be corrected, if possible, or compensated for with elevated rim or face-changing acetabular polyethylene liners. Suboptimal soft tissue tension can be improved by adding length to the femoral side with a number of methods including a longer modular neck length, a longer modular proximal hip body, or more proximal seating of a femoral component. Lateralized acetabular liners can also reduce femoral-pelvic bone impingement and also provide extra soft tissue tension. Impinging soft tissues or bone may be removed or trimmed. Tripolar constructs or constrained implants may be used for serious deficiency of the abductor mechanism or other difficult to manage intraoperative instability problems.
COMPLICATIONS MANIFESTED POSTOPERATIVELY
Periprosthetic Fracture Patients treated with revision THA are at greater risk for postoperative fracture than patients with primary THA, due to bone defects and reduced bone quality (Fig. 35-7). Postoperative periprosthetic fracture after revision THA is managed according to the principles of periprosthetic fracture management discussed in detail in Chapter 32.
FIGURE 35-7.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree