Fig. 2.1
Classification of Bankart and Bankart variant lesions according to Woertler [5]. (a) Bankart lesion, (b) bony Bankart lesion, (c) Perthes lesion, (d) ALPSA (anterior labro-ligamentous periosteal sleeve avulsion) lesion, (e) GLAD (glenolabral articular disruption) lesion, (f) HAGL (humeral avulsion of glenohumeral ligaments) lesion. LLC anteroinferior labro-ligamentous complex, P scapular periosteum, HH humeral head, AC articular cartilage of glenoid, IGHL inferior glenohumeral ligament
A Hill-Sachs lesion is another typical injury of the humeral head. It is an impression fracture at the posterosuperior side of the humeral head, indicating a traumatic history of the anterior shoulder dislocation. In contrast, a reversed Hill-Sachs lesion occurs in the context of a posterior dislocation, typically in association with a convulsion. The reversed Hill-Sachs lesion is located at the anterior side of the humeral head, just in front of the lesser tuberosity.
In the elderly, the injury pattern changes. It becomes more likely to obtain a rotator cuff tear with or without capsulolabral pathology.
The incidence of injuries associated with traumatic shoulder dislocations can be estimated according to Boss et al. [6]. They observed anterior labral lesions in 88 %, Hill-Sachs lesions in 54 %, superior rotator cuff tears in 22 %, tears of the subscapularis tendon in 16 %, lesions of the long head of the biceps in 10 %, SLAP lesions in 11 %, and fractures of the greater tuberosity in 4 %. If there is no intraoperative evidence of a Bankart lesion or one of its equivalents after traumatic shoulder dislocation, one should be alert for a HAGL lesion. HAGL lesions occur in up to 9 % according to Bui-Mansfield [7] (Figs. 2.2 and 2.3).
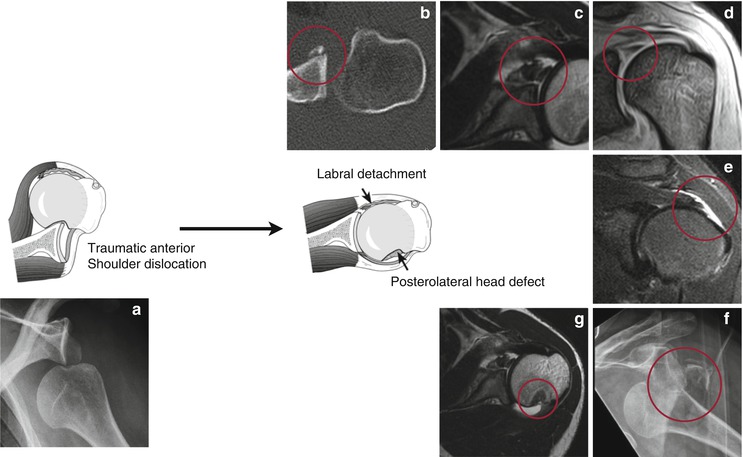
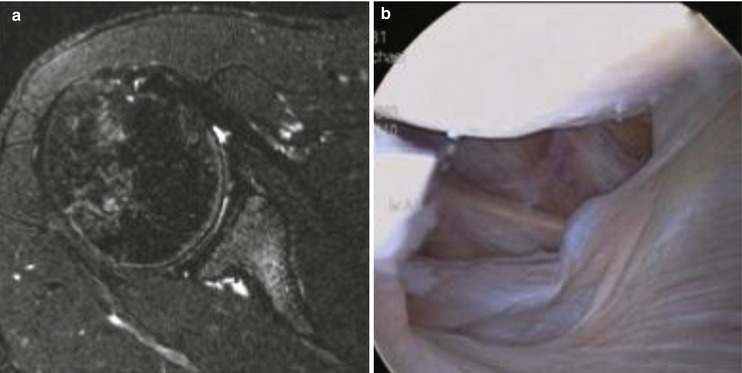
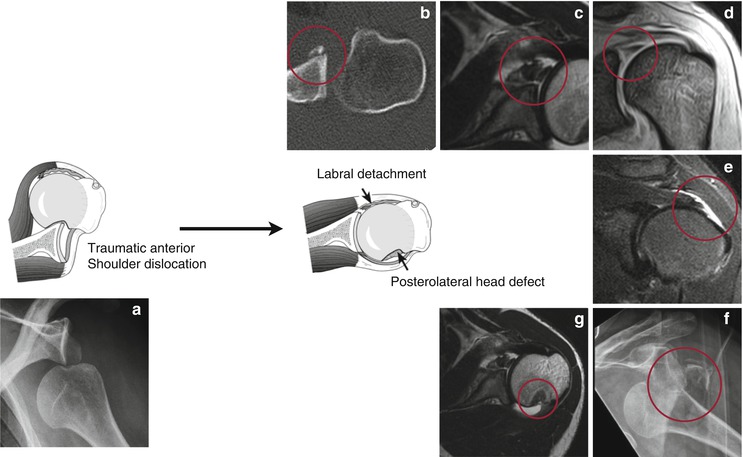
Fig. 2.2
Injury pattern after traumatic anterior shoulder dislocation. (a) Anterior shoulder dislocation. (b) Bony Bankart lesion. (c) Anterior Bankart lesion. (d) SLAP lesion. (e) Superior rotator cuff tear. (f) Fracture of the greater tuberosity. (g) Hill-Sachs lesion
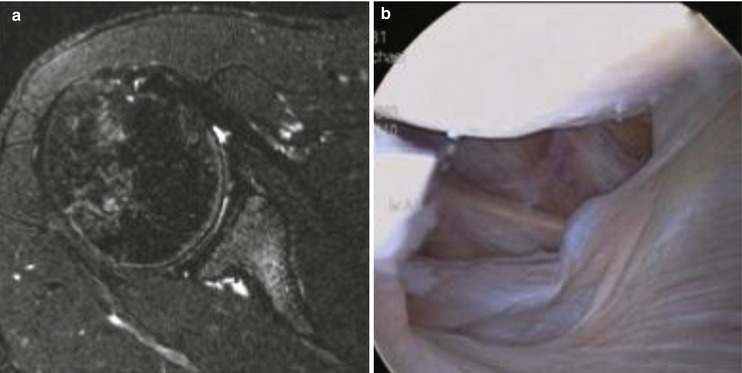
Fig. 2.3
HAGL-lesion. (a) Axial sequence of MRI. (b) Intraoperative picture
2.3 Diagnostic Procedures
A precise history and clinical examination provides valuable information, but, determination of the neurovascular status is of greatest importance. In particular, the status of the axillary nerve and the brachial plexus must be examined and documented.
It is also crucial to obtain “true” a.p. X-rays of the shoulder in order to detect a displaced shoulder. This kind of view tilts the X-ray beam in the line of the glenohumeral joint space. Any double contour around the glenoid is indicative of a displacement. An outlet view and/or an axillary view verify the displacement.
At this point in time, additional imaging procedures are not typically needed. If there is any sign of a fracture dislocation or locked dislocation, an additional CT scan is recommended, especially if a foreseen surgery becomes more likely.
After a reduction, a new clinical examination and imaging is necessary to document the successful reduction and to exclude any complications.
Further diagnostics are needed to estimate the degree of instability, especially the whole injury pattern. The gold standard is MRI of the shoulder. The MRI is useful detecting any capsulolabral injuries, injuries of the long head of the biceps, including its anchor, or the rotator cuff. It is also valuable to estimating bony and chondral lesions. Typically, an arthro MRI is not needed in the acute setting because the hemarthrosis provides sufficient contrasting of the intraarticular structures. In delayed or chronic situations, an arthro MRI is recommended to more precisely evaluate the capsulolabral injury, biceps anchor (SLAP lesions), and integrity of the rotator cuff. If there is an engaging Hill-Sachs lesion, bony Bankart lesion and/or glenoidal bone loss situation, an additional CT scan provides valuable further information. Glenoidal dysplasias and rotational deformity can also be detected using a CT scan. At least in the German-speaking countries, an arthro CT scan is not done routinely.
2.4 Initial Reduction of the Shoulder
There are many methods known for reducing a displaced shoulder. Even today, the painful and brusque procedures of Arlt and Hippokrates remain widespread. These are accompanied by a relatively high complication rate. Hence, they should no longer be applied in the clinical setting. Here, gentle and painless reduction techniques have proved themselves, for example, the technique of Stimson with or without manipulation of the scapula. Using this kind of technique, the patient is placed in a prone position with the affected arm hanging freely. A prospective cohort study published by Pishbin describes 112 consecutive anterior shoulder dislocations in 111 patients. The primary success rate was 87.5 % without any medications [8]. The total success rate after a recurrent attempt using medications was 97.3 %.
2.5 Nonoperative Treatment
Nonoperative treatment is still a well-accepted treatment option. The outcome correlates with the injury pattern, the patient’s age, and gender [9–11]. The outcome, especially the recurrence rate after nonoperative treatment, is significantly worse in patients younger than 30 years. Young men have a significantly higher risk than women of the same age. If a recurrent dislocation occurs, the cumulative risk can be estimated at 85 % within the first two post-traumatic years [10]. Hovelius reported his long-term results after nonoperative treatment of traumatic shoulder dislocations in patients younger than 40 years [12]. Forty-three percent had not re-dislocated over time. Again, there was a strong relationship to the patients’ age. In patients older than 30 years, 73 % suffer no further shoulder dislocation. Just 14 % achieved surgical stabilization for remaining instability. On the other hand, in patients between ages 12 and 22 years only 28 % were nonrecurrent, 20 % became stable over time, 12 % dislocated recurrently, and 40 % required a surgical stabilization.
The period of immobilization has no significant influence on recurrent instability [9, 13–15]. Neither Hovelius nor Kiviluoto were able to detect any significant benefit in patients younger than 30 years when treating patients nonoperatively in internal rotation for less than 1 week or longer than 3 weeks. Therefore, it is recommended to immobilize the shoulder no longer than 3 weeks, just for pain release in order to prevent posttraumatic shoulder stiffness.
Whether to immobilize the shoulder in internal rotation or in external rotation/abduction remains a matter of debate. Itoi first described beneficial effects in external rotation and abduction. This was confirmed by biomechanical, MRI, and arthroscopic observations [16–18]. The capsulolabral complex gets close contact to the anterior glenoid in abduction/external rotation. Thereby, the best position can be achieved in 30° abduction and 60° external rotation. In addition, several prospective clinical studies show a lower recurrence rate after treatment in this position. However, it is crucial to obtain compliant patients, who must wear a bulky orthesis. This might be the reason why other prospective randomized studies show heterogeneous results. While Itoi and Liavaag initially showed significantly better results in external rotation [11, 19], later reports failed to do so over time [20].
2.6 Surgical Treatment
The goal of surgical treatment is to achieve a stable shoulder and to restore the initial shoulder function. To do so, it is crucial to address the underlying pathology. As mentioned above, this is strongly age dependent. Arguments that must be considered include:
Occurrence of additional pathologies (i.e., intra- and/or periarticular fractures, SLAP lesions, rotator cuff tears, lesions of the rotator interval)
Size of the glenoidal and/or humeral bony defect
Location of capsular injuries (HAGL lesion)
These pathologies result in a higher likelihood of recurrence and/or impaired shoulder function and should indicate surgical treatment. In the absence of these pathologies, surgery becomes relative. The indication is based on the results of nonoperative treatment, which is age and gender dependent. It seems reasonable to recommend surgery in young males, regardless of their activity level, in order to lower the recurrence rate from approximately 80 % to approximately 5 %. However, in women older than 40 years a recommendation of surgery is less certain.
Even absolute contraindications for surgery diminish over time. There are patient-related factors that must be carefully considered because of the high risk of peri- and/or postoperative complications, including:
Co-morbidity of the patient (e.g., medically unstable patient)
Lack of compliance of the patient (e.g., chronic alcoholism, psychiatric diseases, uncontrolled seizure disorder)
Collagen disorders (e.g., Ehler–Danlos syndrome, Marfan syndrome)
Secondary gain or voluntary subluxation
2.7 Anterior Soft-Tissue Stabilization
Anterior soft-tissue stabilization addresses the anterior capsulolabral pathology. Indication for surgery is given if the amount of bone loss does not exceed a specific size. It is well accepted that a bony deficiency of approximately 25 % on the glenoidal side and approximately 30 % on the humeral side leads to a significantly higher rate of recurrence and should therefore be addressed. Otherwise, the Bankart repair is the classic procedure and is generally performed arthroscopically. From the evidence-based literature, arthroscopic Bankart repair may be considered as the new gold standard [21]. Bankart repair can be performed with or without an additional capsular shift. For fixation of the capsulolabral complex, several methods have been used, including staples, tacks, and transosseous sutures, but these have been accompanied by an unacceptably high rate of recurrence. Today, suture anchors or knotless anchors are well accepted [22]. Modern arthroscopic Bankart repairs are characterized by the following three criteria [21, 23]:
Use of at least three anchor systems
Addressing of capsular laxity by anterior shift of capsular plication
Treatment of concomitant intraarticular pathologies (e.g., lesions of the rotator interval, SLAP lesions)
2.8 Arthroscopic Bankart Repair
2.8.1 Positioning
Lateral decubitus
Beach chair
2.8.2 Typical Steps of the Procedure
Diagnostic arthroscopy
Creation of one optic (posterior) and two working portals (anterior and anterosuperior)
Mobilization of anterior capsulolabral complex until subscapularis becomes visible
If necessary, inferior capsular incision for later capsular shift
Debridement of anterior chondral border
Fixation of anterior capsulolabral complex using shuttle devices and suture anchors
2.8.3 Tips and Tricks
Changing the optic into the anterosuperior portal achieves better visualization of the anterior glenoid neck. This becomes useful for mobilization of the capsulolabral complex, especially for ALPSA lesions.
A deep anterior trans-subscapular portal might be useful to fix the inferior capsulolabral complex.
A modified intraarticular Caspari technique might be useful to perform a sufficient inferior capsular shift.
An arthroscopic Bankart repair is also useful to address bony Bankart fragments.
2.8.4 Results
With respect to the criteria of modern arthroscopic Bankart repair, equivalent rates of recurrence, better functional outcomes, and less morbidity may be achieved compared with open Bankart repair [21, 24]. The recurrence rate can be lowered to 0–6 % [21, 25–27]. Compared with open Bankart repair, several advantages are obvious [28–31]:
Lower perioperative morbidity
Less impaired postoperative shoulder function (i.e., less external rotation deficiency)
No lesions of subscapularis musculotendinous unit
Ability to address intraarticular pathologies
Less postoperative pain (Figs. 2.4 and 2.5)
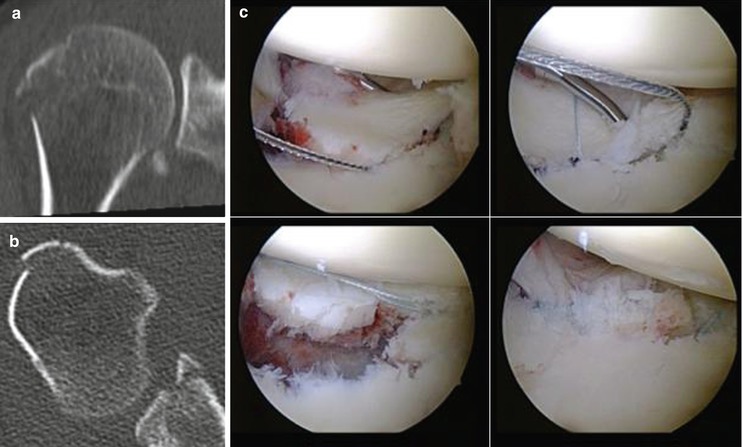
Fig. 2.4
Arthroscopic repair of a bony Bankart lesion. (a, b) Preoperative CT scan demonstrating an anterior bony Bankart lesion. (c) Stepwise arthroscopic fixation of the bony Bankart lesion using suture anchors
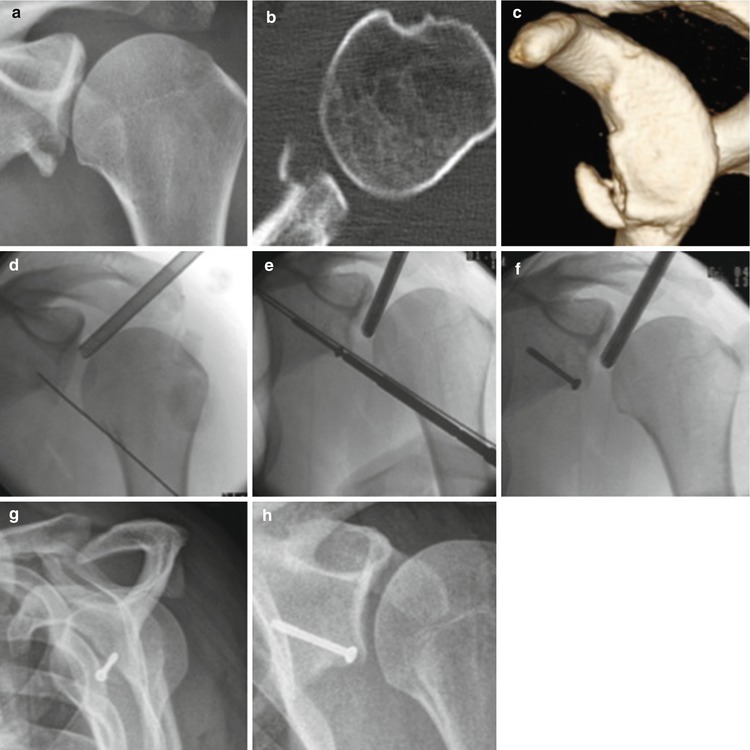
Fig. 2.5
Arthroscopic guided screw fixation of an anterior Bankart fracture. Preoperative diagnostic using (a) plain X-ray. (b) axial CT-scan. (c) 3D-volume rendering of CT scans. (d–f) Intraoperative X-rays demonstrating arthroscopic guided screw fixation. (g, h) 6 months postoperative controls showing anatomic healing of the anterior Bankart fracture
2.9 Bone Transfer
Indication for bone transfer is given if there is a relevant bone loss either at the glenoid and/or at the humerus. In order to judge the glenoidal bone loss, it is useful to evaluate parasagittal sectional images of the glenoid either in CT scan or MRI. A circle can cover the inferior glenoidal surface. In case of a bone loss, a segment of the circle is missing. The size of this defect can be estimated using several methods–the length of the segment’s base, its height, or the including angle. Using a digital image viewer the defect’s calculation becomes precise [32, 33].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








