Chapter 8 Posterior Tibialis Tendon Dysfunction
Introduction
Acute posterior tibialis tendon injury in the athlete is rare1,2 but must be considered in the differential diagnosis of a patient who presents primarily with tenderness, swelling, and pain over the medial ankle or plantar medial midfoot. Antecedent to the acute presentation, there often is a history of less severe prodromal symptoms more consistent with a chronic interstitial rupture with tendinosis. The chronic picture is seen more often in the middle-aged to elderly patient, athlete or not, that was especially popularized by the late Kenneth A. Johnson, MD,3–5 with whom I had the honor of fellowship training. Others,1,2,6–9 of course, also have contributed to a further understanding of the diagnosis and treatment of this condition.
Anatomy and Biomechanics
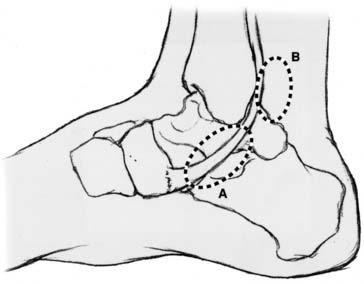
The posterior tibialis muscle is a resident of the deep posterior compartment of the leg, originating along the proximal one third of the tibia and intraosseous membrane. Distally, its tendon travels posterior, then inferior, through the medial malleolar groove, changing direction abruptly almost 90 degrees. The stout retinaculum of the long flexors prevents the tendon from subluxating over the medial malleolus.10 Because the posterior tibialis tendon is without a mesotenon, there is an area of relative hypovascularity from this acute turn at the medial malleolus to the medial navicular insertion. These factors of hypovascularity and the mechanical stress of an acute turn of the tendon as part of a strong, weight-bearing leg muscle (second only to the gastrocnemius) make the tendon predisposed to injury in this area.
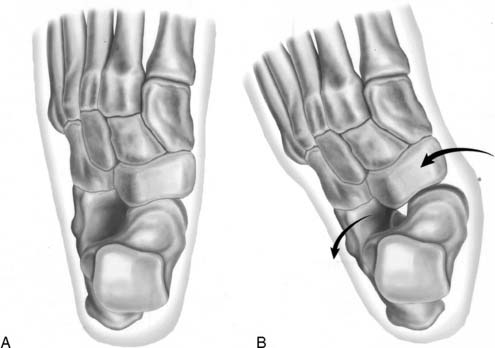
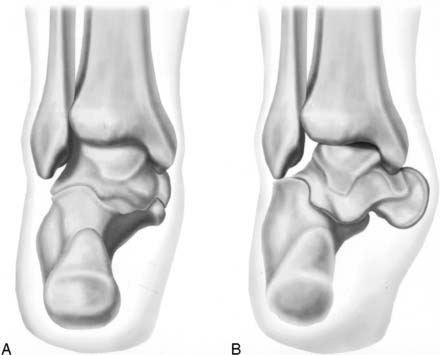
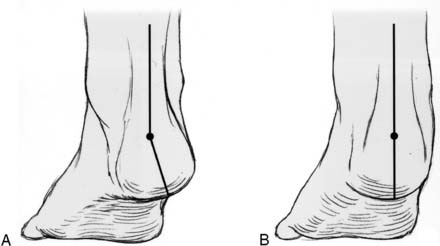
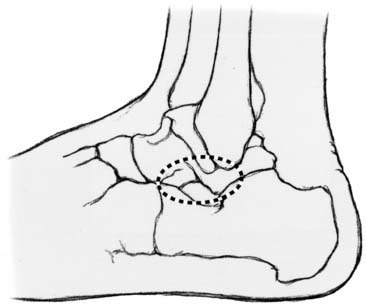
Because the posterior tibial tendon travels posterior to the axis of the ankle and medial to the axis of the subtalar joint, it serves as an ankle plantarflexor and foot invertor via the transverse tarsal joint (talonavicular and calcaneocuboid joints).11 The tendon also has multiple slip attachments to the capsule of the naviculocuneiform joint, all three of the cuneiforms, the cuboid, and their respective metatarsal bases in the plantar arch.4,12 The posterior tibialis tendon therefore is primarily a midfoot invertor and dynamically supports and elevates the medial longitudinal arch. It also indirectly supports the hindfoot because of its medial malleolar pulley action and intimate relationship to the deep deltoid ligament, plantar medial talonavicular joint capsule, and spring ligament (calcaneonavicular ligament).13 With relatively little elongation because of rupture, the tendon becomes incompetent to support the medial longitudinal arch initially, resulting in the acquired adult flatfoot with forefoot pronation and abduction (Fig. 8-1). However, over time other ligamentous structures are affected, including the talonavicular joint capsule, deltoid ligament, and spring ligament. The stretching out or even frank rupture of these structures eventually leads to a valgus inclination of the hindfoot and external rotation of the calcaneus, also resulting in contracture of the Achilles tendon as it becomes a hindfoot everter11 (Fig. 8-2). Clinically, this may result in impinging pain and swelling in the subfibular or sinus tarsi area as the calcaneus abuts against the lateral malleolus. In very severe or neglected cases, a valgus tilt of the ankle may be seen as the deltoid ligament becomes incompetent.
Diagnosis
History and questions to be answered
Physical examination and questions to be answered
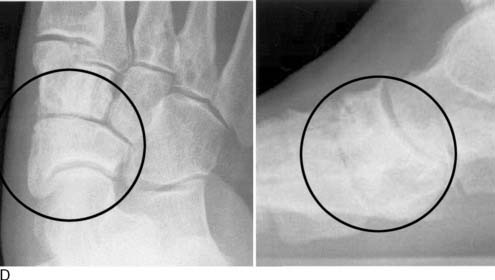
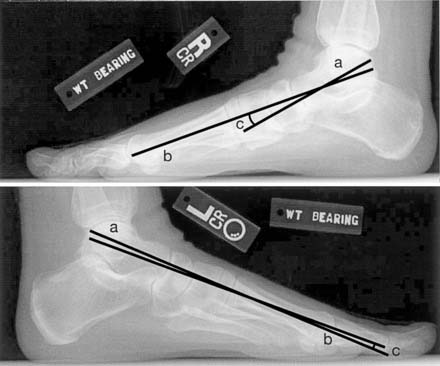
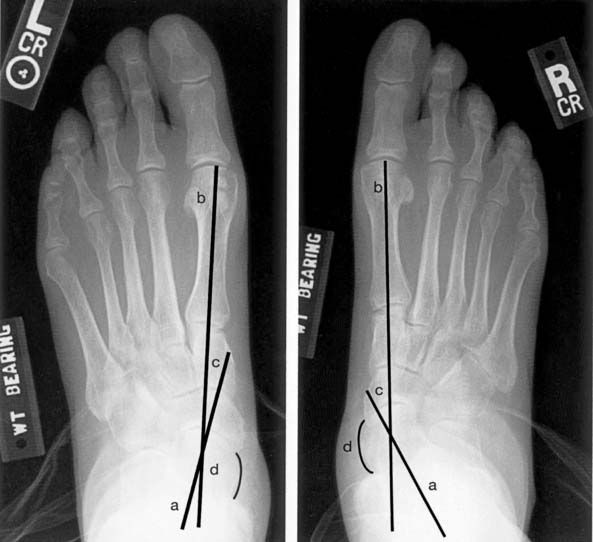
X-rays and questions to be answered
Ankle x-rays
Foot x-rays
Magnetic resonance imaging (MRI)
Although rarely necessary, if the history, physical examination, and x-rays fail to conclusively determine the diagnosis of a posterior tibialis tendon injury, or to confirm the diagnostician’s impression, then an MRI may be indicated.14,15 An MRI also is helpful to determine the extent of acute injury or chronic tendinosis and thus guide treatment, especially if surgery is planned, and may predict the postoperative clinical outcome.15 Finally, the MRI may help to determine other conditions that may mimic, be concomitant with, or even contribute to posterior tibialis tendon disease8,10,13,16,17 (Table 8-1). Perhaps of historical interest, others have proposed the diagnostic use of tenography7 or ultrasound,18 but their sensitivity is significantly less than that of a high-quality MRI.
Table 8-1 Differential diagnosis
| Medial ankle arthritis | Medial subtalar joint or medial column arthritis |
| Medial ankle instability with deltoid ligament rupture/laxity | Symptomatic accessory navicular with synchondrosis disruption |
| Medial malleolar or talar stress fracture | Medial navicular bony avulsion or stress fracture |
| Medial talar dome osteochondritis dissecans | Acute injury or tendinosis of the flexor hallucis longus or flexor digitorum longus tendons |
| Tarsal tunnel syndrome | Peri-insertional anterior tibialis tendon rupture or tendinosis |
| Tarsal coalition, especially in periadolescent athletes | Medial ankle or hindfoot/midfoot crystalline or autoimmune arthritis |
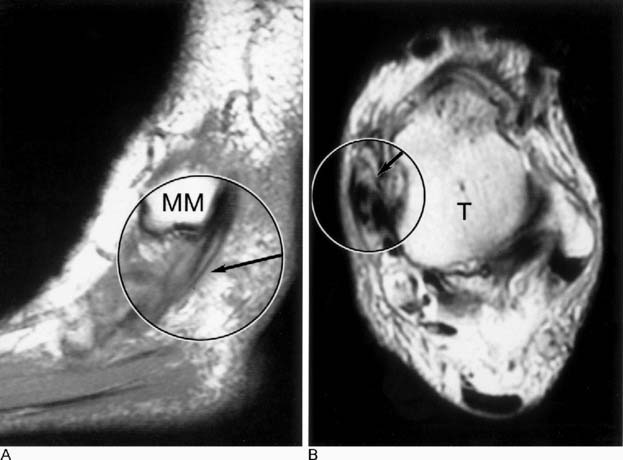
Generally, the MRI will reveal fibrous tendinotic longitudinal hypertrophy or bulbous enlargement of the tendon, sometimes with cystic or longitudinal voids (Fig. 8-10, A). Also, there usually is increased tenosynovial fluid within the sheath surrounding the tendon18,19 (Fig. 8-10, B). These findings usually are seen between the medial malleolus and navicular but also can extend proximally into the posterior medial malleolar area.
Disease Staging
Once the diagnosis is firmly established, the stage of posterior tibialis tendon disease, as popularized by Kenneth A. Johnson’s seminal work, is important to determine the proper course of treatment. Johnson initially described stages I to III,5 but a stage IV11,20 has more recently been described that involves a valgus inclination of the talus with degenerative arthritis of the ankle joint (Table 8-2). This is exceedingly rare in the active athlete and will not be elaborated upon beyond its mention.
| Stage I Peritendinitis and/or tendon degeneration (tendinosis) |
| No deformity |
| Stage II Tendon elongated/incompetent |
| Mild flexible deformity |
| Stage III Findings of Stage I and II |
| Moderate-to-severe deformity that may be rigid with possible subfibular or sinus tarsi impingement |
| Radiographic arthritic changes of triple joint complex and/or naviculocuneiform joints |
| (Stage IV, which involves a valgus talar tilt and early ankle joint degeneration, also has been described but probably is not applicable to this discussion, given its extreme rarity in the active athlete.) |