Chapter 5 Ankle and Midfoot Fractures and Dislocations
Introduction
Fractures and dislocations of the foot are among the most common injuries in the musculoskeletal system. With the recent explosion of interest in athletic activity, the foot and ankle have been exposed to a variety of new stresses. The disability and time away from sports resulting from these injuries warrant close attention to diagnosis and management (Figs. 5-1, 5-2, 5-3, and 5-4).
Clinical Diagnosis
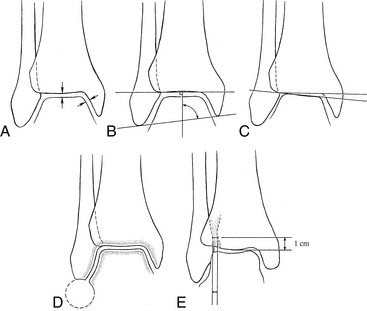
Standard radiographic examination of the ankle includes three views: AP, lateral, and mortise. From these, a remarkable amount of information may be obtained, not only about fracture patterns but, more importantly, about the relationship of the three bones that comprise the ankle mortise—tibia, fibula, and talus. Use of measurements of mortise width; medial or tibiofibular clear space; talocrural angle; “Shenton’s” line of the ankle (that space that demonstrates a mirrored congruity between the lateral talar wall and the corresponding curvature of the distal medial fibula); and talar tilt all are helpful in determining the subtle abnormalities of the ankle mortise (Fig. 5-5).
When in doubt, the clinician also may obtain contralateral views to determine that which constitutes normal anatomy for that particular patient, because there tends to be a high degree of variability in what is considered normal from patient to patient. Medial clear space is as viewed in anterior/posterior radiographs. It is the measure of distance between the medial talar wall and lateral portion of medial malleolus. Although this is a linear measure, it reflects a rotational (external) abnormality of the talus with respect to the tibia. Injury leading to abnormality of this relationship with measurements of less than 1 mm or greater than 4 mm has been shown to correlate with poor outcomes, including chronic pain, instability, and arthrosis.1–3
Syndesmotic space probably is the most confounding of all radiologic measures. Measurements should be performed to account for the space existing between the medial edge of the fibula and the lateral edge of the tibial incisura, determined at 1 cm proximal to the joint line to ensure reproducibility. Average distance should be less than 5 mm but may vary up to 6 mm in larger individuals. Another measure of syndesmotic integrity is the tibiofibular overlap. The distance between the medial fibula and the lateral edge of the anterior tibia should be 10 mm (see Fig. 5-5).
Treatment
Generic goals in the treatment of fractures and dislocations of the foot are as follows:
The evolution of treatment of the traumatized foot and ankle of the athlete has directed more attention to aggressive intervention than to “benign neglect.” Recognition of the fact that long periods of immobilization after trauma may lead to muscular atrophy, myostatic contracture, reduction of joint mobility, associated connective tissue proliferation leading to scarring, synovial adhesion, and cartilage degeneration has prompted a more aggressive approach to foot and ankle injuries, using appropriate surgical intervention to stabilize injuries and institute earlier range of motion and weight bearing when possible. These tenets provide for the ability to institute potential prevention against previously disabling factors such as disuse osteopenia, limb atrophy, proprioceptive losses, and chronic, persistent pain.4–8 Introduction of early range of motion, physical therapy modalities, appropriate splinting, and bracing, as opposed to casting, allows for the earlier restoration of function and avoidance of complications. The static accumulation of hematoma, fluid extravasation, and resultant articular and tendinous adhesions is far less with treatment that promotes earlier rehabilitation.4 This type treatment also helps to prevent disabling sequelae, such as arthrofibrosis and regional pain syndromes.7
Ankle Fractures
Medial fractures
Isolated medial fractures are unusual but not rare (Fig. 5-6, A and B). One must have suspicion for a “bimalleolar variant” in which lateral ligamentous injury has occurred in deference to bony injury. Generally, medial malleolar fractures indicate loss of stability of the ankle. Anywhere from 5% to 15% of untreated fractures may go on to nonunion (Fig. 5-7, A through D). Fracture patterns may vary from vertical, oblique, or horizontal, depending on the mechanism of injury. However, because of the risk of sequelae and potential for instability and abnormal mechanics, all but those that are nondisplaced should be repaired. Even those demonstrating minimal (<2 mm) displacement carry some advantage to stabilization, such as reliable fixation, early range of motion, lack of immobilization, and potentially early return to activity.
As evidenced by Ramsey and Hamilton,9 as well as Yablon,10 ankle stability is dependent on medial integrity. Michelson and others1,11–20 have shown that the talus will not shift abnormally with integrity of medial structures. Therefore attention should be directed to anatomic restoration of the medial ankle if it is disrupted. Repair may be performed percutaneously with cannulated screw fixation but should be reserved for absolutely anatomic reductions. Any incongruity, as evidenced by articular irregularity, necessitates open repair with restitution of the articular surfaces. I prefer open techniques because radiographs often may disguise an occult malreduction. Often, anterior/posterior reduction appears anatomic, but evaluation via live fluoroscopy will demonstrate some degree of articular step-off with internal rotation toward a mortise view. I prefer an open reversed J incision with attention to interposed periosteum and unrecognized comminution at the fracture site. Additionally, open reduction affords the opportunity to inspect the articular surface, which provides useful prognostic information. Fixation is dictated by fracture pattern. Most often, one or two partially threaded cancellous screws are sufficient; however, with a more vertical fracture pattern, several screws with washers or even a small one-third tubular anti-glide plate will be indicated.
Lateral fractures
Isolated lateral malleolar fractures present one of the most challenging management dilemmas in the realm of sports injuries. Associated syndesmosis widening or medial injury, bony or ligamentous, make the choice of treatment fairly simple and obvious.15,21,22,23 However, fibular fractures at any level without concomitant injury or significant radiographic displacement generate varied and controversial opinions as to what is considered appropriate intervention.
On one hand, arguments may be made that surgery is unnecessary because, even though the lateral stability is compromised, it is not completely diminished. Intact medial structures, specifically the malleolus and deltoid ligament, provide primary resistance to lateral talar translation, thus limiting or preventing abnormal ankle mechanics. Several studies support displacement, lateral or posterior, of up to 5 mm without significant compromise in clinical outcomes.22–2526 Physiologic loading studies of the normal and compromised ankle suggest that the medial structures are, in fact, most important for stability.1,10–19,26,27 It also has been shown by CT analysis that fibular displacement occurring as a result of an external rotation force with intact medial structures (Lauge-Hansen SER2) is the result of internal rotation of the proximal fragment.18 This implies that the distal fibula maintains its relationship with the mortise and that no functional incongruity is present (Fig. 5-8, A through D). Clinical studies have supported this notion, demonstrating good results with up to 30-year follow-up on nonoperative treatment of isolated lateral malleolar fractures.24,28–30
Alternatively, an argument may be made for repairing all but nondisplaced fibular fractures, the rationale being that even small increments of displacement may lead to fibular shortening or mortise widening.4,10 Early mechanical testing suggested that the lateral talar displacement of as little as 1 mm would significantly increase contact pressures in the tibiotalar joint, thus creating a potential predisposition to early arthritic changes.9 In addition, it was shown that the talus would routinely follow the displacement of the fibula, thus lending itself to anatomic malpositioning and subsequent abnormal loading stresses10 (Fig. 5-9, A through F).
However, these studies9,10 are some of the most often misquoted or misinterpreted in the literature. These analyses were performed in vitro and, as such, focused specifically on the relationship between the fibula and talus after eliminating all other attachments. There was no medial restraint to motion; thus, even though the results can be viewed as reliable and truthful, they bear limited clinical applicability because the contribution of the medial osseous and ligamentous structures was ignored. Appropriate interpretation of these studies suggests that abnormal ankle mechanics may be encountered when a fibular fracture exists in the face of medial deficiency. In these cases, operative treatment should be used.15 However, these studies fail to speak to the long-term, clinical consequences of a truly isolated lateral malleolar fracture.
Controversy persists surrounding the process of decision making. Despite evidence to the contrary, many surgeons perform, and athletes elect to undergo, repair of the injured lateral malleolus, presumably for fear of abnormal and untoward results of pathologic mechanics and to resume activity as quickly as possible. A large body of clinical evidence favoring this faction is the demonstrated lack of reliability of reproducible medial tenderness on clinical examination in disclosing the presence or absence of deltoid ligament injury.31 It is unclear as to what degree of deltoid injury in the face of the fibular fracture will allow for clinical instability.10 Therefore many surgeons ascribe to the philosophy that it is better to be aggressive, especially in someone whose livelihood may depend on the anatomic function of an ankle or lower extremity. Again, the perspective is anecdotal but reasonable. Surgical treatment often is pursued, as detailed later.
Should one embark on the surgical management of the isolated lateral malleolus fracture, operative principles of anatomic restoration and rigid fixation apply. The goal is to allow early mobilization and quick recovery. Debate still exists regarding the use of interfragmentary fixation combined with lateral buttress plating versus posteriorly placed, anti-glide fixation. Lateral plating is technically easier, whereas posterior plating theoretically provides greater mechanical stability.32,33 Both seem to perform well clinically. No current consensus exists, and the method remains the preference and comfort level of the surgeon.
Bimalleolar/trimalleolar fractures
Little debate exists regarding treatment of bimalleolar/trimalleolar ankle fractures. In an athletic population, uniform agreement exists regarding the need for operative intervention21,22 (Fig. 5-10, A through D).
High fibular fractures associated with bimalleolar fracture patterns should be stabilized rigidly and anatomically. All injuries should be tested for syndesmotic stability, but especially those demonstrating a medial soft tissue injury. This test can be done by directly visualizing the syndesmotic ligaments while applying a laterally directed pull on the fibula with a towel clamp, reduction tool, or other grasping object. Any laxity in tibiofibular stability associated with a fibular fracture more than 3.5 to 4.0 cm from the joint should be stabilized with syndesmotic fixation11 (Fig. 5-11, A through D).
I prefer to use a 3.5-mm screw with three cortex fixation and a plate long enough to incorporate the screw proximally to the distal-most hole (see Fig. 5-11, D). Routine screw removal is performed after 12 weeks on the basis of biomechanical evidence of abnormal ankle mechanics in the face of restricted talofibular motion.34 This reduces the risk of a free-standing screw hole as a stress riser and theoretically allows quicker, safer, and more reliable return to activity.
Trimalleolar fractures at least should have the medial and lateral components repaired. Fixation of the posterior fragment of tibia is performed on the basis of size of the segment and, more importantly, percentage of articular surface involved. Those with more than 25% to 30% of the joint involved in the fracture should undergo stabilization with at least one anterior to posterior screw (see Fig. 5-10, C and D).
Pediatric ankle fractures
Salter-Harris (S-H) fractures not involving the joint adhere to principles of all generic, pediatric fracture management protocols (Fig. 5-12). Closed anatomic reduction often is successful simply by reversing the mechanism of injury. Cast immobilization typically is effective for management, and bony remodeling usually compensates for any minor malalignments. Immobilization usually is required for 6 to 8 weeks, at which point gradual weight bearing and range of motion may be advanced as tolerated. Any articular incongruity necessitates open management (Fig. 5-13, A and B).
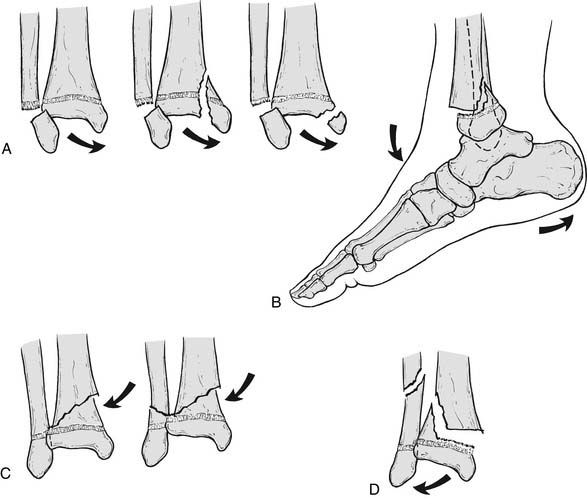
Figure 5-12 Dias, Tachdjian modification of Salter-Harris’ classification of ankle fractures in the immature skeleton.
From Green NE, Swiontkowski MF: Skeletal trauma in children, Philadelphia, 2002, WB Saunders.
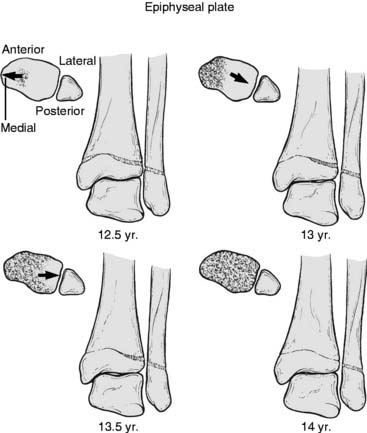
Complexity increases in the diagnosis and management of the adolescent variants of the Tillaux (S-H III) and triplane (S-H IV) fractures. These typically occur in the 12- to 14-year age range as the medial tibial physis begins to close, creating an irregular stress distribution and resistance to forces applied across the ankle (Fig. 5-14).
Tillaux and triplane fractures are considered adult, and issues regarding treatment should be viewed as such (Fig. 5-15). The focus of treatment should be based on congruity of articular reduction because the complications surrounding these injuries arise from nonanatomic incongruous relationships, leading to early degenerative changes rather than the more popular but erroneous presumption of growth arrest. Abnormalities or asymmetry in growth actually are rare and not terribly consequential in these scenarios.
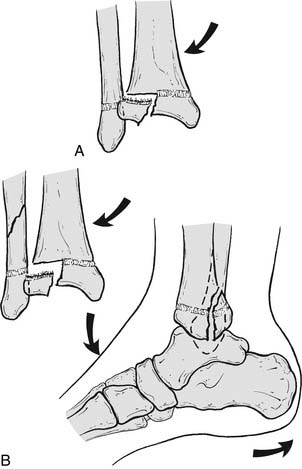
Figure 5-15 (A and B) Tillaux and triplane ankle fracture variants in the adolescent athlete.
From Green NE, Swiontkowski MF: Skeletal trauma in children, Philadelphia, 2002, WB Saunders.
Lateral Process Talar Fractures
Fractures of the lateral process of the talus previously have been considered an uncommon injury. Historically, this injury was thought to occur as the result of high-energy trauma and would result from a peritalar dislocation that caused avulsion of the subtalar ligamentous attachments on loading. More recently, however, this injury has gained notoriety because of its strong predilection for presentation after snowboarding injuries. Before the advent of this relatively new winter sport, reports were infrequent. However, with the explosion of attention to this activity by a predominantly young, risk-taking population, the incidence and recognition have risen dramatically—so much so that this injury has been deemed by some as the “snowboarder’s ankle.”35,36 One review demonstrates 74 lateral process fractures of the talus that occurred as the result specifically of snowboarding, accounting for 2.3% of all snowboard injuries. This is, to date, the largest series reported.36
Lateral process fractures often are missed, commonly masquerading as chronic ankle sprains. It is easy to understand why this happens because of the relative anatomic proximity of this injury to the anterior talofibular ligament, as well as the lack of reliability of reproducible evidence of fracture on standard radiographic studies. Early diagnosis and treatment, however, are important because studies have suggested that late recognition and failure to implement treatment routinely lead to poor outcomes, such as chronic pain, stiffness, instability, and arthritis.37–44
Traditionally, lateral process fractures were purported to arise from a sudden dorsiflexion inversion force on a fixed foot. However, mechanical loading studies have demonstrated that an acute external rotation or shear force is a key element in reproducing this fracture pattern in a cadaveric model.35
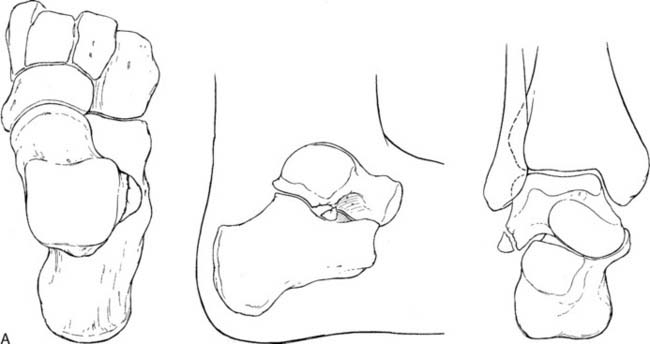
Hawkins39 has classified these fractures into three subcategories (Fig. 5-16). Type I is a simple fracture of the lateral process extending from the tibiofibular articulation down to the posterior talocalcaneal articular surface of the subtalar joint, with or without displacement of the fragment. Type II fractures involve comminution of the fibular and posterior calcaneal articular surfaces, as well as the lateral process. Type III is an avulsion or chip fracture off the anterior and inferior part of the posterior articular processes of the talus. Another classification system has been proposed by Fjeldborg,38 who described stages of injury with type I fissuring, type II lateral process fracture with displacement, and type III lateral process fracture with subtalar dislocation. Diagnostically, this fracture pattern presents a dilemma, and a high index of suspicion is needed by the clinician. Injury pattern reports by the patient often are unreliable and inaccurate. Physical examination findings often are similar to those found with an acute, severe ankle sprain with tenderness just anterior and inferior to the tip of the fibula, along with swelling and ecchymosis.
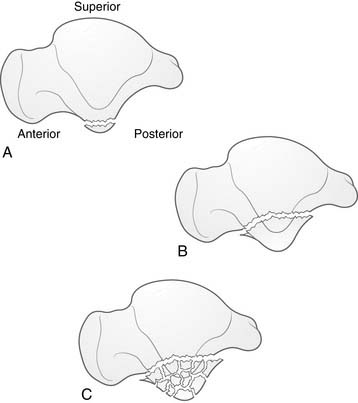
Figure 5-16 (A through C) Hawkins classification of lateral talar process fractures.
From: Boon AJ, Smith J, Zobitz ME, Amrami KM, et al: Am J Sports Med, 29(3):333, 2001.
Radiographs sometimes are helpful when large fragments or significant comminution are present but, again, are not reproducibly diagnostic because of the irregular anatomy and overlap of joints in this area.37,45 Special radiographic views have been proposed to help elucidate these fractures, including a 20-degree internal rotation view with the foot in neutral dorsiflexion.46 Alternatively, Dimon37 has suggested that the ankle be placed in 45-degree internal rotation and the foot plantarflexed at 30 degrees to show the posterior facet in profile. If the diagnosis is entertained, the best and most reliable study remains CT scanning. This not only provides the examiner with diagnostic evidence but also demonstrates the degree of displacement and comminution of fragments. Because of the poor outcomes obtained, all fractures must be sought and treated aggressively. Nondisplaced fractures should not be ignored but immobilized in a cast for 6 to 8 weeks with no weight bearing and then reevaluated at that time for bony union. Failure to aggressively treat larger displaced fracture fragments or comminuted fractures may and often does result in malunion, nonunion, heterotopic overgrowth, subtalar instability, and, ultimately, disabling arthritis.39,40,42,43,47–53 Late symptoms have been shown often to not respond to excision of the offending fragments.37,47,51
Treatment is fracture type dependent. Large displaced fractures are managed with anatomic restoration of the articular surface with internal fixation (Fig. 5-17, A through E). These often are large enough to accept at least one small fragment screw for fixation (2.7 or 3.0 mm usually will suffice). This most often can be done through a typical Ollier approach to the sinus tarsi and subtalar joint region. Comminuted fracture patterns are more ominous and carry a more unpredictable outcome. These often are refractory to repair and necessitate excision for all fragments. This at least removes any potentially abrasive surfaces and areas of future impingement. If repaired, early range of motion, focusing on inversion/eversion, will promote restoration of subtalar mechanics.
Sequelae of untreated or missed fractures are well documented. Malunion, nonunion, instability, overgrowth, and/or arthritis of the subtalar joint can be debilitating. Missed fractures that present late often are refractory to repair or remove fragments and will necessitate subtalar arthrodesis.37,47,51 Therefore it is critical that awareness of this injury pattern remains prevalent and a high index of suspicion be maintained for any patient presenting with atypical or persistently painful ankle sprains.35,36,47