Chapter 1 Assessment and Treatment of the Elite Athlete: Helpful Hints and Pertinent Pearls
#2 “Conservative Treatment was Exhausted” may Mean Only That the Athlete and Medical Team were Exhausted
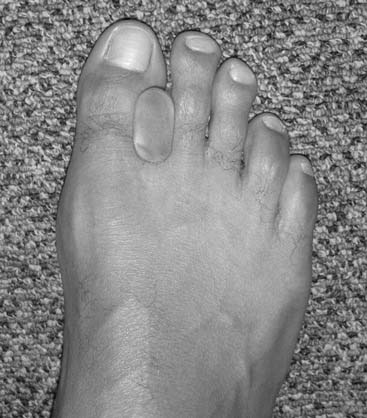
A Major League Baseball player presented with a chronic, overuse strain of his left great toe. He was a left-handed pitcher, and the left great toe was being subluxed into a lateral valgus position during push-off. The problem was diagnosed as a form of a turf-toe, more specifically a sprain of the medial sesamoidal phalangeal ligament and the medial head of the flexor hallucis brevis tendon. After talking to the trainer, agent, team doctor, and orthotist, we designed and custom made a spacer to fit between the great toe and the second toe. After a slow start to the season and requisite reassurance, the pitcher won 22 games using a simple device (Fig. 1-1).
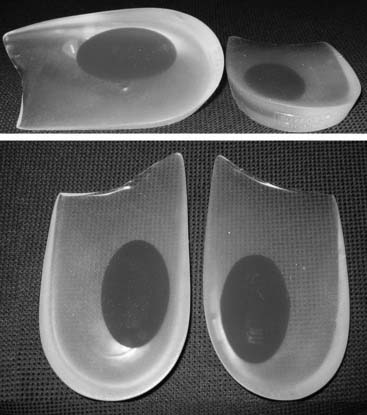
Another Major League Baseball player had ankle and hindfoot symptoms that were felt to limit his hitting. The ankle and hindfoot examination was unremarkable, with good stability, alignment, and strength. An examination of the whole musculoskeletal system brought to light an obvious genu varus, which resulted in varus of the ankle and the subtalar joint. When watching him simulate his swing, we noted that his ankle would subtly invert. By placing an off-the-shelf lateral wedge into the shoe, the player was able to get a better stance and more stability while batting and was able to increase his batting average significantly, winning the major league batting title (Fig. 1-2).
A professional quarterback asked for the opinion of three foot and ankle subspecialists. His ruptured Achilles tendon had been repaired one season before the examination. The repair had stretched out and did not allow adequate push-off. After careful discussion by the three orthopaedists who saw the quarterback simultaneously, it was decided to treat the elongated and weak tendon conservatively with an ankle-foot orthosis (AFO). This AFO was made with a plantar assist by using an anterior tibial stop for the AFO (Fig. 1-3). The Hall of Fame quarter back played three more seasons with a similar brace and never had additional surgery to the Achilles tendon.
A top-level and highly paid National Basketball Association (NBA) star sustained within 1 year three sequential injuries to his Achilles tendon that were diagnosed as partial tears. Following each injury, addressed by brief bouts of conservative treatment (physical therapy [PT], nonsteroidal anti-inflammatory drugs [NSAIDs], and rest), he was aggressively encouraged to continue to play despite persistent pain, swelling, and dysfunction. His third injury during the playoffs was the most incapacitating, both physically and emotionally. He lost faith in his doctors, whom he felt had allowed him to be reinjured by trivializing his trauma as insignificant. Much to the frustration of the team management, doctors, and fans, he decided to wait for complete resolution of the swelling, pain, and weakness before resuming play and missed numerous games. Further opinions were sought to bring the situation to resolution. The nonsurgical solution that we initiated satisfied all parties and permitted return with protection. A flexible plastic molded poster shell AFO, fabricated for each game (to avoid sudden and potentially catastrophic fatigue failure of the device), reduced the strain on the Achilles tendon while allowing somewhat restricted and controlled mobility. With the device, he returned to play after a 6-month hiatus and experienced progressive restoration of confidence while the injury continued to heal (Fig. 1-4).
#3 Conservative Care may not Conserve Resources
An example of the economic impact of the conservative option is provided. A 2-mm, displaced supination-eversion II fibular fracture occurred in a top-level National Hockey League player immediately preseason (Fig. 1-5, A through C). He had no deltoid or syndesmotic tenderness. There were concerns about potential hardware prominence interfering with the skate if an open reduction internal fixation (ORIF) were performed. This would delay return to play until after the hardware was removed. Given the nature of this injury to heal quickly and uneventfully, it was decided to treat the ankle fracture without surgery. The ankle was placed in a cast and the player was kept nonweight bearing for 6 weeks, then given a removable, off-the-shelf, boot brace. He resumed conditioning and ankle strengthening progressively with low-impact activity and then subsequently began skating. At 3 months, he still had tenderness, focal edema, and warmth, and could not skate aggressively or confidently enough to perform choppy sprints or to make quick stops and precision turns. He also was concerned about getting checked and sustaining a complete fracture. The x-ray and computed tomography (CT) scan (Fig. 1-5, D) performed at 3 months showed approximately 20% healing along the proximal posterior aspect. All parties were frustrated, and the team suffered without his talent. Treatments discussed included operative and nonoperative modalities. Among all parties—trainers, manager, team doctor, and the patient—it was agreed that we perform shock wave treatment of the delayed union with the Sonocur extracorporeal machine (which requires no local or general anesthetic), begin an EBI bone stimulator (EBI, Parsippany, NJ), and fabricate a custom-molded, plastic AFO that could be worn in a sneaker. The patient continued to advance in his low-impact skating and nonskating workout, using the brace and bone stimulator when not conditioning. By two additional months, the fracture had progressed to 60% healing and the symptoms had abated to allow return to aggressive skating during the playoffs (Fig. 1-5, E and F).
#5 Think About the Nerves
The anterior tarsal tunnel syndrome also is fascinating because the deep peroneal nerve may be irritated for several reasons. It can be compressed because of a functional instability of the ankle or the talonavicular joint. The treatment includes a minimal release by cutting the inferior edge of the retinaculum and then carefully removing dorsal bone from the talus or navicular bone (Fig. 1-6). The lateral branch of the deep peroneal nerve may be compressed by the fascia of the extensor brevis muscle, causing a sinus tarsi pain. This is an often-overlooked cause of the sinus tarsi syndrome. In this situation, the nerve should be released where it is focally tender, typically dorsal and medial to the sinus tarsi itself. The fascia of the extensor brevis muscle can be the causative structure, but the physician always must evaluate for ankle instability, as well. We do not recommend transecting this nerve branch as a means of reducing the pain.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree