Chapter 58 Posterior Cruciate Ligament Reconstruction
Remnant-Preserving Technique Through the Posteromedial Portal
The posterior cruciate ligament (PCL) is the strongest ligament in the knee and provides primary restraint to tibial posterior translation. Although the anatomy and biomechanics of the PCL have been examined in detail, controversy continues regarding the optimal treatment for PCL injuries. If surgical reconstruction is elected, the goals of surgery are to replicate the anatomy and biomechanics of the native PCL. Various surgical options are currently available for PCL reconstruction: the transtibial or inlay technique, single- or double-bundle reconstruction, and the one- or two-incision technique.22 Surgeons observe preserved continuity of the attenuated PCL in most PCL-insufficient patients.1,4,14 However, many surgeons have lost sight of the importance of these remaining fibers and surrounding structures. In conventional PCL reconstruction, the surgeon generally removes the residual stump of the PCL to facilitate visualization and technical performance. In fact, ligaments around the joints contain mechanoreceptors that are involved in providing the central nervous system with information about joint position and movement.15 The cruciate ligaments have recently attracted interest and have been studied not only as mechanical and structural stabilizers, but also as sensory structures.7,9,10,15 In addition, it has been suggested that the meniscofemoral ligaments (MFLs) contribute significantly to the cross-sectional area of the PCL complex and act as secondary restraints to tibial posterior translation.3,24
Scientific Rationale
Mechanoreceptors in the Posterior Cruciate Ligament
The presence of mechanoreceptors in the cruciate ligaments has led surgeons to suppose that these receptors influence the motor function of the knee joint. Several studies on anterior cruciate ligament (ACL) reconstruction revealed that success of surgery depends not only on the stability of the reconstructed ligament, but also on the quality of proprioception.13,21,27 Unfortunately, in comparison with the ACL, very little research has been carried out exclusively on PCL receptors and proprioception. Franchi et al8 found that the PCL possesses a neural network, and that mechanoreceptors occupy 1% of the total area of the ligament in histologic study. Afferents from these mechanoreceptors such as Ruffini endings, Ruffini corpuscles of the Golgi tendon organ-like type, and Pacinian corpuscles are thought to be involved in the control of proprioception.5,8,31 Loss of proprioception after ligament injury leads to changes in gait pattern, muscle strength, and timing of muscle activation, which may inhibit protective reflexes and result in degenerative changes.10
Mechanoreceptors on the Remnant Fibers
The PCL is known to have better synovial coverage, blood circulation, and healing potential than the ACL.29,30 Arthroscopic examination of the PCL-insufficient knee usually demonstrates well-maintained continuity of the PCL, even though it might be attenuated.1,4,14 However, no histologic reports have indicated whether the remnant of the ruptured PCL contains mechanoreceptors. Some studies have revealed the presence of mechanoreceptors even 3 years after ACL injury,9 and reproducible cortical somatosensory-evoked potentials induced by electrical stimulation were detected in patients with an ACL remnant bridging the femur and tibia or adherent to the PCL.26 In this respect, the importance of the remnant of the PCL as a proprioceptive organ can be considered similar to that of the ACL.
Functions and Anatomy of the Meniscofemoral Ligaments
The MFLs are composed of the ligament of Humphrey (anterior) and the ligament of Wrisberg (posterior), which originate from the posterior horn of the lateral meniscus and insert on the lateral aspect of the medial femoral condyle. The anterior MFL passes anterior to the PCL and attaches adjacent to the femoral condylar articular cartilage, indenting the attachment of the anterolateral fibers of the PCL.6 The posterior MFL passes posterior to the PCL and attaches proximally, close to the roof of the intercondylar notch.2 Studies investigating the prevalence of MFLs have shown that 82% to 93% of all knees have at least one MFL, and 26% to 50% possess both.3,24 The mean strength of the MFLs is approximately 300 N, which is mechanically equivalent to that of the posteromedial bundle of the PCL.3 Nagasaki et al24 reported that the cross-sectional area of MFLs accounted for 17.2% of the area of the PCL proper. Regarding a functional role in knee stability and protection, the slanting arrangement of the MFLs from the posterior horn of the meniscus up to the femoral intercondylar notch can help to withstand a tibial posterior drawer.11 Amis et al2 indicated that the MFLs contributed 28% of the resistance to posterior drawer in the intact knee at 90 degrees flexion; this contribution rose to 70% in the PCL-deficient knee. Moran et al23 showed that MFLs allowed the posterior horn of the lateral meniscus to be effectively restrained relative to the femur. In some PCL-insufficient knees, where the distal attachment of the MFLs is seen at the relatively mobile lateral meniscus, it is possible for the MFLs to remain intact despite rupture of the PCL.3 Consequently, preservation of the MFLs may promote stabilization of knees that require PCL reconstruction.
Surgical Technique
Arthroscopic Portals
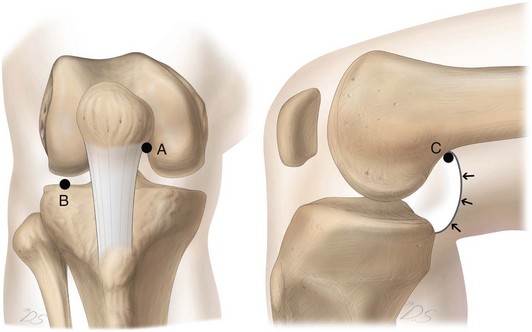
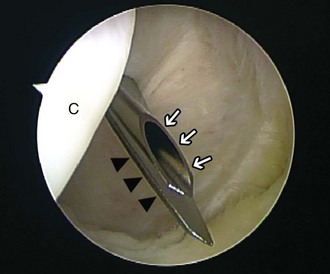
For more convenient reconstruction of the PCL, three unique portals are used: a high medial parapatellar portal, a far anterolateral portal, and a high posteromedial portal (Fig. 58-1). The high medial parapatellar portal is made first at the highest position on the medial parapatellar line, which is just off the medial edge of the patella tendon and the inferior border of the patella. This portal is more proximal than the conventional anteromedial portal and facilitates access to the attachment area of the PCL through the intercondylar notch, as well as to the posterior capsule, with a 30 degree arthroscope. The far anterolateral portal is made just above the joint line and 5 mm anterior to the lateral femoral condyle. Then, under direct visualization through the high medial parapatellar portal, the high posteromedial portal is made. A spinal needle is inserted through the posteromedial side of the knee as high as possible and just beside the medial gastrocnemius, aiming for the tibial footprint of the PCL. A scalpel is inserted alongside the entry point of the needle and is run parallel with the needle. The back of the scalpel blade should face the femoral condyle to avoid damage to articular cartilage (Fig. 58-2). Through this portal, the tibial attachment of the PCL can be accessed directly while viewing through the intercondylar notch. Furthermore, the high posteromedial portal facilitates excellent visualization of the tibial stump and the posterior capsule as an additional viewing portal.
Tibial Tunnel Preparation
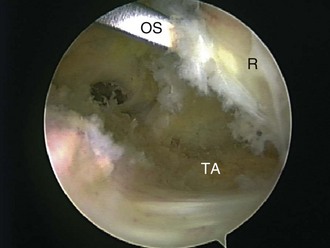
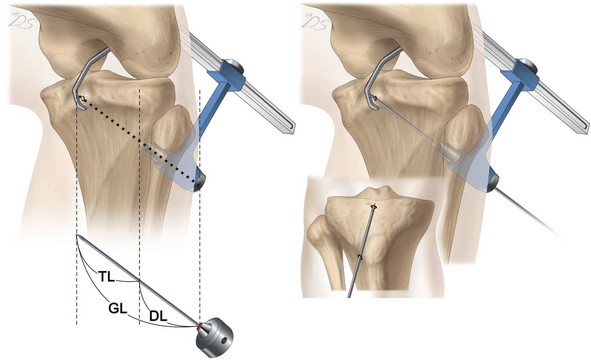
In preparing the tibial footprint of the PCL, the remnant is laterally peeled from the tibial attachment with a narrow osteotome (Fig. 58-3). To create a tibial tunnel, a PCL guide is inserted through the high medial parapatellar portal and is passed through the intercondylar notch while viewing through the high posteromedial portal. The PCL guide is located about 1.5 cm below the articular surface and just lateral to the midline on the fossa for the PCL. A 3- to 4-cm longitudinal skin incision is made just lateral to the tibial tuberosity. The tibialis anterior muscle is stripped off and retracted laterally, exposing the starting point of the tibial tunnel 2 cm posterolateral from the anterior tibial crest. Using calibrations on the PCL guide, the distance from the anterolateral cortex of the tibia to the tip of the guide in the fossa for the PCL is accurately measured. The same length as measured on the guide system is marked on the guide pin to prevent past-point drilling (Fig. 58-4). Placement of the guide pin at the ideal site of the PCL footprint is confirmed by visualization through the high posteromedial portal. To enhance visualization during the following procedures, the previously stripped PCL stump and the posterior capsule are pushed back with the arm of the PCL guide. The tibial tunnel is reamed incrementally with a 6- to 11-mm-diameter cannulated reamer. The final tibial tunnel reaming is completed manually to avoid damage to neurovascular structures (Fig. 58-5). Then, chamfering of the upper sharp edge of the aperture is performed using the half-round–shaped rasp to reduce abrasion of the graft.

Figure 58-5 The final tibial tunnel reaming is completed manually to avoid damage to neurovascular structures.
Author’s Tips
In the tibial attachment of the native PCL, the anterolateral fibers are on the anterior (deep) aspect, and the posteromedial fibers are posterior (superficial). Because of this arrangement, when a surgeon performs a single-bundle PCL reconstruction with reproduction of the anterolateral fibers, the graft should be brought up from the tibia underneath (anterior to) the remnant of the PCL.3 In this respect, lateral peeling of the remnant from the tibial attachment with the osteotome enables not only preservation of the remnant but also restoration of the anatomic arrangement. In addition, as described earlier, we are in favor of anterolateral tibial tunnel drilling for PCL reconstruction. Concentration of stress from the acutely angled graft at the proximal tibial tunnel margin can cause friction and stretching, followed by failure of the graft during motion against the abrasive edge, in the early postoperative incorporation period. A biomechanical laboratory study showed that the lateral approach for tibial tunnel drilling had the lowest values for maximum shear stress.19 Moreover, in a cadaveric experiment using pressure films, the lateral tunnel showed a lower reactive force than that of the medial tunnel.19 A recent clinical study in our institute supports the superiority of this lateral approach. When cases of anteromedial tibial tunnel and anterolateral tibial tunnel were compared, side-to-side differences in posterior tibial translation were significantly less with the anterolateral tibial tunnel technique (2.87 ± 1.25 mm) than with the anteromedial tibial tunnel technique (3.98 ± 1.27 mm).16 In addition to decreased stress concentration, technical advantages of the anterolateral tibial tunnel direction include easy inspection of the inside of the tibial tunnel aperture through the posteromedial portal view, making it more convenient to chamfer the abrasive edge (Fig. 58-6), and shorter tibial tunnel length with less surgical damage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree