Fig. 19.1
Preoperative radiographs in a 12-year-old boy. The diagnosis in this patient is a right knee posterior-cruciate-ligament-based multiple-ligament-injured knee with posterior cruciate ligament tear, posteromedial instability type A, and posterolateral instability type B in a patient with open growth plates
KT 1000 arthrometer testing revealed the following side-to-side difference measurements: PCL screen at 90° of knee flexion 6 mm, corrected posterior measurement at 70° of knee flexion 6 mm, corrected anterior measurement at 70° of knee flexion 4 mm, and the 30-pound anterior displacement measurement at 30° of knee flexion was 1 mm. Side-to-side difference on stress radiography at 90° of knee flexion with a posterior displacement force applied to the tibial tubercle area of the proximal tibia using the Telos device comparing the involved to the normal knee was 10 mm (Fig. 19.2).
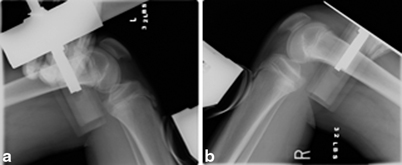
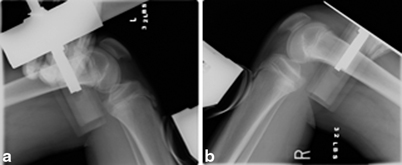
Fig. 19.2
Preoperative stress radiography with a posterior directed force applied to the proximal tibia of the normal uninjured knee (a) and the PCL, posterolateral, posteromedial injured knee (b). These stress radiographs demonstrate increased posterior translation at approximately 90° of knee flexion in the injured knee compared to the normal knee. Side-to-side difference on stress radiography at 90° of knee flexion with a posterior displacement force applied to the tibial tubercle area of the proximal tibia using the Telos device comparing the involved to the normal knee was 10 mm increased posterior tibial translation compared to the normal knee. PCL posterior cruciate ligament
Preoperative testing with three knee ligament rating scales revealed the following: Hospital for Special Surgery score was 42/100, Lysholm score was 44/100, and the Tegner activity score was 3 (pre-injury, the patient was level 7).
The diagnosis in this patient is a right knee subacute PCL-based multiple-ligament-injured knee with PCL tear, posteromedial instability type A, and posterolateral instability type B in a patient with open growth plates. The decision was made to proceed with arthroscopic single-bundle transtibial PCL reconstruction using fresh-frozen Achilles tendon allograft without bone plug combined with a fibular-head-based figure-of-eight posterolateral reconstruction using fresh-frozen semitendinosus allograft. The PCL reconstruction femoral tunnel crossed the distal femoral physis, and the PCL tibial tunnel was positioned distal to the tibial physis. Cortical suspensory fixation with two stacked polyethylene ligament fixation buttons were used on the femoral side, and a bioabsorbable interference screw and bicortical screw and spiked ligament washer were used on the tibial side fixation. No fixation device crossed the growth plates, and there were no bone plugs on the Achilles tendon allograft tissue, so no bone plug crossed the growth plate (Fig. 19.3).
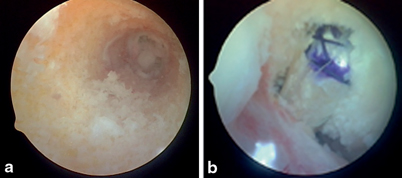
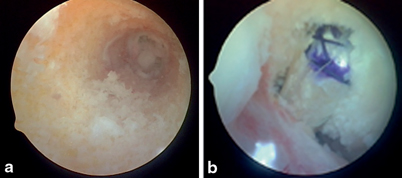
Fig. 19.3
The posterior cruciate ligament reconstruction femoral tunnel crossed the distal femoral physis (a), and the PCL tibial tunnel was positioned distal to the tibial physis. Cortical suspensory fixation with two stacked polyethylene ligament fixation buttons were used on the femoral side, and a bioabsorbable interference screw and bicortical screw and spiked ligament washer were used on the tibial side fixation. No fixation device crossed the growth plates, and there were no bone plugs on the Achilles tendon allograft tissue, so no bone plug crossed the growth plate (b). PCL posterior cruciate ligament
The posterolateral reconstruction was a fibular-head-based figure-of-eight reconstruction using a fresh-frozen semitendinosus allograft. The allograft was looped around the common biceps tendon at the fibular head and sewn there using permanent braided suture. The fibular collateral ligament component was passed medial to the iliotibial band, and the popliteofibular popliteus tendon component passed medial to the common biceps tendon and the iliotibial band. The allograft limbs were crossed in a figure-of-eight fashion with the fibular collateral component being lateral to the popliteus tendon component. The graft limbs were sewn into their respective anatomic femoral insertion sites with number 2 braided permanent sutures with a slight valgus applied to the knee to close the lateral compartment with the knee in approximately 90° of flexion. The allograft was then sewn to the deep capsular layers for additional reinforcement, and a posterolateral capsular shift was also performed. There were no drill holes through or around the lateral-side growth plates (Fig. 19.4).


Fig. 19.4
The posterolateral reconstruction was a fibular-head-based figure-of-eight reconstruction using a fresh-frozen semitendinosus allograft. The allograft was looped around the common biceps tendon at the fibular head and sewn there using permanent braided suture. The fibular collateral ligament component was passed medial to the iliotibial band, and the popliteofibular popliteus tendon component passed medial to the common biceps tendon and the iliotibial band. The allograft limbs were crossed in a figure-of-eight fashion with the fibular collateral component being lateral to the popliteus tendon component. The graft limbs were sewn into their respective anatomic femoral insertion sites with number 2 braided permanent sutures with a slight valgus applied to the knee to close the lateral compartment with the knee in approximately 90° of flexion. The allograft was then sewn to the deep capsular layers for additional reinforcement, and a posterolateral capsular shift was also performed. There were no drill holes through or around the lateral-side growth plates
The posteromedial reconstruction was performed using the posteromedial capsular shift technique (Fig. 19.5). This was an all suture posteromedial capsular advancement procedure performed with the knee in approximately 45° of flexion as described in Chap. 15. The PCL reconstruction, the posterolateral reconstruction, and the posteromedial reconstruction procedures were all protective of the growth plates. Postoperatively, the surgical knee was immobilized in a long leg brace locked in full extension, and was nonweight bearing with crutches. Prophylactic preoperative and postoperative antibiotics were utilized. Progressive weight bearing and the range of knee motion were gradually initiated according to our postoperative rehabilitation program detailed in Chap. 25.


Fig. 19.5
The posteromedial reconstruction was performed using the posteromedial capsular shift technique. This was an all suture posteromedial capsular advancement procedure performed with the knee in approximately 45° of flexion. A longitudinal incision is made just posterior to the posterior border of the superficial medial collateral ligament. Care is taken not to damage the medial meniscus during the capsular incision. Avulsed capsular structures are primarily repaired using suture anchors and number 2 permanent braided sutures. The interval between the posteromedial capsule and medial meniscus is developed. The posteromedial capsule is shifted in an anterior and superior direction. The medial meniscus is repaired to the new capsular position, and the shifted capsule is sewn into the medial collateral ligament using three number 2 ethibond permanent braided sutures in horizontal mattress fashion, and that suture line is reinforced using a running number 2 ethibond permanent braided suture
Six-year follow-up postoperative examination of the patient at the age of 19 reveals equal leg lengths, normal and symmetrical carrying angles, and normal gait during ambulation. Radiographs reveal closed distal femoral and proximal tibial physes that are symmetrical to the normal knee with no malalignment, no evidence of growth arrest, and no degenerative changes (Fig. 19.6). Physical examination of the surgical right knee compared to the normal left knee reveals the posterior drawer is negative, posteromedial and posterolateral drawer tests are negative, and the dial test is symmetrical at 30° and 90° of knee flexion . The Lachman test is negative, the pivot shift test is negative, and the surgical knee is stable to varus and valgus stress throughout the flexion extension arc. The hyperextension external rotation recurvatum and heel liftoff tests are symmetrical compared to the normal knee.


Fig. 19.6




Six-year follow-up postoperative examination of the patient at the age of 19 reveals equal leg lengths, normal and symmetrical carrying angles, and normal gait during ambulation. Radiographs reveal closed distal femoral and proximal tibial physes that are symmetrical to the normal knee with no malalignment, no evidence of growth arrest, and no degenerative changes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








