Fig. 17.1
The anatomy of the posterior medial corner including the hamstring tendon attachment (yellow), sMCL (bright green), fascial arm POL (light blue), central arm POL (mid-blue), capsular arm POL (dark blue), and semimembranosus tendon (dark Green). sMCL superficial medial collateral ligament, POL posterior oblique ligament
The anatomy of the medial structures of the knee has also been described from anterior to posterior, extending from the medial border of the patella to the medial edge of the PCL . The anterior third comprises the extensor retinaculum of the quadriceps femoris muscle. The middle third consists of the dMCL and the sMCL. The former is itself made up of meniscofemoral and meniscotibial fibers, and is separated from the sMCL by the MCL bursa (Fig. 17.2). The posterior third represents the posteromedial capsule and again there is some controversy as to what exactly this comprises. However, from previous biomechanical and anatomical studies, those structures that play a functional role include the posterior horn of the medial meniscus, the POL, semimembranosus tendon and insertions, meniscotibial ligaments, the oblique popliteal ligament, and the posteromedial capsule [1, 5, 12–14].
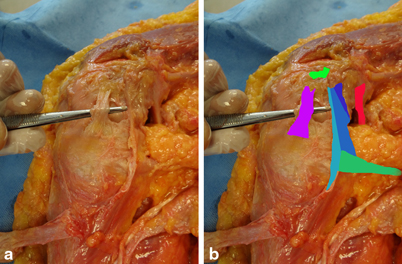
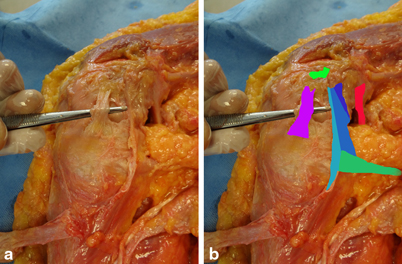
Fig. 17.2
The sMCL reflected to demonstrate the femoral foot print of the sMCL (bright green), dMCL (purple), fascial arm POL (light blue), central arm POL (mid-blue), capsular arm POL (dark blue), semimembranosus tendon (dark green), and the medial gastrocnemius tendon (red). sMCL superficial medial collateral ligament, dMCL deep medial collateral ligament, POL posterior oblique ligament
The PMC has been described as a synergistic muscle–ligament–meniscal unit with all of the structures working together to provide stability. The semimembranosus muscle has multiple attachments to the tibia and provides a dynamic component to the PMC. The anterior arm of the semimembranosus attaches to the tibia deep to the proximal attachment of the superficial MCL, whereas the direct arm attaches posterior to the medial tibial crest. In extension, it acts as a restraint to valgus and in flexion it restricts but also tightens the PMC via its attachments to POL and posterior capsule. The resulting posterior retraction of the posterior horn of the medial meniscus serves as a restraint against anterior tibial translation via the “chock block” effect [7].
Superficial Medial Collateral Ligament
The superficial medial collateral ligament consists of one femoral attachment and two tibial attachments. The femoral attachment is on average, 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. The proximal tibial attachment is primarily to soft tissue over the termination of the anterior arm of the semimembranosus tendon and is located at an average of 12.2 mm distal to the joint line. The distal tibial attachment of the sMCL is located just anterior to the posteromedial crest of the tibia at an average of 61.2 mm distal to the joint line. The two distinct tibial attachments have been reported to result in two distinct functioning divisions of the superficial medial collateral ligament [15].
Deep Medial Collateral Ligament
The deep medial collateral ligament comprises the thickened medial aspect of the joint capsule that is deep to the superficial medial collateral ligament. It is divided into meniscofemoral and meniscotibial components. The meniscofemoral portion has a slightly curved convex attachment, 12.6 mm distal and deep to the femoral attachment of the superficial medial collateral ligament. The meniscotibial portion, which is much shorter and thicker than the meniscofemoral portion, attaches just distal to the edge of the articular cartilage of the medial tibial plateau, 3.2 mm distal to the medial joint line [15].
Biomechanics
The PMC and the POL are biomechanically separate structures from the superficial MCL and play a role in restraint to valgus stress, internal/external rotation, posterior tibial translation (PTT), and anteromedial rotatory instability (AMRI).
Valgus Stress
The PMC is a primary stabilizer of the extended knee providing approximately one third of the restraint to valgus stress. However, with flexion, the PMC slackens, causing the superficial MCL to become the primary stabilizer to valgus stress across the remainder of the flexion–extension arc. At 0°, the PMC resisted 29 % valgus, 14 % at 30° and < 5 % at 90° [16].
Internal/External Rotation
The POL is a primary stabilizer for internal rotation at all knee flexion angles although the most load occurs in full extension. In biomechanical studies where the MCL has already been cut, sectioning the POL and capsule causes significant increases in internal and external rotation in all degrees of flexion.
The PMC is not a significant restraint to tibial internal rotation above 30° flexion but is the primary restraint near full extension. The fibers of PMC are slackened by tibial ER and therefore do not contribute to restraining this movement unlike the sMCL and dMCL [16].
Posterior Tibial Translation
The PMC is an important secondary restraint to PTT in the PCL -intact knee. It has been shown to resist 28 % of the posterior tibial load when the tibia was free to rotate, rising to 42 % when the tibia was internally rotated. However, the PMC becomes the primary restraint to PTT in the PCL-deficient knee.
Sectioning of the POL and posteromedial capsule in this setting has been shown to increase posterior tibial translation and this can be helpful for distinguishing between isolated and combined PCL injuries [7].
The effect on PTT is even more pronounced when the knee is in extension because POL fibers slacken with flexion. Weimann et al. reported that the application of valgus rotation with a force of 10 N m causes a significant increase in PTT of the knee with posteromedial instability. This suggests that the POL should be intact if there is no PTT in extension with valgus testing in the PCL -deficient knee. This finding may also be considered as a basis for the observation that isolated PCL injuries may not always cause functional disability and furthermore supports the clinical theory that untreated injuries to the POL may contribute to PCL graft failure [1].
Anteromedial Rotatory Instability
Injury to multiple structures on the medial side of the knee results in the phenomenon of AMRI which is defined as anterior subluxation and external rotation of the medial tibial plateau [7].
Mechanism of Injury
Clinical Examination
The hallmarks of clinical examination are detailed below.
Valgus Stress Testing
For an isolated superficial MCL injury, the greatest joint space opening occurs with the knee in 30° of flexion. Joint space opening with the knee fully extended indicates an injury to the capsule, the POL, or both [20]. Chahal et al. showed that in their series of knee dislocations, all those with grade III medial opening at 0 and 30° had complete tears of the sMCL as well as the POL. No patient with grade I opening had complete tears of POL or sMCL [2].
Posterior Drawer
In combined PCL –PMC injury, a posterior drawer test is performed with the knee flexed at 90° and the foot in neutral rotation and repeated with the foot 10° internally rotated. The PMC acts as a secondary stabilizer with an isolated PCL injury decreasing tibial translation when the foot is held in internal rotation, if intact. With combined PCL–PMC injury, there is increased translation during the posterior drawer when the tibia is internally rotated as these secondary stabilizers are no longer intact [7, 19].
Anterior Drawer and AMRI
AMRI is detected by performing the anterior drawer test while holding the tibia in external rotation. Any evidence of anterior subluxation of the medial tibial plateau during a valgus stress test with the knee in 30° of flexion might also indicate the presence of AMRI [7].
Imaging
Plain Radiographs
All patients should have plain radiographs taken in orthogonal planes to evaluate for fractures, avulsions, or a dislocation [21].
Stress radiograph s can be useful to assess the degree of medial opening and PTT. Garavaglia et al. reported that > 12 mm of posterior translation at 80° flexion was indicative of a combined PCL –PMC injury [22].
MRI
MRI is the imaging study of choice to evaluate the PMC and can elucidate injuries to SM, the POL, medial meniscocapsular structures, the OPL, and fractures/bone bruising. MRI should be performed prior to fixation of any coexisting periarticular fractures as metal artifact can significantly reduce the quality of imaging [2, 6].
Chahal et al. reported MR findings in 27 consecutive knee dislocations. It is interesting to note that they found evidence of injury to at least one structure in the posteromedial corner in 81 % (22/27) of knees. Of these, 64 % (14/22) had injury to the POL. The semimembranosus and its expansions were injured in 64 % (22/22) and injury to the MT ligament was identified in 50 % (11/22). Of particular note, 9/22 had injuries to the PHMM and of those 100 % had a tear of MT ligament and 67 % had a tear of the POL. They concluded that injuries to the PMC are in fact common with high-grade multiligament knee injuries [2].
A cadaveric study demonstrated that T1-weighted fat-saturated coronal- and coronal-oblique sequences acquired after the injection of intra-articular contrast demonstrated the best visualization of the POL and posteromedial capsule. However, the use of contrast studies is not common practice and noncontrast T1 axial images can provide good visualization of the MCL, POL, and the semimembranosus attachments [21].
It is important to look for evidence of injury to each structure within the PMC as involvement of any of these can disable the functional cascade of the posteromedial capsule [13]. However, Chahal et al. reported that isolated injuries to semimembranosus on MRI did not correlate with clinical medial knee instability [2].
Surgical Management
Immediate Management
The immediate management of knee dislocation is well described elsewhere. In brief, patients should be assessed with respect to standard trauma care principles and life-threatening injuries treated first. The hallmarks of clinical examination of the PCL –PMC injured knee are described above, but in the acute setting a neurological and vascular assessment of the limb is also mandatory. Provided that no emergent management is required (e.g., for open dislocation or vascular injury), the affected limb can be placed into a cricket pad splint while awaiting further imaging, assessment, and definitive management.
Nonoperative Treatment
Nonoperative management is not recommended for combined PCL– PMC injuries. Although low-grade MCL injuries heal predictably with nonsurgical treatment, as stated at the beginning of this chapter, it is important to distinguish these from PMC injuries [23]. This is necessary because PMC injury is associated with AMRI, excessive PTT and medial opening all of which may affect long-term viability of cruciate ligament reconstruction [1, 7, 19, 21, 23]. Furthermore, it is recognized that the nonoperative management of isolated PCL injury also causes a relative change in the kinematics of the medial compartment resulting in a characteristic pattern of arthrosis. It is therefore logical that the increased PTT associated with a PMC injury may exacerbate this progression to degenerative change though there is currently no clinical evidence to support this assumption.
Operative Treatment
There are no series describing the surgical management of PCL and PMC injuries alone but small numbers of cases have been included within larger multiligament knee injury series. A wide variety of surgical techniques have been described. In addition to reconstructing the PCL, these have included repair or reattachment of the posteromedial capsular structures, reconstructing the POL, or both the POL and the MCL [1].
Timing of Surgery
Currently, there is no evidence regarding the timing of surgery [20]. However, Tuman et al. recommend surgery within 2 weeks of the injury in order to minimize the formation of scar tissue, maintain tissue planes, and facilitate primary repair. In those patients with chronic injuries (defined as >3 weeks since the injury), primary repair is no longer possible due to abundant scar tissue and the focus of treatment becomes restoration of range of movement prior to elective surgery [24]. When planning the timing of surgery, it is important to note that multiligament injuries repaired acutely have less articular and medial meniscal damage than do those repaired more than 1 year after the injury [7].
PCL Surgery
The surgical technique for PCL repair or reconstruction is described elsewhere in the book. A variety of techniques exist and it is reasonable for surgeons to use the procedure they are most familiar with.
Arthroscopy
In addition to PCL reconstruction , arthroscopy may be used before the open procedure to evaluate intra-articular pathology and perform debridement/meniscal repair as indicated. However, care must be taken to avoid significant fluid extravasation. Other arthroscopic findings may include posterior capsular hemorrhage, pathologic medial ‘‘meniscus rise’’ (meniscus lift off from the tibia during abduction stress testing at 30° flexion) and the “arthroscopic spin sign” (excessive rotation of the tibia beneath the medial meniscus) [3].
Repair Versus Reconstruction of the PMC
There are no clinical studies directly comparing repair versus reconstruction of the PMC and some authors will use both techniques together, particularly in the acute setting. However, Stannard reported failure rates of 4 % (PMC reconstruction) and 20 % (PMC repair). On the basis of these results, Stannard recommended reconstruction of the MCL/PMC in patients who have sustained a knee dislocation and have medial instability [21, 25].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








