Posterior Ankle Arthroscopy and Tendoscopy
Mikel L. Reilingh
Peter A.J. de Leeuw
Maayke N. van Sterkenburg
C. Niek van Dijk
INTRODUCTION
Ankle arthroscopy has been developed and improved over the last 30 years. Nowadays, this minimal invasive technique is increasingly used for dealing with a wide range of ankle pathologies. In 1931, Burman was the first orthopaedic surgeon attempting ankle joint arthroscopy in vivo and concluded that the ankle joint was unsuitable for arthroscopy, because of its narrow interarticular access (1). Technical improvements, such as smaller diameter arthroscopes and joint distraction methods, made it possible for Watanabe in 1972 to report on a series of 28 ankle arthroscopies.
Van Dijk et al. (3) were the first to describe endoscopic access to the tendons by tendoscopy. These included tendoscopy of the posterior tibial tendon, of the peroneal tendons (4,5), and of the Achilles tendon (6), which was followed by endoscopic treatment for retrocalcaneal bursitis, called endoscopic calcaneoplasty (7,8). In 2000, he introduced a two-portal endoscopic hindfoot approach (9). Recently, the results of 55 consecutive patients with posterior ankle impingement were reported on with a good to excellent outcome in 74% of patients (10). This minimal invasive technique provides excellent access to the posterior aspect of the ankle and subtalar joint. Furthermore, extra-articular structures of the hindfoot such as the os trigonum, flexor hallucis longus (FHL), and the deep portion of the deltoid ligament can be assessed (9).
INDICATIONS AND CONTRAINDICATIONS OF THE PROCEDURES
Contraindications for endoscopic/arthroscopic procedures are few but important. Relative contraindications include severe edema and a tenuous vascular status. More absolute contraindications include localized soft tissue infection and severe degenerative joint disease in arthroscopic procedures. Obesity, although not a contraindication, significantly contributes to a prolonged intraoperative surgical time and postoperative morbidity (11).
The different indications can be categorized according to the location of the pathology.
ARTICULAR PATHOLOGY
Posterior Compartment Ankle Joint
The main indications include both soft tissue and/or bony pathology. Soft tissue pathology mainly includes chronic synovitis, chondromatosis, and excessive scar tissue. Bony pathology includes loose bodies, ossicles, posttraumatic calcifications, avulsion fragments, and osteophytes of the posterior tibial rim. An osteochondral defect (OD) in the ankle joint that cannot be approached by means of anterior ankle arthroscopy with the ankle in maximum plantar flexion can be assessed through posterior ankle arthroscopy.
Osteochondral Defects
A traumatic insult is widely accepted as the most important etiologic factor of an OD of the talus. In 93% to 98% of the lateral talar lesions, trauma has been described and for medial lesions in 61% to 70% (12,13). ODs can either heal and remain asymptomatic or progress to deep ankle pain on weight bearing, prolonged joint swelling, recurrent synovitis, diminished range of motion, and formation of subchondral bone cysts. However, absence of swelling and diminished range of motion does not rule out an OD.
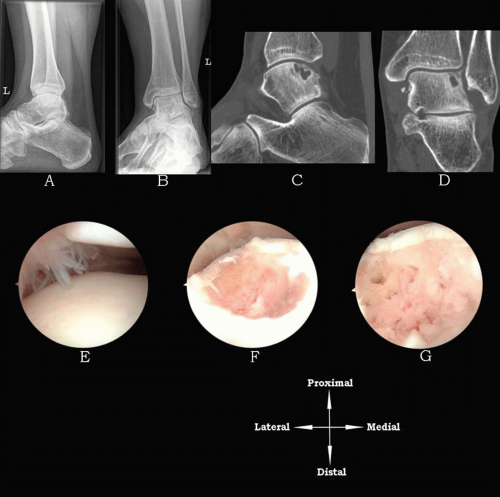
Routine radiographs of the ankle should be obtained after careful history taking and physical examination of the ankle. These consist of weight-bearing anteroposterior (AP) (mortise) and lateral views of both ankles (Fig. 49.1A and B). Initially, the damage may be too small to be visualized on a routine radiograph. The OD sometimes becomes apparent on radiographs at a later stage. A posteromedial or posterolateral defect may be revealed by a heelrise mortise view with the ankle in plantar flexion (14) (Fig. 49.2). Additionally, computer tomography can be performed to confirm diagnosis and to plan arthroscopic treatment (15) (Fig. 49.1C and D).
In case of a symptomatic OD, arthroscopic débridement and bone marrow stimulation remain the best treatment that is currently available for defects up to 15 mm in diameter (13,16). With this technique, all unstable
cartilage including the underlying necrotic bone is removed. Any cysts underlying the defect are opened and curetted. After débridement, multiple connections with the subchondral bone are created by drilling or microfracturing. The objective is to partially destroy the calcified zone that is most often present and to create multiple openings into the subchondral bone (Fig. 49.1). Intraosseous blood vessels are disrupted and the release of growth factors leads to the formation of a fibrin clot. The growth of local new blood vessels is stimulated, marrow cells are introduced in the OD, and fibrocartilaginous tissue is formed (17).
cartilage including the underlying necrotic bone is removed. Any cysts underlying the defect are opened and curetted. After débridement, multiple connections with the subchondral bone are created by drilling or microfracturing. The objective is to partially destroy the calcified zone that is most often present and to create multiple openings into the subchondral bone (Fig. 49.1). Intraosseous blood vessels are disrupted and the release of growth factors leads to the formation of a fibrin clot. The growth of local new blood vessels is stimulated, marrow cells are introduced in the OD, and fibrocartilaginous tissue is formed (17).
Posterior Compartment Subtalar Joint
The main indications are removal of osteophytes; treatment of degenerative changes in the subtalar joint, including talar cystic lesions; loose body removal; and a subtalar arthrodesis in case of osteoarthritis (18, 19, 20, 21). Intraosseous talar ganglions can also be treated arthroscopically (22).
PERIARTICULAR PATHOLOGY
Posterior Ankle Impingement
Posterior ankle impingement syndrome encompasses a group of pathologies that are characterized by posterior ankle pain in plantar flexion. The mechanism can be caused by overuse or trauma. It is important to differentiate between these two groups, because posterior impingement from overuse has a better prognosis (23) and patients are more satisfied after arthroscopic treatment (10).
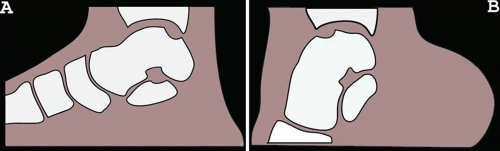
The overuse group mainly exists from ballet dancers, downhill runners, and soccer players (23, 24, 25). In professional ballet, the specific dancing maneuvers force the ankle in hyper plantar flexion. The anatomical structures in between the calcaneus and the posterior part of the distal tibia thereby become compressed. Through exercise, the dancer will attempt to increase the range of motion and joint mobility, ultimately decreasing the distance between the calcaneus and the talus. The anatomical structures at the back of the ankle joint hereby become compressed. Running with more pronounced plantar flexion, such as downhill running, imposes repetitive stresses on the anatomical structures of the posterior ankle area (26). Kicking with the foot in plantar flexion results in high forces on the anatomical structures in the hindfoot. These repetitive high forces can eventually cause posterior ankle impingement.
An isolated or combined hyper plantar flexion—and supination—trauma can damage these structures and may finally lead to a chronic posterior ankle impingement syndrome. Congenital anatomic anomalies such as a prominent posterior talar process, os trigonum, or talus bipartitus (27) could facilitate the occurrence of the syndrome, especially in combination with overuse injury (28, 29, 30). An os trigonum is estimated to be present in 1.7% to 7% and occurs bilateral in 1.4% of the people (28,31,32). During plantar flexion, the soft tissue structures such as synovium, posterior ankle capsule, or one of the posterior ligamentous structures can get pinched and compressed, eventually resulting in swelling, partial rupture, or fibrosis.
The diagnosis is made by means of physical examination. The forced passive hyper plantar flexion test is positive when the patient complains of recognizable pain during the test (Fig. 49.3). A negative test rules out the posterior ankle impingement syndrome. A positive test is followed by a diagnostic infiltration with Xylocaine. Disappearance of pain following infiltration confirms the diagnosis. For radiographic detection of posterior impingement, the AP ankle view typically does not show abnormalities. On a lateral view, the posterolateral part of the talus is often superimposed on the medial talar process. Therefore, detection of a posterolateral talar process or os trigonum is often not possible. We recommend
lateral radiographs with the foot in 25 degrees of external rotation in relation to the standard lateral radiographs (29).
lateral radiographs with the foot in 25 degrees of external rotation in relation to the standard lateral radiographs (29).
Deep Portion of the Deltoid Ligament/Cedell Fracture
Hyper dorsiflexion or eversion trauma can result in avulsion of the posterior talotibial ligament at its insertion into the medial tubercle of the talus. This may result in posttraumatic calcifications or ossicles in the deep portion of the deltoid ligament. These patients typically present with posteromedial ankle pain that is aggravated by running and walking on uneven grounds. Cedell was the first to report four cases of young athletes with ligament avulsion of the deep portion from the posteromedial talar process of the deltoid ligament (34).
Flexor Hallucis Longus Tendon pathology
Posterior ankle impingement syndrome is often accompanied by tenosynovitis or degeneration of the FHL, especially in ballet dancers (30,35,36). The patient experiences pain in the posteromedial part of the ankle (30). On physical examination, the tendon can be palpated behind the medial malleolus. By asking the patient to repetitively flex the big toe, while the ankle is in 10 to 20 degree plantar flexion, the FHL tendon can be identified in its gliding channel, in between the medial and the lateral talar process. In case of tendinitis or chronic inflammation, crepitus and recognizable pain can be provoked by the examiner putting the palpating/compressing finger just behind the medial malleolus. In some cases, a painful nodule in the tendon exists. Arthroscopic treatment can be considered when nonoperative treatment fails to improve symptoms. Débridement of the FHL and release of the flexor retinaculum and tendon sheath up to the level of the sustentaculum tali can be performed in order to achieve unrestricted movement of the tendon.
Peroneal Tendon Pathology
Peroneal tendon pathology frequently coexists with or is secondary to chronic lateral ankle instability. These disorders often cause chronic ankle pain in runners and ballet dancers (37). Posttraumatic lateral ankle pain is seen frequently, but peroneal tendon pathology is not always recognized as a cause of these symptoms. In a study by Dombek et al. (38), only 60% of peroneal tendon disorders were accurately diagnosed at first clinical evaluation. Because the peroneal tendons act as lateral ankle stabilizers, in chronic instability of the ankle more strain is put on these tendons, resulting in hypertrophic tendinopathy, tenosynovitis, and ultimately in tendon tears (4).
Pathology consists of tenosynovitis, tendon dislocation or subluxation, and (subtotal) rupture or snapping of one or both of the peroneal tendons. It accounts for the majority of symptoms at the posterolateral aspect of the ankle (39). Other causes of posterolateral ankle pain are rheumatoid synovitis, bony spurs, calcifications or ossicles, pathology to the posterior talofibular ligament, or disorders of the posterior compartment of the subtalar joint. Posterior ankle impingement can present as posterolateral ankle pain. On clinical examination, there is recognizable tenderness over the tendons on palpation. Swelling, tendon dislocation, and signs of tenosynovitis can be found in peroneal tendon pathology.
The diagnosis of peroneal tendon pathology can be difficult in a patient with lateral ankle pain. A detailed history should include the presence of associated conditions such as rheumatoid arthritis, psoriasis, hyperparathyroidism, diabetic neuropathy, calcaneal fracture, fluoroquinolone use, and local steroid injections. These can all increase the prevalence of peroneal tendon dysfunction (40). A diagnostic differentiation must be made with fatigue fractures or fractures of the fibula, posterior impingement of the ankle, and lesions of the lateral ligament complex.
Additional investigation such as magnetic resonance imaging (MRI) and ultrasonography may be helpful in confirming the diagnosis in (partial) tears of the tendon of peroneus brevis or longus (41,42). Posttraumatic or postsurgical adhesions and irregularities of the posterior aspect of the fibula (peroneal groove) can also be responsible for symptoms in this region.
In case of recurrent peroneal tendon dislocation, the primary indication for treatment is pain. After several months of conservative treatment without improvement, open or nowadays endoscopic/tendoscopic treatment options are available (4,43). An endoscopic fibular groove deepening technique, based on the posterior ankle arthroscopic portals (9), with one additional portal 4 cm proximal to the posterolateral portal (44) was recently introduced. Other peroneal tendon pathologies as for instance synovitis, adhesion, and exostosis can safely be assessed through tendoscopy, resulting in good to excellent clinical outcome (4).
Posterior Tibial Tendon Pathology
In the absence of intra-articular ankle pathology, posteromedial ankle pain is most often caused by disorders of the posterior tibial tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree