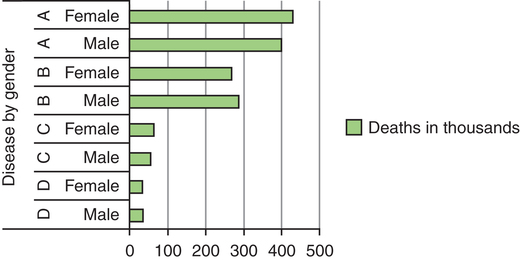
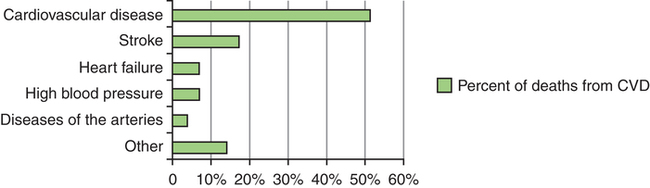
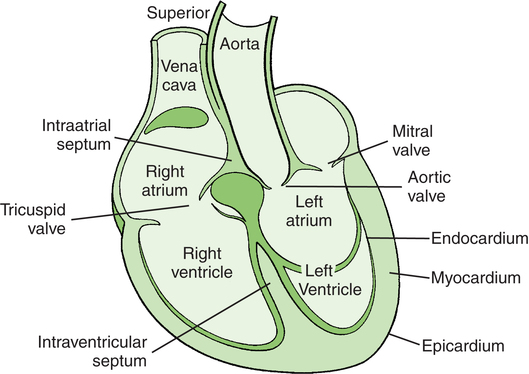
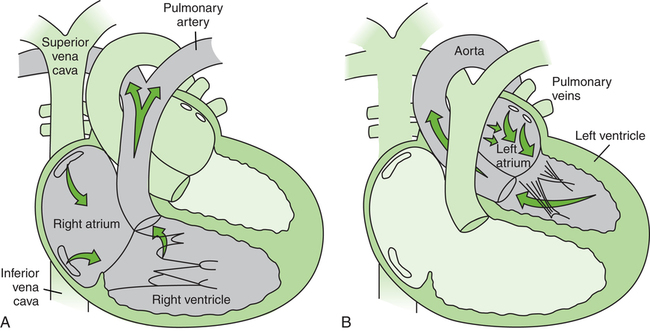
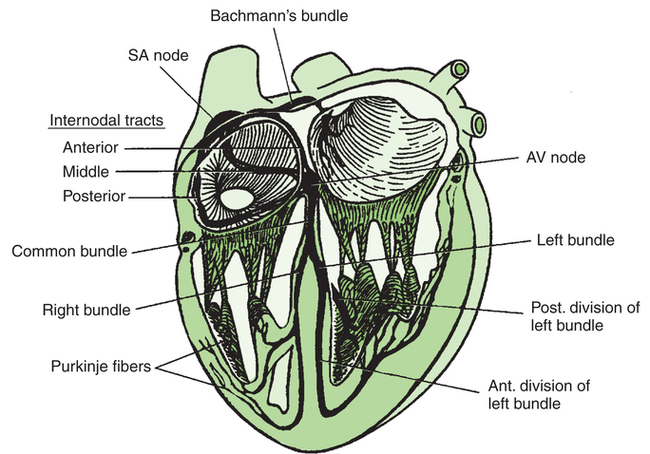
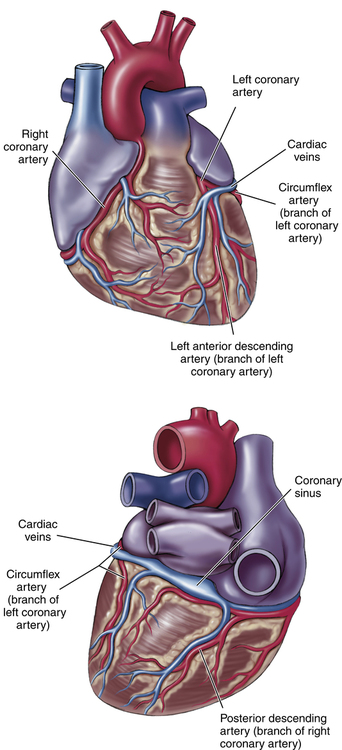
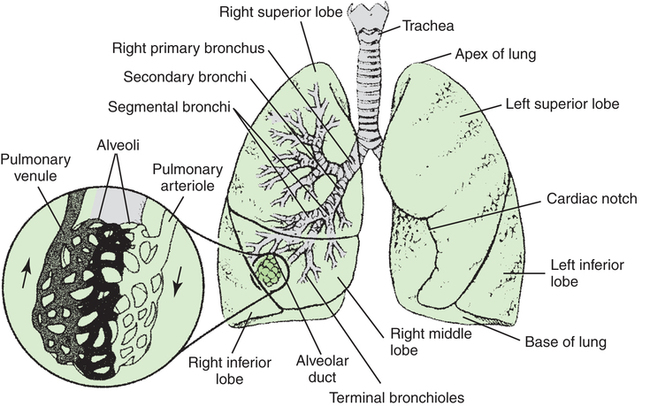
After reading this chapter, the reader will be able to: Cardiovascular disease (CVD) remains the number one cause of death in the United States, claiming over 830,000 lives in 2006 (last full data set available).1 This represents 26% of the more than 2.4 million people who died that year (Figure 10-1). The economic impact and prevalence of this disease are extensive. Estimated direct and indirect costs for 2010 were $485.6 billion for the 81.1 million American adults that had CVD. The prevalence of two or more risk factors for adults 18 years of age or older varies with ethnicity, education, income, and employment status. Data from the 2003 Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System indicate that these factors were highest among blacks (48.7%) and American Indians/Alaska Natives (46.7%) and lowest among Asians (25.9%). Multiple risk factors ranged from 25.9% for college graduates to 52.5% for those with less than a high school diploma (or equivalent). Individuals with household income of $10,000 or less had the highest prevalence (52.5%), whereas those with $50,000 or more had the lowest prevalence (28.8%). Adults who were unable to work had the highest prevalence (69.3%), followed by retired persons (45.1%), unemployed adults (43.4%), homemakers (34.3%), and employed persons (34.0%). Coronary heart disease (CHD), disease specifically of the heart and its vascular supply, is responsible for 51% of all deaths caused by CVD (Figure 10-2).1 This represents 1 of every 6 deaths in the United States in 2006. Approximately every 25 seconds an American undergoes a coronary event, and about every minute someone dies of a cardiac event. For 2010, an estimated 785,000 Americans had a new heart attack (myocardial infarction [MI]) and 470,000 had recurrent attacks. Besides attempts to alter the lifestyle of a person who is at risk for heart disease to decrease the risk factors, direct intervention is commonly used to manage heart disease. In 2006, an estimated 1,313,000 percutaneous coronary interventions (PCIs, previously referred to as angioplasties) were performed. The most common PCI procedure requires inserting a tube into a coronary vessel and inflating a balloon on the end of the tube to open up a blockage in the vessel to restore normal blood flow. Nearly half a million coronary artery bypass procedures were performed, 418,000 pacemaker procedures were completed, and 2163 heart transplantations were performed in 2006.1 In 2008 (last full data set available), 12.1 million people in the United States aged 18 or over had a diagnosis of COPD.2 COPD is the fourth leading cause of death in the United States, and for the last 7 years more women than men died of COPD. As in CVD, gender, race, and age affect the population in which COPD develops. In 2008 the highest percentage of individuals with chronic bronchitis consisted of non-Hispanic white females from the South, ranging from 45 to 64 years of age. The greatest percentage of individuals with emphysema also consisted of non-Hispanic white females from the South, but over the age of 65. In 2010, the projected annual cost of COPD to the nation was $49.9 billion. This included $29.5 billion in direct health care costs, $8 billion in indirect morbidity costs, and $12.4 billion in indirect mortality costs. The heart is positioned left of center in the chest cavity (mediastinum), with the base located superiorly and the apex inferiorly and left of center. A fibrous tissue known as the pericardial sac surrounds the heart. The major portion of the heart is made up of muscle tissue referred to as the myocardium. This tissue is cross-striated with layers of muscle fibers arranged in multiple directions.3 The heart has two pairs of matched chambers. The two atria are thin-walled chambers, whereas the two ventricles have much thicker muscular walls (Figure 10-3).4 These chambers are separated by valves that direct the blood through the chambers in a specific pattern. The right atrium receives venous blood from the body through the superior and inferior venae cavae. With atrial contraction (atrial systole) the blood then passes through the tricuspid valve into the right ventricle (Figure 10-4, A).4 The left atrium receives oxygenated blood through the pulmonary veins coming from the lungs. During atrial systole, this oxygenated blood passes through the bicuspid (mitral) valve into the left ventricle (Figure 10-4, B).4 It is significant that the ventricles have thicker muscular walls than the atria. This greater muscle mass, especially in the left ventricle, must provide enough force to overcome the resistance to flow that blood encounters as it moves through the peripheral arteries.5 The specialized tissues are called nodal and Purkinje fibers (Figure 10-5).6 The sinoatrial (SA) node initiates the impulse (sinus rhythm) and is referred to as the pacemaker of the heart. Once a signal is initiated by the SA node, it travels quickly through the walls of the atria on special tracts to the atrioventricular (AV) node. The impulse also travels to the muscle fibers of the atria and causes them to contract. The AV node transports the signal to the bundle of His, which is where the Purkinje fibers start to spread out into the muscle fibers of the ventricles. For every heartbeat or contraction, the depolarization signal that causes the myocardium to contract must travel through this conduction system of the heart. Both the SA and AV nodes receive autonomic nerve fibers via the sympathetic and parasympathetic systems. These nerve fibers release special neurotransmitters that influence the rate of contraction and myocardial contractility. The ability to influence the heart’s rate and contractility is extremely important because this mechanism allows the central nervous system to tell the heart how to respond to increases in demand, such as those made during exercise.5 The myocardium receives its blood supply from two major vessels: the right and left coronary arteries (Figure 10-6).7 These arteries arise from the ascending aorta, which is the major artery leaving the left ventricle and carrying blood to the body (see Figure 10-3). In general, the right and left coronary vessels supply the right and left sides of the heart, respectively; however, this arrangement can vary a great deal among individuals. If something occurs that causes blockage of a coronary vessel, it is important to determine exactly how that blockage alters blood flow to the individual’s myocardium. A blockage that prevents oxygen supply to the heart, causing permanent damage to the heart cells, is known as a heart attack (myocardial infarction or MI). Respiration is the process of exchanging oxygen and carbon dioxide between the air we breathe and blood cells that pass through the lungs. Ventilation is the process of exchanging air between the atmosphere and the lungs through inspiration and expiration.8 The mechanics of inspiration and expiration depend on many factors, including the structure of the lungs, chest, and muscles. Inspiration occurs when the muscles of ventilation, the most important being the diaphragm, contract to cause an increase in the space within the thoracic cavity. This expansion causes air pressure to drop inside the lungs, which causes air to move into the lungs. Expiration is the reverse of this process. If the body needs increased amounts of oxygen, such as during exercise, the amount of air that must flow into and out of the lungs must markedly increase. When this situation occurs, the muscles of ventilation must work extensively. When disease affects the lungs, the results can be the same. In this case, however, the body is not requiring more oxygen. The ability of air to move normally into and out of the lungs is compromised because of blockage of the tubes that conduct the air. This obstruction results in high resistance to airflow and increased work for the muscles of ventilation.9 Conducting airways are the passageways and tubes that transport air into and out of the lungs. The upper conducting airway includes the nose, pharynx, and larynx. This component of the air transport system cleans and humidifies the air and terminates at the beginning of the trachea. The lower conducting airway is made up of the trachea and bronchiole system (Figure 10-7).9 The bronchiole system consists of tubes branching from the main bronchus out to the terminal bronchioles. It is here that the conduction system ends and air enters into the alveolus, where gas exchange takes place. The alveoli are surrounded by capillaries that contain deoxygenated blood coming from the right ventricle of the heart. It is at this junction that oxygen and carbon dioxide are exchanged, with the reoxygenated blood returning to the left atrium. The lungs are compartmentalized into a system of lobes, which are present because of the structure of the bronchial airway system (Figure 10-7). A special membrane, the pleura, covers the outer surface of the lungs and the inner surface of the chest wall. The pleura is extremely important to the process of ventilation and maintenance of the continuity of the lungs.3 Two major categories of disease processes influence the myocardium: ischemic conditions and cardiac muscle dysfunction.10 The cause of arteriosclerosis, which can affect all vessels of the body, is not completely understood. It is clear, however, that the severity of the arteriosclerotic process can be influenced by many risk factors (Box 10-1).11 Some of these factors cannot be changed, such as having a family history of CHD. However, most of these risk factors can be modified or eliminated completely by changes in behavior. PTs and PTAs promote a healthy lifestyle and help patients with cardiac dysfunction to alter their behavior as they progress through the rehabilitation process. Cardiac muscle dysfunction refers to various pathologic conditions associated with heart failure.10 Heart failure occurs when a disease process or congenital defect either directly or indirectly causes a decrease in the pumping capability of the heart muscle. These disease processes can occur either acutely or gradually. An example of an acute change in the heart’s pumping capability is the occurrence of an MI (heart attack). In this case one of the coronary arteries suddenly becomes blocked by an embolus (clot). When embolism occurs, blood flow to heart muscle beyond the embolus stops, and the part of the heart muscle no longer receiving blood dies. If this embolus causes an interruption in blood flow to a large amount of heart muscle, death can result. When the heart muscle is compromised to the point that it cannot move blood volume effectively, congestive heart failure (CHF) will develop. This disorder can occur acutely or chronically. When CHF is present, the ventricles are not adequately pumping the appropriate volume from their chambers. When the right ventricle is not contracting efficiently, blood volume backs into the venous system and fluid collects in the liver, abdominal cavity, and legs. If the left ventricle does not contract appropriately, an abnormal amount of blood volume remains in the lungs, which results in fluid collection. The right ventricle then has to work harder because it must try to push blood into the lungs against increased resistance. This increased workload eventually leads to compromised function of the right ventricle (see Figure 10-4, A). Diseases of the lung are generally classified as being obstructive or restrictive. If pathologic changes in the lung cause an abnormality in airflow through the bronchial tubes, the process is defined as obstructive lung disease, whereas if pathologic changes cause the volume of air in the lungs to be reduced, the process is defined as restrictive lung disease.10 How lung diseases are classified is a controversial subject. What is most important is that the common diseases that change lung function eventually demonstrate both obstructive and restrictive characteristics.12 COPD is a group of disorders that produce certain specific physical symptoms. These symptoms include chronic productive cough, excessive mucus production, changes in the sound produced when air passes through the bronchial tubes, and shortness of breath (dyspnea). The specific disorders that can produce these changes include chronic bronchitis (inflammation of the bronchi), emphysema (trapping of air in the alveoli), and peripheral airway disease (collapse of terminal bronchioles). Other disorders sometimes included in this disease group include bronchial asthma (spasmlike contraction of bronchi, resulting in air trapping) and cystic fibrosis (dysfunction of mucous glands, causing blockage of bronchi).12 Differences between these obstructive diseases include their cause, pathology (what tissues are affected and how they are changed), and management. However, all of them cause similar symptoms in varying degrees. As resistance to airflow increases because of the decreasing lumen size of the bronchioles, the thorax enlarges as a result of air trapping. This enlargement of the thorax causes the respiratory muscles to work harder. With time, the effectiveness of the respiratory muscles decreases. With chronic hypoxemia, changes begin to occur in the function of the heart, in blood pressure, and in the thickness of the blood. All these changes can lead to respiratory failure.10,12 The signs and symptoms that develop as restrictive disease progresses include some of the same changes seen in COPD, such as shortness of breath and chronic cough. In the case of restrictive lung disease, however, the cough is nonproductive (does not bring mucus out of the lungs). Other changes include tachypnea, or an increase in the rate of breathing, which results in a marked increase in the amount of energy expended on breathing. This increased energy cost can be so severe that it results in weight loss and an emaciated appearance. Patients with restrictive lung disease are also subject to the problems associated with hypoxemia.10,12 The examination performed by PTs and PTAs is an inclusive process that involves not only the patient, but also the family and other caregivers who are participating in the overall care of the patient. It includes a review of the patient’s past medical and social history, review of the body systems, and tests and measures to gather data about the patient’s condition. Areas reviewed include not only physical parameters, but also functional, psychological, social, and employment conditions. The tests and measures that are selected to examine a patient/client depend on various parameters, including the age of the patient/client; severity of the problem; stage of recovery (acute, subacute, chronic); phase of rehabilitation (early, intermediate, late, return to activity); and home, community, and work status.13 Table 10-1 describes tests and measures commonly performed in the examination of patients with cardiovascular and pulmonary conditions.13 Table 10-1 Description of Common Tests and Measures for Patients with Cardiovascular and Pulmonary Conditions Data from American Physical Therapy Association (APTA): Guide to physical therapist practice, revised ed 2, Alexandria, Va, 2003, APTA.
Physical Therapy in Cardiovascular and Pulmonary Conditions
 Describe the normal anatomy and physiology of the cardiovascular and pulmonary systems
Describe the normal anatomy and physiology of the cardiovascular and pulmonary systems
 Define and describe the effects of common diseases that alter normal function of the cardiovascular and pulmonary systems
Define and describe the effects of common diseases that alter normal function of the cardiovascular and pulmonary systems
 Outline how the functions of the cardiovascular and pulmonary systems are evaluated both normally and when disease is present
Outline how the functions of the cardiovascular and pulmonary systems are evaluated both normally and when disease is present
 Discuss how physical therapists examine, evaluate, and provide interventions to individuals who have cardiovascular or pulmonary disease
Discuss how physical therapists examine, evaluate, and provide interventions to individuals who have cardiovascular or pulmonary disease
General Description
Prevalence
Cardiovascular System
Heart
Conduction
Coronary Arteries
Pulmonary System
Respiration
Conducting Airways and Lungs
Common Conditions
Cardiovascular Diseases
Ischemic Conditions
Cardiac Muscle Dysfunction
Lung Diseases
Chronic Obstructive Pulmonary Disease
Restrictive Lung Diseases
Principles of Examination
Function or Characteristic
Description
Home, work, and community (job, play, school)
Analysis of the home and work environments to determine the level of functional capacity needed to perform safely within these environments. Examination of the patient’s capacity to function at an appropriate level of social interaction with various populations (e.g., family, peers, strangers).
Ergonomics and body mechanics
Determination of the dynamic capabilities required of the patient to safely perform within various environments (e.g., home, work, school, leisure).
Aerobic capacity and endurance
Assessment of cardiovascular and pulmonary performance during controlled exercise and functional activities. Can include measuring oxygen consumption, heart and respiratory rates, blood pressure, dyspnea, and blood gases; electrocardiogram; and heart and lung auscultation.
Ventilation and respiration
Assessment of pulmonary function, arterial blood gases, airway clearance efficiency, and perceived exertion and dyspnea during and after exercise; measurements of strength and endurance of muscles of ventilation and of chest wall mobility and expansion.
Anthropometric characteristics
Determination of body fat composition.
Muscle strength and endurance
Assessment of functional muscle strength and endurance as they relate to exercise protocols.
Posture
Assessment of posture abnormalities and their effect on energy cost during movement.
Range of motion
Assessment of limitations in joint range of motion and impact on energy cost during movement.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine