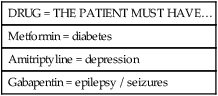
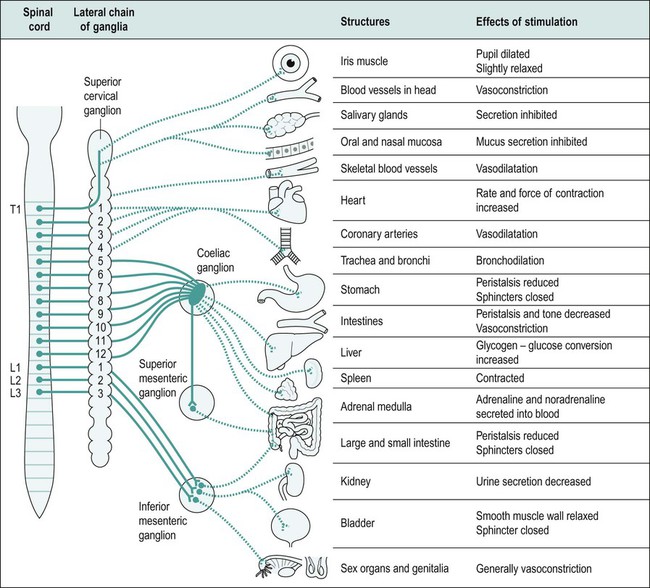
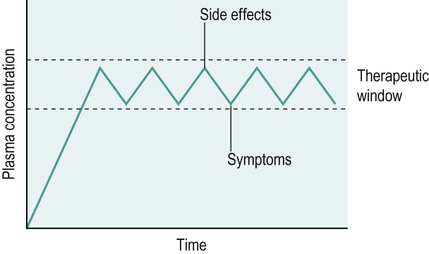
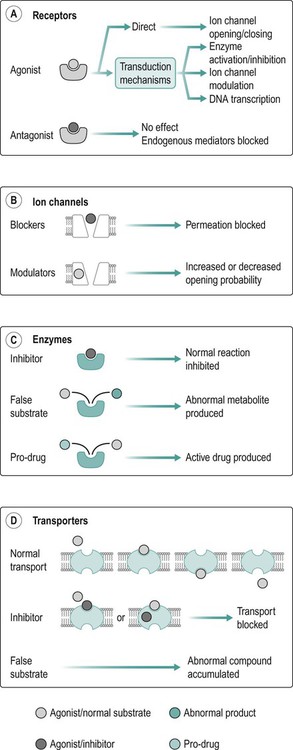
Clinical pharmacology is an entire science; this is a chapter within a book. In no way will it cover the entire breadth and scope of the topic, but rather provide a brief overview of the application of basic scientific knowledge regarding common medicines encountered by the physiotherapist. This information should be adequate for your studies, but I hope to light the touch paper of an explosive interest in pharmacology which you may fuel further by reading the recommended texts at the end of this chapter. A basic physiological knowledge is expected to be enough to understand pharmacology; however, where possible, the relative physiology will be explained. Please note that Chapters 12 and 17 may be a useful starting point. Please see the end of this chapter for a reference glossary of pharmacology terms and some common drugs. When talking about a drug, the typically accepted method is as outlined in Table 4.1. Table 4.1 This is all you need to know about ibuprofen for the adult in one paragraph, simple! However, this chapter herein avoids using this method for two reasons: Their action will ultimately have an impact on the cell to which the surface protein is attached, and therefore the tissue, organ and system in which the cell resides. A cell has three main options during normal function: excitation – such as that of a depolarised neurone – contraction or secretion. The drugs will affect the cells’ ability to express themselves either making them more active, less active or maintaining normal function by blocking other substances from affecting them (Figure 4.1). Table 4.2 • epithelial surface application (skin, nasally, corneal, etc.); • injection (subcutaneous, intramuscular (i.m.), intravenous (i.v.), etc.). These routes each have additional factors which will contribute to how well the drug is absorbed, for example: • dissociation constant (kPa/physiochemical factors of the drug; see the Glossary term ‘pH and ionisation’ for details). Wherever they are heading, they will need to cross a membrane along their way. They will do this in one of the following ways: • diffusion through the lipid bilayer; • transmembrane carrier protein; • pinocytosis (invagination of the cell membrane creating an intracellular vesicle); The sympathetic response is part of the ‘fight or flight’ reaction. Part of the sympathetic effect is to decrease the gastric blood flow in favour of skeletal muscle and reduce peristalsis (this is the fight or flight response which is explained in exquisite clarity in Payne’s Handbook of Relaxation Techniques: A Practical Guide for the Health Care Professional). By encouraging relaxation you will allow the parasympathetic nervous system to resume control and allow normal absorption of drugs and food from the gut (Figure 4.2). Figure 4.3 is a basic representation of delivery of i.v. morphine. An initial bolus dose is given until analgesia is achieved and then a top-up is given, perhaps by a patient-controlled analgesia device. This ensures that the plasma concentration is always in the therapeutic window. All medications taken by the patient should be known to all involved in their care. • direct action on myocardial cells (anti-dysrhythmic drugs, inotropes, etc.); • indirect cardiac function (diuretics, angiotensin converting enzyme (ACE) inhibitors, etc.); Statins help reduce the levels of low-density lipoprotein cholesterol (LDL-C) which adhere to damaged blood vessel walls as part of the athrogenesis chain reaction which ultimately results in significant vessel damage. The action is rather complex and involves an understanding of the mechanism of cholesterol transport and lipoprotein metabolism that exceeds the scope of this chapter. Suffice to say, they reduce circulatory HDL levels (see Chapter 20 of Rang and Dale’s Pharmacology for more detail). Examples of common statins are simvastatin, atorvastatin and pravastatin. As a physiotherapist, it is worth remembering that statins commonly cause muscle pain, so additional medical history may be required relating to how long they have been taking statins: does the pain correspond? Usually, by alerting the prescriber, the problem may be resolved by reducing the dose or changing the drug.
Pharmacology
Introduction
Pharmacology?
What is pharmacology?
Drug
The name of the drug
Route and dosage
Orally, injected, rectally, transdermal, etc.
Pharmacodynamics
What the drug does to the body
Pharmacokinetics
What the body does with the drug
Metabolism/excretion
How is the drug eliminated
Side effects
Including contraindications/precautions, etc.
Basic science
Where do drugs act (Table 4.2)?
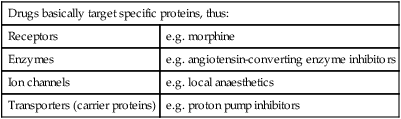
Drugs basically target specific proteins, thus:
Receptors
e.g. morphine
Enzymes
e.g. angiotensin-converting enzyme inhibitors
Ion channels
e.g. local anaesthetics
Transporters (carrier proteins)
e.g. proton pump inhibitors
How may drugs get to their destination?
A note on dosing
Medicines you will (probably) encounter
The heart and vascular systems
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine