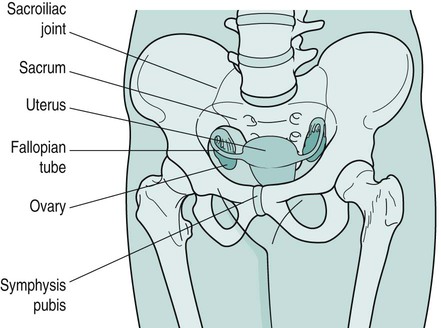
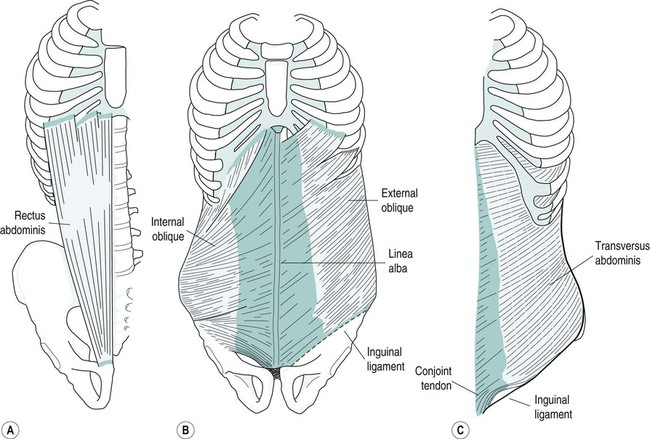
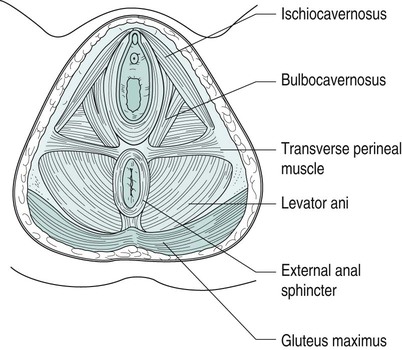
Gill Brook, Tamsin Brooks, Yvonne Coldron, Ruth Hawkes, Judith Lee, Melanie Lewis, Jacquelyne Todd, Kathleen Vits and Liz Whitney The pelvic girdle protects and supports the pelvic contents, provides muscle attachment and facilitates the transfer of weight from trunk to legs in standing, and to the ischial tuberosities in sitting. The joints (Figure 27.1) are supported by some of the strongest ligaments in the body, which may become more lax in pregnancy leading to increased joint mobility and less efficient load transfer through the pelvis. The pelvic outlet at the base of the pelvis is narrower in transverse diameter when compared with the pelvic inlet; it comprises the pubic arch, ischial spines, sacrotuberous ligaments and coccyx (Haslam 2004a). Four pairs of abdominal muscles combine to form the anterior and lateral abdominal wall, and may be termed the abdominal corset. Transversus abdominis (TrA), whose fibres run transversely, lies deep to the internal abdominal oblique (IO) and external abdominal oblique (EO), with the rectus abdominis (RA) central, anterior and superficial (Figure 27.2). IO, EO and TrA insert into an aponeurosis joining in the midline at the linea alba. The deep abdominal muscles, together with the pelvic floor muscles, multifidus and diaphragm, can be considered as a complete unit and may be termed the lumbopelvic cylinder. This provides support for the abdominal contents and maintains intra-abdominal pressure (Cresswell et al. 1992). At low level muscle activity force is exerted on the thoracolumbar fascia and studies suggest that this contributes to lumbopelvic stability, crucial to pain-free resting posture and normal function (Richardson et al. 1999). Motor control of the muscles of the lumbopelvic cylinder is also significant in maintaining continence and controlling respiration. The main function of RA is lumbar spine flexion (Sapsford et al. 2001), while the obliques, interlaced diagonally in midline deep to the recti, produce side-flexion and rotation of the spine. In later pregnancy, the growing uterus stretches the abdominal muscles and may cause RA to be separated in midline by several finger widths (Sapsford et al. 1998). This inter-recti distance – diastasis rectus abdominis muscle (DRAM) – can persist postnatally (Barton 2004; Coldron et al. 2008). The pelvic floor is a fascial and muscular sheet forming the inferior boundary of the abdominopelvic cavity (Figure 27.3). It supports the pelvic and abdominal contents and comprises four layers. The deepest (viscerofascial) is important for both organ support and muscle attachment. The next part of the supportive mechanism and assisting with the sphincteric control of the bladder and bowel is formed by the levator ani muscles – pubococcygeus (pubovisceral muscle), puborectalis, ileococcygeus and ischiococcygeus. The co-coordinated action of levator ani, in the presence of intact fascia, generates a rise in intra-abdominal pressure to maintain organ support, and urinary and faecal continence. Contraction of the pelvic floor muscles (PFM) results in a cranio-ventral movement that has been observed by real-time ultrasound (Lovegrove Jones et al. 2009). The next layer is a dense triangular membrane lying anteriorly – the perineal membrane. It is of importance for connection of the urethra, vagina and perineal body to the ischiopubic rami (De Lancey 2001). The most superficial external genital muscles – ischiocavernosus, bulbocavernosus and the transverse perineal muscles – have a sexual function in assisting a woman to achieve orgasm. It has always been believed that the pudendal nerve, from sacral nerve root S2–4, supplies all of the pelvic floor muscles. However, Barber et al. (2002) suggested that although the pudendal nerve supplies the urethral sphincter and the external genital muscles, levator ani has a distinctive separate nerve supply from S3–5 which has been named the ‘nerve to levator ani’. This theory is under some dispute. Pregnancy and childbirth are major contributory factors to pelvic floor muscle dysfunction (Freeman 2002). Women who suffer urinary incontinence in pregnancy are twice as likely to be symptomatic 15 years after childbirth (Dolan et al. 2003). Vaginal delivery also increases the likelihood of future urinary and faecal disorders, but caesarean section may not be fully protective (MacArthur et al. 2006). It is also thought that there is a possible genetic factor related to collagen (Hannestad et al. 2004). The uterus – a hollow, pear-shaped organ – comprises the fundus, body, isthmus and cervix, and weighs about 50 g in its normal state (Haslam 2004a). Together with the ovaries, it is suspended in connective tissue and peritoneum inside the true pelvis (Figure 27.1). The broad ligament (a double fold of peritoneum) extends from the lateral walls of the uterus to the sidewalls of the pelvis, dividing the pelvic cavity into two compartments – the anterior (containing the bladder) and the posterior (containing the rectum). The ovaries lie in the broad ligament on each side of the uterus. Behind and slightly above are the trumpet-shaped open ends of the contractile fallopian tubes. Their tentacle-like fringes (fimbriae) catch the ovum when it erupts from the ovary at ovulation. The free ovum is propelled along the fallopian tube to the uterus by a peristaltic wave and the cilia lining the tube walls. On fertilisation, the ovum is embedded in the endometrium lining the uterus. If fertilisation has not occurred, the lining is shed (menstruation). Following fertilisation of the ovum, the first sign of pregnancy is amenorrhea (cessation of menstruation). As pregnancy progresses, the uterus grows, its muscle fibres lengthening and thickening, and weight increasing from 50 g to 1000 g at term. By 12 weeks it has enlarged to become an abdominal organ. Gestational dates can be determined by the level of the uterus, which continues to rise until the later weeks of pregnancy. Co-ordinated contractions of the uterus may be felt by women from about 20 weeks (Braxton Hicks contractions). These contractions assist in blood flow through the placental site and in development of the lower uterine segment. The cervix gradually increases in size with an increase in collagen content, hypertrophy of external muscle fibres and increase in vascularity (McNabb 1997) and becomes slightly softer in consistency. A mucous plug acts as a barrier to infection. • progesterone decreases smooth muscle tone, initiates sensitivity to carbon dioxide in the respiratory centre, and causes an increase in maternal temperature, breast development, and storage of fat deposits for milk production; • oestrogen influences uterine and breast growth and development, prepares prime receptor sites (e.g. pelvic joints) for relaxin, and causes increased water retention. Increased vaginal glycogen predisposes pregnant women to thrush; • in target areas relaxin replaces collagen with a modified form of greater pliability and extensibility. It may have a softening effect on connective tissue (pelvic floor and abdominal fascia), increasing extensibility in those structures. It also inhibits myometrial activity up to 28 weeks gestation. Kypho-lordotic, sway back and flat back have been described as ideal postures (Kendall et al. 2005). The overall equilibrium of the spine and pelvis alters as pregnancy progresses but there is still confusion as to the exact nature of any associated postural adaptation. With weight gain, increased blood volume and ventral growth of the fetus, the centre of gravity no longer falls over the feet and women may need to lean backwards to gain equilibrium (Abitol 1997) resulting in disorganisation of spinal curves. Reported postures include a reduction in lumbar lordosis (Moore et al. 1990), an increase in both lumbar lordosis and thoracic kyphosis (Bullock-Saxton 1991) or a flattening of the thoracolumbar spinal curve (Gilleard et al. 2002). These differences imply a large individual variation with no ‘normal’ posture in pregnancy and antenatal lumbopelvic posture may be an accentuation of normal pre-pregnancy posture. There will be compensatory changes to posture in the thoracic and cervical spines, and this combined with the extra weight of the breasts may result in posterior displacement of the shoulders and thoracic spine, and increase of the cervical lordosis. Postural changes may still be present 12 weeks postnatally (Bullock-Saxton 1991). Altered levels of relaxin, oestrogen and progesterone during pregnancy result in an alteration to collagen metabolism and increased connective tissue pliability and extensibility. Therefore, ligamentous tissues are predisposed to laxity with resultant reduced passive joint stability. The symphysis pubis and sacroiliac joints are particularly affected to allow for birth of the baby. Ligamentous laxity may continue for six months postpartum (Foti et al. 2000). Biomechanical changes of the spinal and pelvic joints may involve an increase in sacral promontory, an increase in lumbosacral angle, a forward rotatory movement of the innominate bones, and downward and forward rotation of the symphysis pubis (Golightly 1982). The normal pubic symphyseal gap of 4–5 mm shows an average increase of 3 mm during pregnancy (Abramson et al. 1934). Pelvic joint loosening begins around 10 weeks, with maximum loosening near term. Joints should return to normal at 4–12 weeks postpartum (Snow and Neubert 1997). The sacrococcygeal joints also loosen. By the last trimester, the hip abductors and extensors, and the ankle plantarflexors increase their net power during gait (Foti et al. 2000) and there is an increase in load on the hip joints of 2.8 times the normal value when standing and working in front of a worktop (Paul et al. 1996). As the uterus rises in the abdomen the rib cage is forced laterally and the diameter of the chest may increase by 10–15 cm (Polden and Mantle 1990). Abdominal and pelvic muscles contribute to spinal and pelvic stability via active tension exerted on the passive ligamentous and fascial stability structures. During pregnancy the enlarged uterus results in elongation of the abdominal muscles and separation of the linea alba (Boissonnault and Blaschak 1988). Passive joint instability (as seen in pregnancy) alters afferent input from joint mechanoreceptors and probably affects motor neurone recruitment. A decrease in muscle stiffness and thus active stability of joints may result from alteration of muscle spindle regulation (Bullock-Saxton 1999) and this is applicable particularly to muscles around the pelvic girdle. These changes may lead to poor recruitment of the muscles responsible for pelvic girdle stability (particularly gluteus medius and maximus) and result in decreased tension of these muscles during walking, perhaps resulting in pelvic girdle pain (PGP). As pregnancy progresses, rectus abdominis (RA) elongates (Gilleard and Brown 1996) and becomes wider and thinner (Coldron et al. 2008). In many women the disproportion between width and thickness remains at 12 months postpartum (Coldron et al. 2008). Although the consequences of this are unknown, the strength of gross muscle flexion can be impaired at 24 weeks postpartum (Potter et al. 1997b). The linea alba becomes wider and thinner via hormonally-mediated change as the fetus grows anteriorly, with the two bellies of RA curving round the abdominal wall (Haslam 2004b). In nulliparous women the inter-recti distance (IRD) at the umbilicus is approximately 11 mm (± 3.62) whereas the divarication of the linea alba during the third trimester and immediately postpartum may vary widely between women, with an average gap of 42 mm (± 20.28) at the umbilicus (Coldron et al. 2008). The linea alba can split and become a diastasis with herniation of the abdominal contents. Diagnostic criteria of a pathological diastasis at the umbilical level in people under 45 years has been defined by Rath et al. (1996) as an IRD of >27 mm. The IRD at the umbilical level has been shown to resolve to about 22 mm (± 9.44) by 8 weeks postpartum, when it reaches a plateau, though in a minority of women a diastasis may persist (Coldron et al. 2008). There is very little information on the effect of pregnancy on the three lateral abdominal muscles (transversus abdominis (TrA), internal (IO) and external (EO) obliques). However, research on normal subjects has identified the importance of TrA as the prime stabiliser of the trunk (Hodges 1999). Decreased stabilisation of the pelvis happens in late pregnancy and poor stability persists at eight weeks postpartum (Gilleard and Brown 1996). In one study, EO appeared to atrophy during pregnancy but hypertrophy in the postnatal period to become thicker than that of nulliparous controls (Coldron 2006). Furthermore, the thickness of the middle fibres of IO and TrA was significantly greater in day 1 postpartum women than that of controls, but by eight weeks postpartum there was no difference between the two groups. Parity, exercise and a history of lumbopelvic pain had no bearing on the results. The relevance of these findings is unknown but it may be that IO and TrA had an increase in stability function during pregnancy from load-bearing with the weight of the fetus. During pregnancy there is stretching to the pelvic floor and trauma/tearing during labour and vaginal delivery. It is now thought that the function and recruitment of TrA and the pelvic floor musculature are closely associated, with voluntary activity in the deep abdominal muscles resulting in increased pelvic floor muscle activity (Sapsford and Hodges 2001). There is an association between PFM dysfunction and pregnancy-related lumbopelvic pain (Pool-Goudzwaard et al. 2005). Labour continues to be described in three stages, though this theory has been challenged in recent years (Winter and Cameron 2006). The first stage of labour is from the commencement of regular uterine contractions effecting dilatation (opening) of the cervix, culminating when the cervix is fully dilated, allowing the passage of the fetus into the birth canal. It can be further subdivided into the latent phase (early labour), where contractions are short and irregular, and the active phase (established labour), where contractions become intense and regular (Chapman and Charles 2009). Contractions (tightening) and retraction (shortening) of myometrial muscle fibres increase in length, strength and frequency as labour progresses. The mucous plug (show) is expelled as the cervix opens and the membrane sac (amnion and chorion) often spontaneously ruptures, allowing amniotic fluid to drain. Various changes can be observed in women adapting to the intensity of contractions. Expenditure of energy increases the need for hydration and food, although as labour progresses appetite is often suppressed. Women may appear hot, flushed and agitated as intense contractions may cause pain, fear and distress. Endorphin release in response to pain provides an analgesic and euphoric bolster, which may cause some women to appear calm, quiet and withdrawn. Many women find relief through their own instinctive behaviour, such as mobility, change of position and posture (De Jonge and Lagro-Jansen 2004), warm baths or compresses, massage, relaxation and distraction techniques. The second stage of labour is the expulsive stage culminating in the birth. Commonly defined as commencing from full dilatation of the cervix which was thought to herald the urge to push, it has been suggested (Long 2006) that second stage labour commences ‘when the presenting part has passed through the cervix and is below the ischial spines’. When the presenting part distends the genital tract and pelvic floor a surge of oxytocin is released, known as the fetal ejection or Ferguson reflex, whereby strong expulsive contractions facilitate the birth. Throughout the second stage women should be encouraged to instinctively bear down as the urge occurs with a contraction, adopting positions which increase the pelvic outlet (Gupta et al. 2004). Prolonged breath-holding and overzealous pushing should be avoided, as this interferes with placental perfusion and may compromise the fetus. The environment should feel safe and non-threatening, with minimal intrusion from staff, and the midwife should be confident in her skill to support normal labour (Downe 2010). Kabeyama and Miyoshi (2001) demonstrated that self-control was the most important factor in a satisfactory childbirth experience, and women who experienced labour as a challenge, utilising their own resources through breathing and relaxation, had better outcomes. Management of pain relief should therefore take a woman-centred approach utilising the whole spectrum of pain management options. Non-pharmacological approaches to pain management, such as position and posture, play an important part in labour and most women will naturally adopt positions which enhance labour, if they are provided the space and freedom to do so. Warm baths, compresses, massage, breathing, relaxation, music, dance and distraction techniques can also be used to great advantage in labour (Hamilton 2010). Complementary therapies, such as hypnotherapy, aromatherapy, acupuncture and reflexology, should also be considered utilising suitably qualified practitioners. Transcutaneous electrical nerve stimulation (TENS) can be used in labour. A low-frequency high-intensity current of 2–10 Hz is thought to increase the production of endorphins and encephalins. This is applied throughout labour and a high-frequency low-intensity current at 100–200 Hz which activates the pain-gate mechanism (Melzack and Wall 1982) is used during the more intense contractions. The current is introduced via four electrodes placed over the nerve roots to the uterus (T10–L2) and the pelvic floor and perineum (S2–S4). The two channels enable individual control of each pair of electrodes. TENS is easy to apply, is non-invasive and has no known side effects for mother or baby. It allows mobility and affords the woman some control of her analgesia. It cannot be used in water and may, on occasion, interfere with the cardiograph tracings. Recent evidence demonstrates that a reduction in the demand for pethidine and other pain relief was found when TENS was employed (Poole 2007). Opiates, such as pethidine, diamorphine and meptazinol, may be used to relieve pain in labour. Pethidine is historically the most common drug of choice in the UK. Easily administered by intramuscular injection these drugs have similar pain-relieving properties, although their benefits in labour have been challenged (Collis 2000) owing to the episodic nature of contractions and the unpleasant side effects of nausea, vomiting, drowsiness, amnesia, feeling of loss of control and depression of the respiratory centre, especially in the neonate. Neonatal drowsiness also interferes with the establishment of breastfeeding. Epidural will provide a pain-free labour provided it is sited and working correctly. A regional anaesthetic is introduced into the lumbar epidural space by an experienced obstetric anaesthetist. A combination of local anaesthetic (bupivicaine) and opioid (fentanyl) is used to provide adequate analgesic effect with minimal impact on mobility and blood pressure. Continual infusion of drugs as opposed to a bolus dose has been found to reduce the risk of instrumental delivery (COMET 2001). Possible side effects include dural puncture and possible headache, loss of bladder sensation requiring catheterisation, risk of instrumental delivery, infection, backache (possibly as a result of poor posture or localised bruising), total spinal block and respiratory arrest, neurological sequelae (rare). Occasionally, an incision through the perineal tissues may be required but should not be undertaken lightly and always with consent. Two main indications for episiotomy have been identified (Carroli and Belizan 2009): to enlarge the vulval outlet in order to minimise severe trauma to the vagina and perineum, in particular where instrumental delivery is required; and in cases of fetal distress to expedite delivery. Local anaesthetic is infiltrated and a mediolateral incision is made to prevent damage to the Bartholins gland and reduce the risk of extension of the incision into the anal margin (Downe 2010). Assisted vaginal birth by vacuum extraction or forceps is a widely practised intervention used to expedite delivery where there is delay in the second stage, maternal exhaustion or fetal distress. It is more commonly used among women who choose epidural as a form of pain relief (Anim-Somuah et al. 2005). Forceps delivery involves separately placing two spoon-shaped metal blades (which lock into place) on either side of the fetal head. Slow, steady traction and maternal effort is applied to deliver the fetus. Forceps may also be used to protect the head of the preterm fetus or the after coming head in the breech (Hamilton 2010). Adequate analgesia must be provided prior to assisted birth. Induction of labour is an intervention to initiate labour where there is disadvantage to the continuation of pregnancy. The mother may also request induction for social reasons (NICE 2008a). Indications for induction of labour include prolonged pregnancy (exceeding 42 completed weeks), maternal factors (hypertension, diabetes), or pre-labour rupture of membranes, which may lead to infection risk. Fetal factors include growth restriction, macrosomia (large baby), fetal anomaly or fetal death. Different approaches to induction can be used individually or collectively: • stretch and sweep – a digital vaginal examination to stretch the cervix, sweeping the membranes and separating them from the uterine wall; • prostaglandin – administered vaginally to ripen the cervix, which may initiate labour; • artificial rupture of the membranes once the cervix has started to dilate; • lactation is initiated and established or suppressed; • the uterus involutes, returning almost to the pre-pregnant size and position; • the placental site begins to heal and the lochia (blood loss) diminishes to a creamy white discharge; Many women require a considerably longer time to adjust both physiologically and psychologically to the complex life-changing event of childbirth. High expectations with regard to regaining pre-pregnancy shape and lifestyle are not always reflected in reality and can lead to low self-esteem and feelings of inadequacy. Talking and sharing worries both with the health professional and other mothers can be beneficial, and women should be made aware of local groups (Byrom et al. 2010). • education of pregnant women for pregnancy, labour and beyond (see section on antenatal classes); • advice on exercise (see the section on exercise and pregnancy); • identification, assessment and treatment of musculoskeletal problems (dealt with in this section). During pregnancy approximately one in three women experiences stress urinary incontinence (Francis 1960; Stanton et al. 1980; Viktrup and Lose 2001) and pregnancy and birth can have an adverse effect on the area through perineal trauma, muscle, connective tissue and pudendal nerve damage (Snooks et al. 1984; Allen et al. 1990). Pelvic floor muscle exercises (PFME) during pregnancy are effective in reducing urinary incontinence in pregnancy and the immediate postnatal period (Mørkved 2007) and the National Institute for Health and Clinical Excellence (NICE 2006) recommends PFME for every woman during her first pregnancy (see the section on urogenital dysfunction). During pregnancy, physiotherapists may consider it prudent to limit their intervention to advice. Lumbopelvic pain is common during pregnancy with a prevalence described variously as ranging from 50% to 70% (Mantle et al. 1977; Fast et al. 1987; Berg et al. 1988; Ostgaard and Andersson 1991; Wu et al. 2004; Mogren and Pohjanen 2005; Gutke et al. 2006). It may be of spinal and/or pelvic girdle origin (Ostgaard et al. 1996; Stuge et al. 2003; Wu et al. 2004; Vleeming et al. 2004; Mogren and Pohjanen 2005; Gutke et al. 2006). Pain of spinal origin is normally referred to as low back pain (LBP). Pregnancy-related PGP is a global term that encompasses symphysis pubis dysfunction, diastasis symphysis pubis and sacroiliac joint pain. Lumbopelvic pain is often regarded as ‘a normal part of pregnancy’ but, without appropriate treatment, a minor episode may develop into a chronic problem. A third of women report severe back pain that interferes with daily life and compromises their ability to work (Ostgaard and Andersson 1991; Mens et al. 1996). Most backache resolves quickly postpartum, but may continue for 18 months (Ostgaard and Andersson 1992) or present postpartum for the first time (Russell and Reynolds 1997). Some patients experience a relapse around menstruation and in a subsequent pregnancy (Mens et al. 1996). The anatomical origins of pregnancy-related lumbopelvic pain vary and are difficult to determine and diagnose (Nilsson-Wikmar et al. 1999). Common conditions include unilateral sacroiliac dysfunction, symphysis pubis dysfunction, minor lumbar disc herniation, lumbar zygapophyseal joint problems, thoracic spine pain and coccydinia. Women describe pain variously as occurring in the low back, sacral, posterior thigh and leg, anterior thigh, pubic, groin and hip areas. These may occur simultaneously or separately, antenatally, during delivery or postnatally (Heiberg and Aarseth 1997). There is often associated cervical, thoracic or coccygeal pain. Sciatic pain is common and may be of lumbar origin or from sacroiliac joint involvement because the L5 and S1 components of the lumbosacral plexus run immediately anterior to the sacroiliac joints. Several studies have differentiated between pregnancy-related LBP and PGP (Ostgaard et al. 1994, 1996; Ostgaard 1997; Noren et al. 2002; Vleeming et al. 2004; Bastiaanssen et al. 2005; Gutke et al. 2006). It is important that both the lumbar spine and pelvic girdle are examined to determine the origin of symptoms and plan appropriate management. Causes of lumbopelvic pain appear multi-factorial and may include postural adaptations, fatigue, increased joint mobility, increased collagen volume causing pressure on pain-sensitive structures, weight gain and pressure from the growing fetus (Haslam 2004b). The main risk factors are a history of previous lumbopelvic pain and/or previous trauma to the pelvis and possibly a high workload and multiparity (Berg et al. 1988; Ostgaard and Andersson 1991; Kristiansson et al. 1996a; Larsen et al. 1999; Vleeming et al. 2004). Others may include pelvic girdle pain in a previous pregnancy (Larsen et al. 1999), poor workplace ergonomics and awkward working conditions (Larsen et al. 1999), abdominal sagittal and transverse diameters and a naturally large lumbar lordosis (Ostgaard et al. 1993), and also a decreased fitness level before pregnancy (Ostgaard et al. 1993). Factors not associated with PGP include contraceptive pill use, time interval since last pregnancy, height, smoking, age and breastfeeding (Berg et al. 1988; Kristiansson et al. 1996b; Larsen et al. 1999). Reported musculoskeletal factors contributing to pregnancy-related PGP include the pelvic girdle joints moving asymmetrically (Damen et al. 2001), symphyseal laxity (Björklund et al. 1999) and ligamentous strain and muscle weakness (Mens et al. 1996). PGP is probably caused by a combination of these factors plus altered activity in the spinal (Sihvonen et al. 1998), abdominal, pelvic girdle, hip (Pool-Goudzwaard et al. 1998) and pelvic floor muscles (Pool-Goudzwaard et al. 2005) leading to abnormal pelvic girdle biomechanics and stability. However, a small number of women might have non-biomechanical but hormonally-induced pain in the pelvic girdle. Symphysis pubis dysfunction (SPD) relates to pain in the region of the symphysis pubis joint whereas diastasis symphysis pubis (DSP) is a true separation of the symphysis pubis joint confirmed radiologically. The definition of DSP is symphyseal separation of more than 10 mm and vertical shift of more than 5 mm (Hagen 1974). The amount of symphyseal separation does not always correlate with symptoms (Snow and Neubert 1997) and not all symptomatic patients have an increased gap. SPD or DSP may occur antenatally, during delivery or postnatally, and might cause severe social difficulties (Fry 1999). Trauma to the symphysis pubis may occur during a difficult delivery where forceful and excessive abduction of the thighs is necessary (Capiello and Oliver 1995; Gherman et al. 1998; Heath and Gherman 1999; Kharrazi et al. 1997; Albert et al. 2001). Pain distribution may be in the groin, medial and anterior thighs, perineum, coccyx, and one or both sacroiliac joints (Fry 1999; Coldron 2005). Severity and irritability vary from mild to severe and may differ day-to-day. Common physical signs are pain on thigh abduction, turning in bed, lifting a light weight, getting up from a chair and using stairs, a shuffling or waddling gait, severe symphyseal tenderness and an inability to weight-bear unilaterally (Fry 1999; Hansen et al. 1999). Self-reported pain locations in the pelvis, a positive posterior pain provocation test and a sum of other provocation tests (compression/distraction; Patrick-Faber test; palpation of the symphysis pubis; palpation of the long dorsal ligament) were significantly associated with disability and pain intensity in late pregnancy (Robinson et al. 2010). Furthermore, distress was significantly associated with disability. The active straight leg raise (ASLR), fear-avoidance beliefs and the number of pain sites were not associated with pain and disability. Minor trauma, such as stepping down from a kerb, may cause severe symphysis pubis pain. A forward rotation and oblique slip of the innominate caused by overactivity in the adductor muscles of the thigh may contribute to SPD (Röst 1999). With poor use of the glutei and lack of force closure of the pelvis, disruption of the self-locking mechanism of the pelvis may occur. Proposed non-musculoskeletal factors for PGP include increased hyaluronidase (Schwartz et al. 1985), oral contraceptives (Wreje et al. 1997) – although this is disputed by Björklund et al. (2000b) – and genetic susceptibility (MacLennan and MacLennan 1997). The role of relaxin in production of pregnancy-related lumbopelvic pain is controversial with some evidence suggesting an association between relaxin and PGP (MacLennan et al. 1986b; Kristiansson et al. 1996b) while other evidence shows none (Albert et al. 1997; Björklund et al. 2000a). Relaxin levels are at their highest during labour but fall to almost non-pregnant levels by three days postpartum (MacLennan et al. 1986a). As many women experience postpartum lumbopelvic pain, other reasons apart from serum relaxin levels probably contribute. Conclusive association between new-onset postpartum backache and epidural analgesia has not been demonstrated (Breen et al. 1994; Russell et al. 1996; MacArthur et al. 1997; Howell et al. 2002; Loughnan et al. 2002) though its masking effect on pain may lead to women adopting unsuitable positions in labour (MacArthur et al. 1990). It is important to acknowledge that pregnancy-related lumbopelvic pain is a common, recognised condition, which is better managed with prompt identification, assessment and appropriate treatment. If left untreated it may last more than two years (Albert et al. 2001). Antenatal education on posture and back pain by a physiotherapist has been shown to reduce back and pelvic pain, reduce sick leave and continue to benefit women in the postnatal period (Noren et al. 1997). Antenatal advice includes adopting comfortable resting positions; moving out of bed, a chair or the car; postures in walking and standing; and correct lifting and handling. In addition, postnatal advice includes positions for breastfeeding, nappy changing, bathing and handling the growing baby. Woman may be advised to (ACPWH 2010a): • remain active within the limits of pain; • accept offers of help and involve partner, family and friends in daily chores; • consider alternative sleeping positions; • explore alternative ways to climb stairs; • avoid activities that involve asymmetrical positions of the pelvis; • consider alternative positions for intercourse; • organise hospital appointments for the same day if possible; • avoid activities which make the pain worse (e.g. vacuuming, pushing a supermarket trolley, lifting heavy weights). Liaison with midwives is essential. Women should be aware of the masking effect of epidural and spinal anaesthesia in relation to excessive abduction of hips during labour and delivery. If possible, they should adopt the most comfortable position during labour (for example left-side-lying, or kneeling upright with support). They should be discouraged from placing their feet on attendants’ hips and care should be taken if lithotomy is required (ACPWH 2010a). Suturing should take place in the most comfortable position for the mother. There is some evidence that pregnancy-related lumbopelvic pain may respond to manual therapy (Daly et al. 1991; Diakow et al. 1991; McIntyre and Broadhurst 1996), and correct assessment of the spine and pelvic girdle is imperative to enable treatment to be targeted at the correct structures. Providing severity and irritability has been properly assessed, many manual therapy techniques in use in the non-pregnant population can be used and adapted for women with pregnancy-related lumbopelvic pain. Many can be undertaken with the woman in side lying. Management depends upon whether there is movement limitation caused by a true articular restriction, or the joint is held in an abnormal position by imbalance or altered recruitment of the muscles (Lee and Vleeming 2000). Lee (1999) recommended that articular restrictions be treated first with mobilisation or manipulation techniques followed by treatment of myofascial structures using muscle energy techniques (MET). Other techniques for treating myofascial dysfunctions include trigger points, strain/counterstrain, positional release, soft tissue manipulation techniques or taping to offload overactive muscles. Unilateral or bilateral muscles that may be overactive with PGP are the hip adductors, psoas, piriformis, erector spinae and quadratus lumborum. Tightness may be palpated in the posterior fibres of the pubococcygeus. With SPD, special attention should be paid to overactive pelvic adductors, underactive abductors, unilateral displacement of one innominate bone (Röst 1999) and poor pelvic girdle and spinal stabilising muscles. The use of a sacroiliac/trochanteric belt for sacroiliac and symphysis pubis instability both ante- and postnatally may stabilise the pelvic girdle joints (Damen et al. 2002; Mens et al. 2006) and substitute the work of the internal oblique muscle (Snijders et al. 1998) but its effect on pain is equivocal (Depledge et al. 2005). However, a belt should be tried if ASLR test is positive. A large tubular bandage for the abdomen or a maternity belt may give added support. In the most severe cases crutches or a wheelchair may be required. Abdominal, spinal and pelvic girdle muscle motor control needs to be retrained to stabilise an unstable spinal segment or pelvic girdle joint. Specific spinal and pelvic girdle stabilising programmes are effective in reducing pain antenatally (Elden et al. 2005) and postnatally (Stuge et al. 2004a, 2004b, 2006). Rehabilitation exercises antenatally and postnatally should concentrate initially on correct recruitment and strength training of both pelvic girdle stabilising muscles (gluteus medius and maximus) and core lumbopelvic stabilising muscles (transversus abdominis, lumbar multifidus, pelvic floor muscles). Poor recruitment and decreased strength of hip adductors and flexors have been shown to be a factor in pregnancy-related PGP (Mens et al. 2002), and altered recruitment of gluteus maximus has been shown in patients with sacroiliac joint (SIJ) pain. No studies of gluteus medius in pregnancy-related PGP have been undertaken, but the waddling gait of these patients is a common sign and is probably a result of poor gluteus medius control. It is proposed that the main muscles to be targeted in women with PGP are the trunk core stability muscles, as described above, plus the hip abductors, adductors, flexors and extensors. Consideration of the balance between adductors and abductors should be given owing to their function in providing stability across the symphysis pubis (Lee 1999). Exercise for global stabilising muscles, such as the oblique abdominals, erector spinae, latissimus dorsi and iliopsoas should follow as pain and physical ability allows. The role of RA in lower abdominal strength and support should not be ignored as Coldron et al. (2008) found that characteristics of RA shape and size had not returned to normal values by 12 months post-partum. A thinner, wider and longer RA has implications for strength and fascial support, and may cause decreased stiffness of the anterior abdominal wall and predispose to a mechanical disadvantage. Exercises that target the return of normal RA width, thickness (strength) and length without loading and compressing the lumbar spine are required. The consequences of a persistent diastasis rectus abdominis (DRA) are not known fully but a relationship between DRA and diagnoses of stress urinary incontinence, faecal incontinence and pelvic organ prolapse has been shown (Spitznagle et al. 2007). It is also possible that the mechanical advantage of the two RA bellies is compromised and thus could affect muscle strength and potential development of lumbopelvic pain. The IRD should resolve to approximately 20 mm by 8 weeks postpartum (Coldron et al. 2008) which approximates to 1–2 finger widths. However, in some women the IRD does not return to normal values by 12 months postpartum (Coldron et al. 2008) and, together with the changes to RA, anterior abdominal wall stiffness is likely to be compromised. Physiotherapists should examine the postnatal gap between the recti at the level of the umbilicus and assess the IRD. If there appears to be a persistent DRA (>3 finger widths) advice regarding exercise should be given, including initial training of the deep abdominal muscles (TrA) (Sheppard 1996; Potter et al. 1997a), gentle exercises to strengthen RA while avoiding strong trunk curling exercises to prevent herniation of abdominal contents. In a small study, the occurrence and size of DRA in pregnant women was found to be much greater in non-exercising pregnant women than in those who exercised (Chiarello 2005) supporting the view that good fitness pre-pregnancy is of benefit to the woman. There is increasing evidence that acupuncture is effective in relieving antenatal lumbopelvic pain (Wedenberg et al. 2000; Ternov et al. 2001, Guerreiro da Silva et al. 2004; Kvorning et al. 2004; Elden et al. 2005; Lund et al. 2006) and recent evidence suggests that acupuncture has no observable adverse effects on the pregnancy, mother, delivery or the fetus/neonate (Elden et al. 2008). Some experts advise that it is avoided in the first trimester (Forrester 2003) and acupuncture points that have been traditionally associated with abortion (miscarriage) should also be avoided (Betts 2003; West 2008), though this latter point is controversial as no adverse effects have been reported. The use of TENS antenatally for pain relief is controversial owing to concerns about fetal malformations and spontaneous abortion, but no negative effects have been reported from the use of TENS during any stage of pregnancy (ACPWH 2007). Therefore, its use in pregnancy for lumbopelvic pain could be justified provided the usual precautions and contraindications are observed, the current density is kept low, large electrodes are used, electrodes are not placed over the abdomen and acupuncture points thought to induce labour are avoided. Although the evidence for pain relieving effects of TENS is equivocal (Khadilkar et al. 2008) it poses less risk than most analgesic medicines, so could be tried. Many women exercise regularly and wish to continue during pregnancy. Some women take up exercise for the first time, and exercise should be encouraged during pregnancy (RCOG 2006). Special guidelines for safe activity and exercise in pregnancy exist for women with weight-management problems, diabetes and pre-eclampsia (CMACE/RCOG 2010; NICE 2010a). Health professionals should use any appropriate opportunity to provide information about the health benefits of losing weight before becoming pregnant to women with a body mass index (BMI) ≥30. This should include information on the increased health risks their weight poses to themselves and would pose to their unborn child. Research suggests that mild-to-moderate exercise is beneficial to healthy pregnant women (Clapp 2000) and is not harmful to the fetus (Clapp et al. 2000; Riemann and Kanstrup Hansen 2000; ACOG 2002; Arena and Maffulli 2002). Moderate intensity is defined as being able to talk easily, while increasing the heart rate to a maximum of 140 beats per minute. Choice of exercise must be influenced by the physiological changes which will occur (Artal and O’Toole 2003). For example, plasma volume increases before red cell volume, leading to a decreased ability to provide oxygen in response to demand. Also, increased demand causes raised respiratory rates, cardiac output values increase during pregnancy for the same activity (over the non-pregnant woman) and there is a loss of cardiac reserve. Potential benefits of exercise include: • maintenance of cardiovascular fitness; • maintenance of healthy weight range; • improvement of body awareness, posture, co-ordination and balance; • increase in endurance and stamina; • provision of social interaction with exercise, enhancing feelings of social and emotional well-being; • possible reduction in problems during labour and delivery; • possible prevention of gestational diabetes; • reduction in minor complaints of pregnancy;
Physiotherapy in women’s health
Anatomy and physiology
Bones and joints of the pelvis
Muscles
Organs of reproduction
The physiology of pregnancy
Musculoskeletal changes during pregnancy
Postural changes
Articular and connective tissue changes
Neuromuscular changes
Rectus abdominis
Lateral abdominal muscles
Pelvic floor muscles
Labour, birth and the puerperium
Labour
Stages of labour
First stage
Second stage
Pain relief
Episiotomy
Assisted birth
Induction
Puerperium
Physiotherapy in the childbearing year
Pelvic floor dysfunction
Pregnancy-related lumbar spine and pelvic girdle pain
Symphysis pubis dysfunction
Diagnosis of PGP
Non-musculoskeletal causes of PGP
Management of lumbopelvic pain and dysfunction
Advice, posture, education and general exercise
Treatment of articular dysfunctions/movement restriction of the spine and pelvic girdle
Muscle re-education
Management of diastasis rectus abdominis
Pain management
Exercise and pregnancy
General issues
Benefits and contraindications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Physiotherapy in women’s health