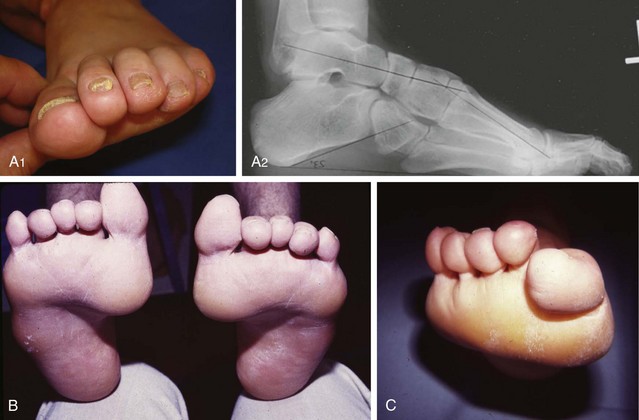
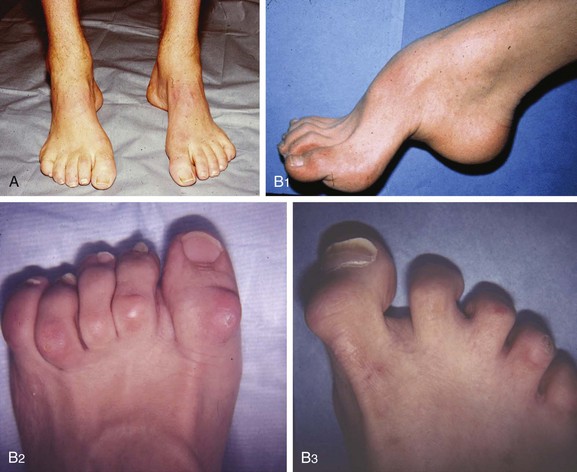
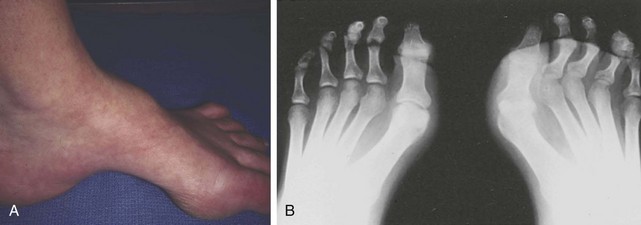
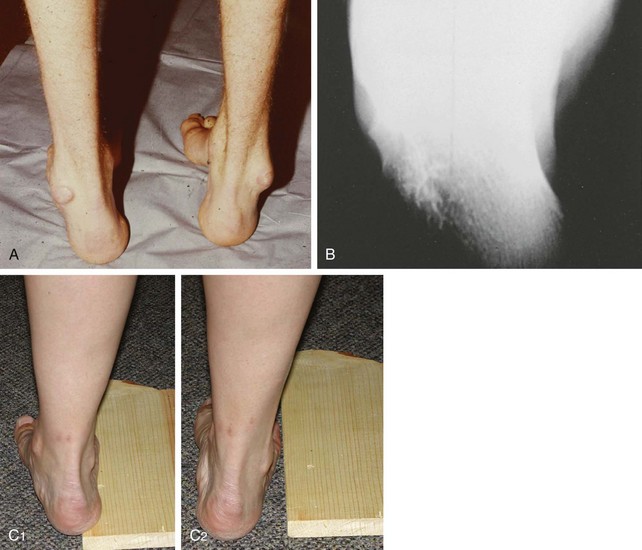
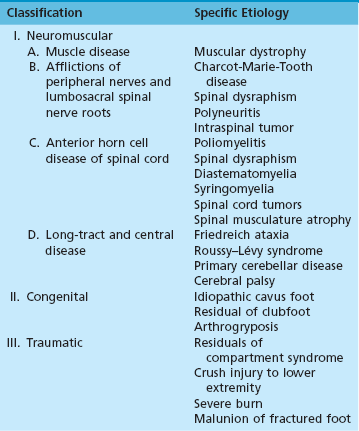
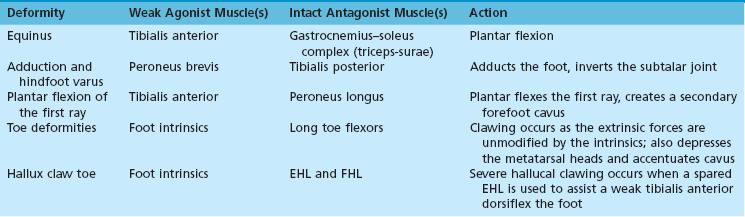
Chapter 26 Although the specific etiology of any cavus foot varies with the disease process, all forms result from muscle imbalance. Historical attempts to attribute all forms of cavus foot to a single neurologic lesion have proven overly simplistic. Bentzon2 and Hallgrimsson16 in 1939 proposed that extrinsic muscle imbalance underlay all deformities. In 1959, Duchenne9 subsequently proposed that the deformity results from an imbalance between the extrinsics and the intrinsics. Neither approach is fully satisfactory; a cavus foot is best thought of as an end result that a variety of subtle neurologic lesions can produce. Brewerton et al5 specifically looked at the cause of pes cavus in a series of 77 patients and found subtle neurologic defects in 66% of them, leaving a large group of “idiopathic” cases. Of these, 11 of the 26 patients had a family history of pes cavus, and 7 of the 26 had nonspecific abnormalities upon electromyographic and nerve conduction velocity examination. Most cases of idiopathic pes cavus likely represent a very subtle neurologic lesion that is below clinical detection. Roughly half of the detectable lesions are variants of Charcot-Marie-Tooth disease, but a host of other less common conditions can also be discovered (Table 26-1).19 Table 26-1 Modified from Ibrahim K: Pes cavus. In Evarts CM, editor: Surgery of the musculoskeletal system, New York, 1990, Churchill Livingstone, pp 4015–4034. Charcot-Marie-Tooth disease (CMT) should at least be considered in every patient who presents with pes cavus. CMT is not, in fact, a single disease but rather a heterogeneous group of disorders caused by inheritable defects in any of several constituent proteins of the myelin sheath of peripheral nerve. The disorder was described in general terms by the great French neurologist Jean Martin Charcot and his pupil Marie in 1886 and independently by Tooth in England later that year.6,44 Originally, Charcot attributed the disorder to a spinal defect, and it was Tooth’s subsequent work that correctly classified it as a peripheral nerve disorder. The disease is the most common inheritable defect of peripheral nerves, but approximately half of the time it represents a new sporadic chromosomal recombination error. The nomenclature associated with CMT is confusing because of the historical lack of understanding of its cause. The archaic term peroneal muscular atrophy (PMA) was supplanted by Dyck and Lambert, who developed an extensive classification of inheritable motor neuropathies based upon their electrodiagnostic patterns in the 1960s and 1970s.12 Their scheme refers to a series of seven hereditary motor sensory neuropathies (HMSN-I through HMSN-VII). Since 1990 there has been an explosion of understanding of the specific genetic defects underlying the CMT disorders,4 leading to a new and still evolving reclassification of the disease. CMT-1C represents the small remainder of CMT-1 patients in whom the genetic defect is still unknown. The foot deformities in CMT do not result from absolute weakness of the motor units powering the foot but of their relative imbalance. Initiation of the deformity likely results from an imbalance of the failing foot intrinsics and the preserved extrinsics.3 Subsequently, a specific pattern of extrinsic motor weakness is common in CMT in which the anterior and lateral compartment musculature is selectively affected, with certain curious exceptions. The disease almost always affects the peroneus brevis but spares the peroneus longus. This was first observed clinically by Mann and Hsu33 and subsequently confirmed by Tynan et al,45 who demonstrated that the cross-sectional area of the peroneus longus was preserved on magnetic resonance imaging (MRI) of patients with the disease. An additional oddity can be observed in the anterior compartment musculature; the extensor hallucis muscle can be spared while the anterior tibialis is affected. This occurs despite the more distal location of the extensor hallucis longus (EHL) and their shared peroneal innervation. The reasons for the unusual patterns of motor weakness in CMT remain poorly understood. The selective denervation affects certain muscles in the anterior and lateral compartments, and only very late posterior compartment involvement is seen. Denervation in CMT progresses very differently from a classic symmetric polyneuropathy, such as that encountered in diabetes. At least some speculation has been centered upon the possibility that some element of nerve compression can play a role.14 Regardless of the cause of the patterns of weakness, each of the deformities of the disease can be explained in the form of a weak agonist muscle and a more normally functioning antagonist (Table 26-2). There is no evidence of spasticity in the motor units that remain innervated. Table 26-2 Foot Deformities in Charcot-Marie-Tooth Disease EHL, extensor hallucis longus; FHL, flexor hallucis longus. From Guyton GP, Mann RA: The pathogenesis and surgical management of foot deformity in Charcot-Marie-Tooth disease, Foot Ankle Clin 5:317–326, 2000. It is rare in clinical practice to encounter a patient at such an early stage of disease that the foot is entirely supple with no hindfoot or forefoot contractures. However, rebalancing the foot through tendon transfers can help prevent the development of further deformity if it is done early enough.38 For instance, the overpull of the peroneus longus that forces the forefoot into cavus can be eliminated by transferring the tendon to the peroneus brevis. This also serves to help oppose the tibialis posterior and prevent adduction. The emphasis in early-stage surgery on CMT should be on tendon transfers rather than lengthening motor units. Because the long-term outcome of CMT is one of progressive, inexorable weakness, strength should be preserved whenever possible. The last great epidemic of polio in the United States occurred in New England in 1955. Although the residual effects of the disease are now encountered with increasing rarity, it still serves as a useful model of a process that can produce either a forefoot cavus or a hindfoot cavus.8 Friedreich ataxia is a familial progressive ataxia in which posterior column function is steadily lost.36 It occurs in an autosomal recessive form with an earlier age of onset (11.75 years) and in a dominant form with a later age of onset (20.4 years). No cases of onset after the age of 25 have been reported. The disease is usually associated with pronounced and progressive symmetric cavus foot deformities with severe claw toe formation. In numerous instances, the foot deformities have been the presenting complaint. Roussy-Lévy syndrome is a rare syndrome of cavus foot, sensory ataxia without obvious long-tract signs, peripheral motor atrophy, and kyphoscoliosis. Because it shares characteristics of both diseases, it was poorly differentiated from Friedreich ataxia and CMT for many years.37 The onset occurs very early in childhood and runs a relatively benign course. Spinal muscular atrophy is a heterogeneous group of disorders that are usually present from birth but have some late-onset forms.41 They are characterized by an inexorably progressive loss of anterior motor neuron cells. The disorders are characterized by hypotonia and can be associated with the cavus foot deformity, although it is rarely the presenting feature. The cavus foot deformity is one of four components of the congenital clubfoot, easily remembered by the mnemonic CAVE (cavus, adductus, varus, equinus). Adult clubfoot residuals encountered after childhood casting usually result from a failure of early casting to adequately elevate the first ray before abducting the foot about the fulcrum of the talar head as described by Morcuende et al.35 The most severe deformities that result from improper casting technique are usually not those of residual cavus but of a rocker-bottom foot that results when the equinus is inappropriately corrected while the calcaneus remains locked under the talus; the foot then dorsiflexes through the midfoot rather than through the ankle. A wave of enthusiasm for surgical clubfoot correction in the 1970s and 1980s is also now yielding residual effects in the adult foot and ankle population. The results of clubfoot correction surgery have proved to be substantially less reliable than once thought.30,42 A patient presenting with problems with a postsurgical clubfoot is just as likely to have overcorrection into planovalgus as residual undercorrection in cavovarus. The one constant in the surgically corrected clubfoot is a remarkable amount of stiffness in adults. In a dynamic gait analysis study, Huber and Dutoit18 specifically identified late subtalar stiffness as the primary feature associated with a poor result after childhood clubfoot surgery. It is rare that anything short of triple arthrodesis can be entertained to address the residual complaints. Pes cavus must be viewed as a spectrum of deformities in which the underlying abnormality is that of an elevated longitudinal arch, but after that a variety of bony and soft tissue deformities can be present. The spectrum can range from a mild cavus foot, with flexible claw toes as the only significant clinical problem, to a severe fixed deformity, with altered weight bearing, callosities, lateral ankle laxity, stress reactions, and pain. The shape of the foot varies with the cause and duration of the motor imbalance that created the deformity. When muscular imbalance in pes cavus begins before maturation of the skeleton, there can be substantial change of healthy osseous morphology. After skeletal maturity, there is usually little or no change in the morphology.1 The cavus foot is best understood by systematically analyzing the bone deformities, the soft tissue deformities, and the specific muscle functions that are imbalanced. The bony deformity may be predominantly in the hindfoot, the forefoot, or a combination of both. A hindfoot cavus describes an elevated pitch of the long axis of the calcaneus, which is usually greater than 30 degrees in a cavus foot (Fig. 26-1). Hindfoot cavus was a very common deformity in the era of widespread poliomyelitis; the focal nature of the disease in the anterior horn cells of the spinal cord often led to gastrocnemius weakness but sparing of the tibialis anterior and often the foot intrinsics. The resultant imbalance of forces then often led to dramatic calcaneal pitch angles and subsequent soft tissue contractures. Pure hindfoot cavus is now less common, while hindfoot varus is a predominant finding in pes cavus with underlying neurologic disease. Elevated calcaneal pitch is still encountered as a component of a combined deformity in the idiopathic cavus foot with no clear neurologic cause. Figure 26-1 Pes cavus with a predominant hindfoot deformity. Note the dramatically high pitch angle of the calcaneus. Most neurologic cavus deformities are thought to occur from a forefoot-driven hindfoot varus resulting from a muscle imbalance as in CMT. The peroneus longus tendon is a direct antagonist to the tibialis anterior tendon. Often spared by the neuropathy, the strong peroneus longus muscle overpowers the affected tibialis anterior and initializes the deformity by plantar flexion of the medial forefoot (Fig. 26-2). The tibialis posterior muscle induces the hindfoot varus, and the Achilles tendon further enhances the varus stress secondary to the plantar-flexed first ray and varus heel alignment, which alters the transmission of axial forces through the ankle joint. With inversion of the hindfoot, the lateral foot supinates and the peroneus longus muscle further plantar flexes the first ray to restore the tripod position and a plantigrade foot.1 Soft tissue contracture converts a flexible to a fixed cavus deformity over time. Toe deformities are thought to occur from early degeneration of the intrinsic muscles of the foot. Because the lumbricals are not acting to stabilize the metatarsalphalangeal (MTP) joint (intrinsics effect: MTP flexion, proximal interphalangeal [PIP] and distal interphalangeal [DIP] extension), the unopposed extensor digitorum longus hyperextends the unstable lesser toes at the MTP level while the flexor digitorum longus and brevis flex the phalanges.1 The plantar-flexed metatarsal heads and plantar fascia shortening amplify forefoot plantar flexion. The deformities might be as mild as flexible clawing of the MTP joints in association with mild flexion of the interphalangeal joints, or they can manifest as fixed claw toe deformities. Once severe fixed claw toe deformities are present, the forces from the extrinsic toe extensors serve to hold the metatarsal heads in a plantar-flexed position (Fig. 26-3). Of importance, the plantar fat pad is displaced distally in severe cases as the toes pull up into extension. Not only are the metatarsal heads driven plantarward by the deformity, but they are also deprived of their normal cushioning layer of fat. The plantar fascia commonly develops a contracture with time in all forms of cavus foot. It is anatomically much thicker on the medial aspect of the foot, and as the contracture develops, it not only holds the longitudinal arch in an elevated position but also holds the forefoot adducted and keeps the calcaneus inverted (Fig. 26-4). Although some bony procedures can secondarily relax the plantar fascia by altering the shape of the arch, they are not always adequate by themselves. Early in the development of many cases of forefoot cavus the deformities remain relatively flexible. The arch might not flatten while standing, but muscle forces are holding it in position rather than bone and joint contractures. This is typical, for instance, of a very young patient with Charcot-Marie-Tooth disease. The subtalar joint compensates for the forefoot deformity by falling into a varus alignment (Fig. 26-5). As the disease progresses, the capsule and interosseous ligament of the subtalar joint become contracted, and the once-flexible hindfoot deformity becomes fixed. The mechanics of all variants of the foot are similar. The axes of the talus and the calcaneus are more collinear. The talar head remains over the anterior process of the calcaneus, and the navicular moves to a superior instead of a medial position to the cuboid; the subtalar joint axis is more vertical; and the Chopart joint function is impaired.1 When the hindfoot is locked in inversion, there is less subtalar and transversal tarsal motion during gait than in the normal foot. The ability of the foot to absorb the impact of walking by pronation during the early part of stance phase is diminished, and the first metatarsal head and the lateral border of the foot are overloaded.1 A cavus foot is always stiffer than one of normal conformation. The relative dorsiflexion of the talus within the ankle mortise is caused by plantar flexion of the medial forefoot, limits ankle dorsiflexion, and is accompanied by anterior ankle impingement. Together with the hindfoot varus position, relative talus dorsiflexion is thought to contribute to an increased anteromedial contact stress in the ankle joint. The association between lateral ankle instability, cavovarus deformity, and ankle arthritis has been discussed in the literature.13,46 A significant pressure increase and reduction of the area loaded in the ankle joint was also demonstrated in simulated pes cavus and is considered to lead to ankle arthritis in long-standing deformities with, but also without, lateral ligament instability.24
Pes Cavus
Etiology
Charcot-Marie-Tooth Disease
Poliomyelitis
Other Neurologic Lesions
Congenital Pes Cavus
Clubfoot Residuals
Evolution of Deformity

Biomechanical Consequences of Pes Cavus
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine