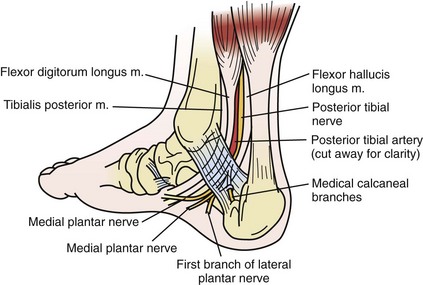
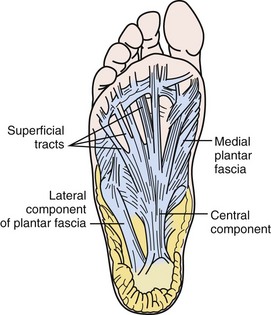
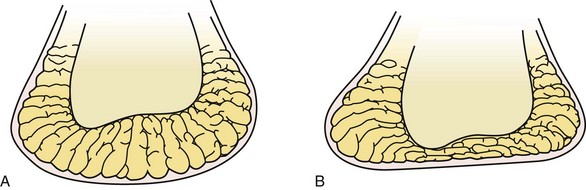
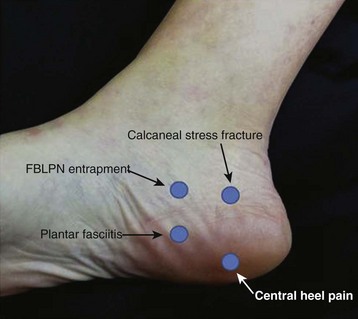
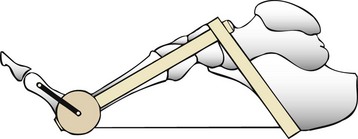
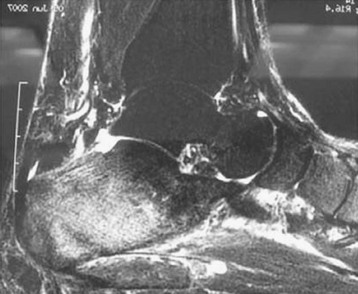
Chapter 13 PATIENT HISTORY AND PHYSICAL EXAMINATION IMAGING AND OTHER DIAGNOSTIC STUDIES Heel Fat Pad Atrophy Treatment Authors’ Preferred Nonoperative Treatment for Plantar Fasciitis Early examiners suggested an infectious origin for heel pain. In the 1930s, they proposed that tuberculosis, streptococcal, gonorrhea, and syphilis infections caused heel pain.13 Dedicated research refuted the infectious etiology of heel pain, and efforts were made to find a mechanical source. With the evolution of x-ray technology, emphasis placed on the heel spur as the source of heel pain gained momentum. Steindler and Smith66 (1938) performed rotational osteotomies to move the spur from the weight-bearing surface. In 1957, DuVries27categorized the different morphology of calcaneal spurs and their impact on heel pain. Contrary to these thoughts, the spurs did not lie within the plantar fascia but dorsal to it. Cadaveric studies confirmed the presence of the spur within the flexor digitorum brevis as well as within the abductor hallucis (Fig. 13-1).30 In the 1960s, after performing a cadaveric dissection study, Tanz67 proposed nerve entrapment as cause of heel pain (Fig. 13-2). He discovered that a branch of the lateral plantar nerve passes around the medial border of the heel and innervates the abductor digiti quinti muscle. Baxter and Thigpen later elaborated on this and demonstrated how the first branch of the lateral plantar nerve (FBLPN) becomes entrapped, resulting in plantar heel pain.7 Although we do not often find heel pain attributed to isolated nerve pain, these early concepts and research laid the foundation of our current understanding of the anatomy, mechanisms, and causes of plantar heel pain. Figure 13-1 A large heel spur is seen on the calcaneus with extension into the flexor digitorum brevis. Although the exact incidence of plantar heel pain is unknown, it is estimated that more than 2 million patients receive treatment for plantar fasciitis each year in the United States.50 Approximately 1 in 10 people will develop heel pain during their lifetime,18 and 1% of all visits to orthopaedic surgeons are thought to be for heel pain.56 In a 2009 study, Scher et al61 reported a 12% incidence of plantar fasciitis in a young, active-duty military service–member population. An increased risk of plantar fasciitis has been associated with decreased ankle dorsiflexion, workers who spend prolonged periods of the day on their feet, runners, and individuals with a body mass index greater than 30 kg/m2.55 These studies demonstrate not only the significant number of patients impacted but also the wide range of ages within the adult population affected by plantar heel pain. The plantar fascia is composed of bands of fibrous tissue that originate on the anteromedial aspect of the calcaneal tuberosity and insert on the bases of the proximal phalanges. Strong vertical septa divide the medial, central, and lateral portions of the plantar fascia and create three distinct compartments of intrinsic plantar muscles. The three bands of fascia spread into a broad sheet as they course distally and divide into five digital bands at the metatarsophalangeal (MTP) joints (Fig. 13-3). Each digital band divides to pass on either side of the flexor tendons and inserts into the periosteum of the base of the proximal phalanges. Fibers of the plantar fascia also blend with the dermis, transverse metatarsal ligament, and flexor tendon sheath.68,71 As the plantar fascia courses distally from its origin deep to the plantar fat pad of the heel, it becomes subcutaneous and is easily palpated beneath the longitudinal arch along the plantar aspect of the foot. The plantar fascia is relatively inelastic. Postmortem studies found a maximum elongation of 4%, with failures in the tissue occurring at 90 kg of force at the clamp margins.72 The fascia itself requires more than 1000 N to fail.39 Tension along the plantar fascia develops when the toes dorsiflex during the stance phase of gait, which transmits tensile loads to its calcaneal origin. The transmission of this tensile load elevates the longitudinal arch, referred to as the windlass mechanism. Because of its inelastic properties, high tensile forces are concentrated on the origin of the plantar fascia during the push-off phase of gait, with dorsiflexion of the MTP joints via the windlass mechanism. In addition, the gastrocnemius-soleus complex pulls simultaneously and concentrates additional body weight onto the forefoot while the downward acceleration of the body concentrates an additional 20% increase in the ground reaction forces.49 Repetitive activation of the windlass mechanism, as one might see in runners or standing workers, may result in tensile overload, microtears, inflammation, and chronic degenerative changes in the plantar fascia origin.8,9 The anatomy was first described by Teitze in 1921.51 The structure is a honeycombed pattern of fibroelastic septa that completely enclose fat globules (Fig. 13-4). The closed-cell structure of the fat pad provides the mechanical integrity for its shock-absorbing function. The tissue septa are U-shaped around the tuberosity and anchored to the calcaneus and skin. Elastic transverse and diagonal fibers that separate the fat into compartments reinforce the chambers internally. The fat pad on the calcaneus functions as an important cushion to the hindfoot. A typical healthy man has a gait velocity of approximately 82 m/min and a cadence of 116 gait cycles/min.59 Each heel strike generates 110% of body weight but can concentrate up to 250% of body weight with running. After approximately age 40 years, the fat pad begins to deteriorate; with the loss of collagen, elastic tissue, and water, the overall thickness and height of the fat pad decrease. These changes result in softening and thinning of the heel fat pad, decreased shock absorbency, and reduced protection of the heel tuberosity.37 Approximately 50% of patients with heel pain have heel spurs.65 Shmokler et al64 found a 13.2% incidence of heel spurs in 1000 patients chosen randomly, and only 5.2% of the total patients with heel spurs reported any history of heel pain. Williams et al71 found that 75% of patients who had heel pain also had spurs, compared with 63% of patients who had no heel pain. Although heel spurs can occur with heel pain, they are not considered the cause. From a histologic perspective, plantar fasciitis is a fibrofatty degeneration of the plantar fascia origin with microtears and collagen necrosis.43 This likely represents a degenerative process, more so than an inflammatory one unless the patient has an associated spondyloarthropathy, such as ankylosing spondylitis. Although some authors believe the thickness of the fat pad is the single most important determinant in heel pain,37 other authors have actually found an increased thickness of the fat pad in patients with heel pain.4 The elasticity of the heel fat pad may be more important than the actual thickness. Prichasuk found that heel pad elasticity is reduced in patients with heel pain and that the elasticity decreases with increasing age and body weight.54 More fat in a closed space, combined with loss of elasticity of septa, might increase pressure on the calcaneal tuberosity.54 A thorough history and physical examination will most often guide the clinician to the appropriate diagnosis and treatment plan. The differential diagnosis for plantar heel pain includes proximal plantar fasciitis, calcaneal stress fractures, tumors, infections, disorders of the fat pad, midplantar fascia strain, plantar fibromatosis, flexor hallucis tendinitis, and nerve entrapment of the posterior tibial nerve (Table 13-1). Table 13-1 Differential Diagnosis for Plantar Heel Pain Plantar fasciitis with entrapment of the FBLPN Enthesitis: spondyloarthropathies Flexor hallucis longus tendonitis Clinicians should first review the patient’s general health, including a treatment history for the heel pain (e.g., therapy, medications, injections, orthoses, or surgeries). Constitutional symptoms, such as weight loss, fevers, chills, and night sweats, should lead the clinician to investigate a systemic condition. Further questioning should focus on the patient’s activities, both recreational and occupational. Specifically, one should inquire about a change in weight or activity coincident with the onset of symptoms. In addition, the amount of time spent weight bearing throughout the day is a causative and provocative factor.56 Unrelenting pain at rest or night pain is a red flag that the pain may be related to a tumor or an infectious process. Bilateral heel pain, especially in a younger patient, suggests a systemic process, such as ankylosing spondylitis, Reiter syndrome, or other seronegative spondyloarthropathies.45 A neuritic, dysesthetic type of pain is likely caused by nerve compression and irritation that can occur at rest. Pain occurring after an acute injury is more likely a plantar fascia rupture or acute fracture within the hindfoot. Patients with ruptures of the plantar fascia often have a history of corticosteroid injection.1,62 Paradoxically, these patients can have less pain after rupture of the plantar fascia, although there can be a subtle collapse of the longitudinal arch. The diagnosis of proximal plantar fasciitis is made by the patient’s history of symptoms along with physical examination findings. Patients usually complain of heel pain that is most notable upon the first steps in the morning or after sitting for an extended period of time. The pain starts with a sharp shooting quality that tends to change to an ache with continued ambulation. Having patients point to the location of their greatest area of pain can be helpful. Usually, they will point to the origin of the medial longitudinal arch at the medial tubercle of the calcaneus (Fig. 13-5). The patient is examined in a standing position to evaluate the hindfoot alignment and longitudinal arch. Achilles tightness is also assessed, with recent studies demonstrating 83% of plantar fasciitis patients have an equinus contracture, and 57% of these patients have an isolated gastrocnemius contracture.48 Patients with an acute plantar fascia rupture often describe an intense tearing sensation on the plantar surface of their foot. Most patients who sustain an acute rupture had prior symptoms of plantar fasciitis. In a 2004 review of 18 athletes treated for an acute rupture, 4 had received a prior corticosteroid injection for their plantar fascia pain. Twelve of the 18 injuries took place while running, with other activities including tennis, basketball, and soccer.60 A plantar fascia rupture diagnosis can be made based on physical examination findings, along with the patient’s description of the injury. Most patients will describe a “poplike” sensation on the bottom of their foot, with a rapid onset of intense pain. Clinical finding include the inability to perform a single-stance heel raise, pain with MTP extension, and focal plantar medial ecchymosis (Fig. 13-6). Treatment protocols vary but frequently include non–weight bearing for 2 to 3 weeks in a short-leg cast or removable cast boot. The use of ice, nonsteroidal antiinflammatory drugs (NSAIDs), orthotics, and gentle stretching is also used as the patient progresses. Although some reports describe high rates of return to activity and complete resolution of pain, other authors report a 50% rate of chronic pain and activity restriction postinjury.1,43 Figure 13-6 Plantar ecchymosis near the origin of the plantar fascia indicative of an acute plantar fascia rupture. TTS can be divided into proximal and distal TTS. Proximal TTS involves a compression neuropathy of the tibial nerve under the flexor retinaculum, and distal TTS involves compression to one or more of the terminal branches of the tibial nerve. Distal TTS frequently includes involvement of the abductor hallucis muscle’s deep fascia as a source of compression. With either proximal or distal TTS, patients complain of a burning or tingling element with their plantar heel pain. These symptoms can usually be reproduced by percussion over the distal course of the tibial nerve within the confines of the tarsal tunnel. An additional physical examination finding includes a pain with the “dorisflexion-eversion test” (dorsiflexion and eversion of the ankle in combination with full extension of the MTP joints). The “windlass test” (full extension of the all MTP joints, Fig. 13-7) also results in increased strain across the tibial nerve and plantar fascia, rendering both tests unreliable in determining whether plantar fasciitis or TTS is the etiology of a patient’s plantar heel pain.2 Calcaneal stress fractures must be considered and evaluated in the patient presenting with plantar heel pain. The patient’s history can assist in making the diagnosis by noting a significant increase in activity level after a former more sedentary lifestyle. Early on their heel pain can easily be confused with plantar fasciitis. Eventually, the pain is present throughout the day. Unlike plantar fasciitis, the pain continues to increase in intensity during weight bearing. The physical examination findings include a reproduction of pain with the calcaneal squeeze test (a medial-lateral compression of the calcaneal tuberosity, see Fig. 13-7), along with associated swelling. Confirmation of the diagnosis can usually be made with plain radiographs 2 to 3 weeks after the onset of symptoms.32 Central heel pain syndrome (or calcaneal fat pad atrophy) presents with a more central and proximal location of pain than the plantar fascia’s origin. Palpation of the fat pad reveals a softened and flattened surface. Erythema and inflammation can occur over the plantar aspect of the heel, a finding unique to this condition. The fat pad may be unstable from the underlying calcaneal tuberosity, with a concomitant bursitic reaction between the bone and the pad. Increased non–weight-bearing heel pad thickness and compressibility, which is equivalent to loss of heel pad elasticity, was significantly higher in the elderly population. These findings may account for the higher incidence of heel pain in older individuals.36 Diagnostic modalities such as radiographs, bone scans, ultrasound, or magnetic resonance imaging (MRI) are not usually necessary for the diagnosis or treatment of plantar fasciitis. However, they can be useful to exclude other mechanical diagnosis of plantar heel pain. Weight-bearing foot radiographs are obtained to rule out calcaneal stress fracture or hindfoot degenerative joint disease. Consideration can be given to obtaining both foot and ankle films in patients with previous trauma to determine if external sources such as exostosis are contributing to the patient’s symptoms. Computed tomography may also have a limited role in the patient with a prior history of trauma. Technetium bone scans have poor specificity and are rarely helpful in these patients. MRI is sensitive for detecting fascial ruptures, along with confirming the diagnosis of plantar fasciitis; it is most helpful in detecting space-occupying lesions of the tarsal tunnel and subtle calcaneal stress fractures or stress reactions (Figs. 13-8 and 13-9). Ultrasonography has also been used and is thought to be as reliable as MRI for the diagnosis of plantar fasciitis, but it is not as helpful with other pathologic sources of heel pain. In the setting of a neural component to the patient’s heel pain, electrodiagnostic studies can be performed to assist with ruling out associated pathology, such as radiculopathies and generalized peripheral neuropathy. Electromyographic results for the abductor hallucis or abductor digiti quinti are more likely to be abnormal in the setting of medial or lateral plantar nerve impingement than nerve conduction studies. Although a positive result adds confirmation to the clinician’s diagnosis, a negative result does not rule out the diagnosis of nerve compression because these studies have an accuracy of 90%.31 Because the neuritic component is believed to be a traction neuropathy most evident in dynamic situations, it is difficult to test with electrodiagnostic studies.41 Both rheumatoid arthritis and spondyloarthropathies can present with heel pain and positive findings on MRI, indicative of an inflammatory process of the plantar heel.28 Patients with recalcitrant unilateral or bilateral heel pain might suffer from a seronegative spondyloarthropathy, such as Reiter syndrome, ankylosing spondylitis, or psoriatic arthritis. Inflammatory bowel arthritis and Behçet syndrome can also manifest as heel pain. Gerster’s33 study of 150 patients with plantar fasciitis or Achilles tendinitis showed that 22% suffered from a seronegative spondyloarthropathy, and 91% tested positive for human leukocyte antigen-B27 (HLA-B27). When comparing this group with 220 patients having rheumatoid arthritis, Gerster rarely found plantar fasciitis in the rheumatoid arthritis group. Although 20% to 30% of patients can experience bilateral plantar fasciitis, clinicians should consider HLA-B27 testing in patients with bilateral heel pain with simultaneous onset or recalcitrant heel pain. Other helpful studies include complete blood count, erythrocyte sedimentation rate, rheumatoid factor, antinuclear antibodies, and uric acid. The overwhelming majority of patients with mechanical heel pain will respond favorably to nonoperative treatment. In plantar fasciitis, 6 to 10 months of treatment with conservative modalities results in a successful outcome for 90% of patients. As a result of the high success rate with nonoperative treatment, the American Orthopaedic Foot and Ankle Society (AOFAS) position statement recommends a minimum of 6 to 12 months of nonoperative treatment before surgical intervention is pursued for a diagnosis of plantar fasciitis.3 The efforts of nonoperative treatment are directed toward a reduction in pain, improved function, and shortened duration of symptoms. Although the number of different treatment options for plantar fasciitis are numerous, there are level I and II evidence studies available to assist in choosing the appropriate therapy. Isolated Achilles stretching was the primary objective of treatment for many years. There is evidence to show that 83% of patients with plantar fasciitis have an equinus contracture in either acute or chronic cases, making Achilles stretching a logical treatment choice.48 Although Achilles stretching is still used, more recent level I and II evidence in literature outlines a plantar fascia–specific stretch (PFSS) protocol that has provided significantly better patient outcomes. As reported by DiGiovanni et al23 in 2003, the PFSS exercise involves maintaining passive ankle and toe dosiflexion position with palpation and massage of the taunt bands of the plantar fascia on stretch (Fig. 13-10). Over a period of 8 weeks, PFSS was compared with Achilles stretching in 101 patients with plantar fasciitis of at least 10 months duration (Fig. 13-11).23 Both groups were also treated with 3 weeks of celecoxib and prefabricated soft inserts. Eighty-two patients in this prospective randomized comparison completed the study. Statistically significant improvements were found in pain, activity limitation, and patient satisfaction in the PFSS group when compared with the Achilles group.23 After 8 weeks of treatment, all patients were converted to the PFSS treatment. A 2-year follow-up study with data from 66 of these patients demonstrated 75% returned to full activity without restrictions. For most patients, maximal improvement was reached within 6 months of receiving treatment, with only 16 of 66 patients seeking additional intervention later. Similar improvements in pain were found in the patients who initially started with the PFSS versus those who started with the Achilles stretching protocol and then later switched to the PFSS after 8 weeks.24 The biomechanical impact of the PFSS was later supported by the Flanigan et al29 cadaveric study, which investigated the foot and ankle position resulting in the greatest amount of stretch placed on the plantar fascia. Fifteen different configurations were used, with combined ankle and toe dorsiflexion producing the maximum stretch. In addition, Cheng et al14 evaluated the finite element analysis of plantar fascia mechanics and demonstrated that toe dorsiflexion has a larger impact on plantar fascia strain than an Achilles tendon dorsiflexion force by a ratio of approximately 2 : 1. These studies assist in supporting the clinical results as well as the logic of treating patients with PFSS versus Achilles stretching alone.
Plantar Heel Pain
History

Epidemiology
Anatomy
Plantar Fascia
Heel Fat Pad
Etiology
Patient History and Physical Examination

Imaging and Other Diagnostic Studies
Nonoperative Treatment
Proximal Plantar Fasciitis
Stretching
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Plantar Heel Pain