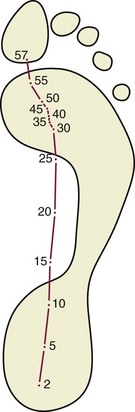
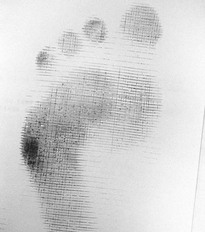
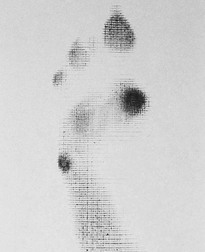
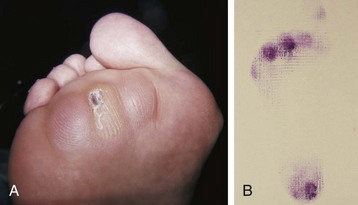
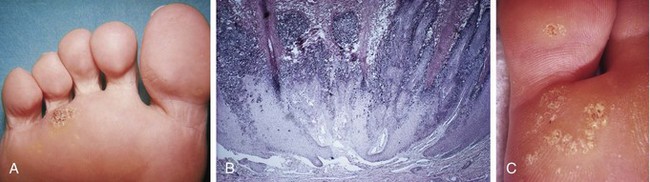
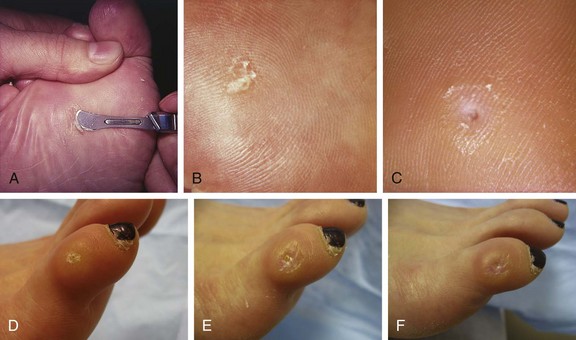
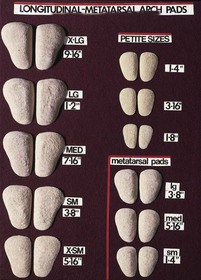
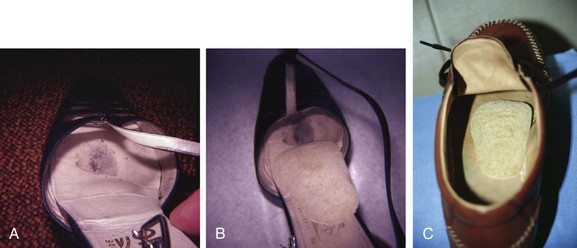
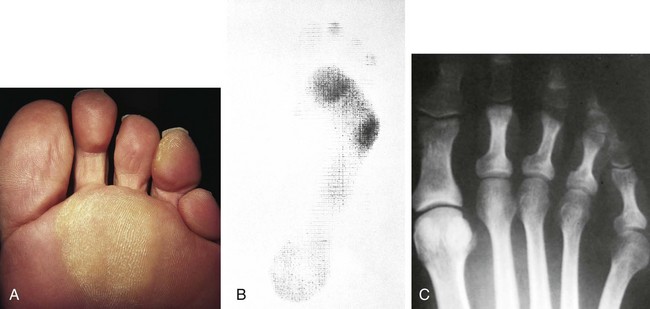
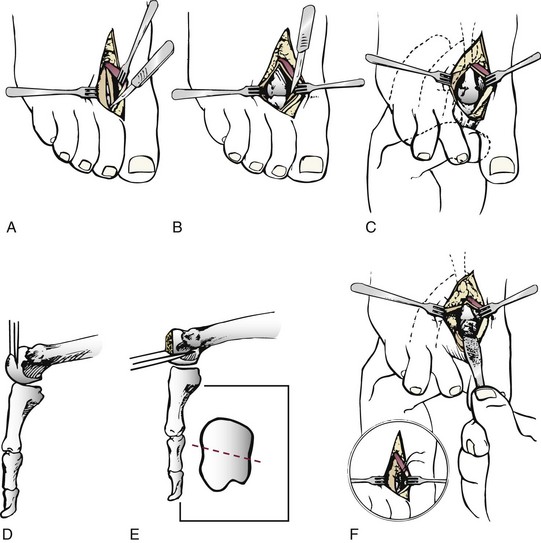
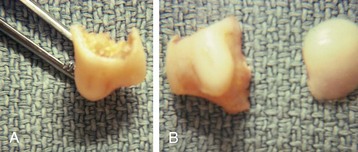
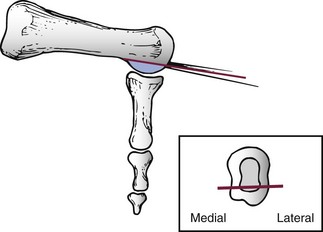
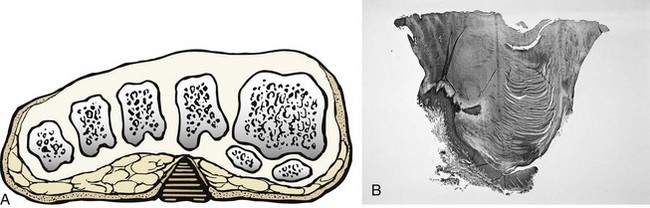
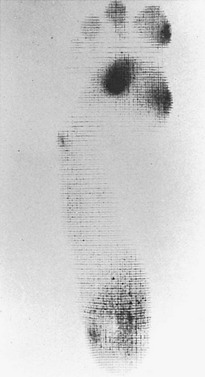
Chapter 8 Localized Intractable Plantar Keratosis Discrete Callus beneath Tibial Sesamoid Diffuse Intractable Plantar Keratosis Localization of pressure along the plantar aspect of the foot illustrates the relative length of time that the center of pressure dwells beneath the metatarsal heads during normal walking (see Chapter 1). After heel strike, the center of pressure moves very rapidly to the metatarsal head area, where it dwells for more than 50% of the stance phase, after which it moves toward the toes (Fig. 8-1). Because of this extended period of weight bearing in the metatarsal area, abnormal alignment of the forefoot, either localized or generalized, can result in the formation of a keratotic lesion. A broad differential diagnosis (Box 8-1) must be considered in the evaluation of the patient presenting with a plantar callus. The diagnosis is usually not difficult to make, but at times the diagnosis may not be clear, and one needs to consider these various causes. The predominant pattern of the metatarsal cascade demonstrates that the first metatarsal is shorter than the second approximately 60% of the time.24 The mobility of the first metatarsocuneiform (MTC) joint or the first metatarsophalangeal (MTP) joint determines the degree of weight bearing of the first ray. The plantar aponeurosis mechanism brings about plantar flexion of the first metatarsal during the last half of stance phase and may become less functional as a hallux valgus deformity develops. As a result, plantar flexion of the first ray might not occur, which can lead to increased pressure under the second metatarsal head57 and diffuse callus formation secondary to increased weight bearing. Hypermobility of the first MTC joint, which may be pathologic in no more than 5% of patients, can also lead to increased weight bearing by the first metatarsal. Pressure is then transferred to the lesser metatarsals, where a diffuse callus can develop beneath the second and possibly third metatarsal (Fig. 8-2). The base of the second and third metatarsals is quite stable because of the rigidity of their tarsometatarsal articulations; therefore, if the first metatarsal is hypermobile or elevated from any cause, callus formation can occur beneath these metatarsal heads. The fourth and fifth metatarsals are more mobile, and therefore calluses rarely develop beneath them unless there is an abnormal foot posture or an osseous deformity. The posture of the foot must always be considered in evaluating the patient with an intractable plantar keratosis (IPK). Abnormal callus formation can be due to an equinus deformity of the ankle joint, a cavus foot, pes planus, a varus forefoot deformity, a pes planovalgus deformity (Fig. 8-3), or abnormal alignment of the MTP joints. Unless the underlying deformity is addressed, the IPK will persist. A varus forefoot deformity, in which the lateral border of the foot is more plantar flexed than the medial border, often results in a diffuse callus beneath the fifth metatarsal head (Fig. 8-4). A valgus forefoot deformity, in which the first metatarsal is more plantar flexed in relation to the lesser metatarsals, often results in a diffuse callus beneath the first metatarsal head region (Fig. 8-5). This is often associated with a cavus foot deformity. Abnormal alignment of the metatarsophalangeal joints, secondary to either subluxation or dorsal dislocation, results in a plantarward force on the metatarsal head and development of a diffuse callus beneath the involved metatarsal head. An extreme example is a patient with advanced rheumatoid arthritis (Fig. 8-6). The physical examination begins with the patient standing. Careful observation should be made of the posture of the toes, characteristics of the MTP joints and longitudinal arch, and the position and posture of the hindfoot in relation to the forefoot. Strength testing of all muscle groups, a thorough neurovascular examination, and range of motion of the ankle, subtalar, transverse tarsal, and MTP joints should be noted. Hypermobility of the first ray, the presence of hallux rigidus,22 as well as swelling, thickening, synovitis, and instability of the lesser MTP joints57 are important diagnostic findings. It is important to differentiate a wart, or plantar verruca, from a callus. Plantar verrucae are common, affecting 7% to 10% of the population.10,37 A plantar verruca is usually localized but occasionally demonstrates a mosaic pattern and is usually not discretely located beneath a metatarsal head. Papillary lines, or rete ridges, diverge around the lesion, whereas in a callus, the rete run unchanged across the lesion.21 To facilitate identification, the lesion is often trimmed with a No. 17 blade. Trimming enables the clinician to identify the margins of the callus, because in a well-localized plantar keratosis, the callus itself has definite circumscribed edges, as opposed to a diffuse callus, which is a generalized thickening of the plantar skin without a defined margin. A wart, on the other hand, may have a small amount of hyperkeratotic skin overlying it, but very quickly one enters the warty material, which consists of multiple end arteries that bleed vigorously, as opposed to a true plantar keratosis, which has no blood supply (Fig. 8-7). Warts are commonly caused by the human papilloma virus (HPV),47 with the dark and moist environment within a shoe facilitating survival. Numerous treatments have been described for this often recalcitrant lesion, including chemical ablation, immunologic modifying treatments, and surgery. Common chemical ablation techniques include phenol, 10% fermaldehyde, 10% formaldehyde with monochloroacetic acid,30 fluorouracil, and bleomycin sulfate.53 Topical treatments include salicylic acid, fluorouracil,64 canthadrin and podophyllotoxin,6 formaldehyde, silver nitrate, corticosteroids, and garlic extract.7 Cryotherapy and electrocautery have been used with varying results. Surgical excision is often required, with recurrence not uncommon. Other rare dermatologic lesions that present as plantar callosities include keratosis palmoplantaris nummularis and epithelioma cuniculatum. If these lesions are suspected, dermatology consultation is recommended (Fig. 8-8). Keratosis palmoplantaris nummularis is an autosomal dominant skin disorder characterized by painful callus formation over areas of mechanical stress on the palms and plantar surface of the foot. It often presents upon the onset of walking in a child, with pain being the primary complaint. Physical examination reveals essentially normal motor and sensory function, with multiple areas of large hyperkeratotic callus formation over weight-bearing areas of the feet that are confluent with the surrounding skin.52 Histologic evaluation is consistent with epidermolytic hyperkeratosis.61 Operative treatment has been reported to be unsuccessful.61 The mainstay of treatment is shaving of the callosities, orthotics, and footwear modification. The natural history and successful treatment of the disorder remain elusive. Epithelioma cuniculatum is a form of verrucous carcinoma that affects the plantar surface of the feet.45 It is an uncommon low-grade squamous cell carcinoma that is typically slow growing and has a tendency to local recurrence. Although metastatic disease is rare, lack of timely diagnosis can lead to its spread.55 It can present as a painless, nonhealing ulceration on the plantar surface of the foot that slowly increases in size and is refractory to standard callus treatment.33 Diagnosis of this rare lesion can be challenging, and deep biopsy is required. The human papilloma virus has been implicated as a causative factor, but both HPV-positive and -negative lesions have been reported.37 Histologic analysis reveals a well-differentiated tumor composed of keratinocytes that extend the dermis and deeper structures, forming sinuses and keratin-filled cysts. Tumor cells in the granular layer may show vacuoles.55 There is often marked hyperkeratosis, with perakeratosis of a prominent granular layer occasionally seen.33 Treatment options include imiquimod (a topical immune-modulating drug), carbon dioxide (CO2) laser ablation, and surgical excision.33 The plantar callus can be trimmed with a sharp knife. A No. 17 podiatric blade is especially useful for trimming of hyperkeratotic skin. When trimming a callus, one should attempt to reduce the hyperkeratotic tissue, and if it is invaginated, this too should be trimmed. With a deep-seated lesion, however, it may not be possible to remove all of the keratotic lesion at the first trimming, and several trimmings may be necessary to permit the deep-seated portion of the callus to surface. Occasionally, a seed corn, which is a well-localized keratotic lesion, usually 2 to 3 mm in diameter, can be removed at the first sitting, although it might require a second trimming (Fig. 8-9). After debridement of the callus, a soft metatarsal support is used to relieve pressure on the involved area (Fig. 8-10). The soft support can be used, provided that the patient’s shoe is of adequate size. If the patient is wearing stylish women’s dress shoes, there may not be sufficient volume for the foot and the metatarsal support. The patient with a significant keratotic lesion should be encouraged to wear a broad, soft, preferably low-heeled shoe to provide more cushioning for the plantar aspect of the foot. The metatarsal support should be placed into the shoe just proximal to the area of the lesion (Fig. 8-11). It is important to instruct the patient that this support may initially feel uncomfortable and may take a period of breaking in of a week to 10 days. Other footwear modification, such as a wide or tall toe box or the addition of a rocker-bottom sole, can potentially provide relief. If an equinus contracture is a contributing cause, physical therapy to stretch the gastrocsoleus complex can increase the relative length of the Achilles tendon unit, thereby increasing ankle dorsiflexion.18 If the callus persists and is symptomatic, surgical intervention can be considered. Surgical management of a plantar keratosis is based on the characteristics of the callus. A discrete callus with a central keratotic core is observed beneath the fibular condyle of the metatarsal head and beneath the tibial sesamoid (Fig. 8-12). When the patient with a discrete, localized lesion walks over a Harris mat, the imprint created is well localized beneath the prominence that has brought about the callus (Fig. 8-13). Histologically, this lesion is a dense, keratinized lesion with a central core (Fig. 8-14). Figure 8-13 Harris mat print demonstrating well-localized area of pressure—a discrete plantar keratosis. Figure 8-14 A, Location of a discrete plantar keratosis beneath a prominent fibular condyle. B, Histologic features of the keratotic lesion demonstrate layers of keratin with no blood vessels. Compare with Figure 8-7B. This should be differentiated from a diffuse callus, which is often caused by deformity at the MTP joints because of instability, and usually associated with abnormal weight bearing during the third rocker portion of the gait cycle, in which only the forefoot is in contact with the ground (Fig. 8-15).15 A diffuse callus is observed beneath a metatarsal head that does not have a prominent fibular condyle and is noted most often beneath the second metatarsal head. Occasionally, a diffuse callus is noted beneath multiple metatarsal heads. When this type of callus is present and is trimmed, although the material consists of hyperkeratotic skin, there is no central core as observed in a discrete callus. When this patient walks over a Harris mat, the print that is observed is diffuse beneath the entire metatarsal head or beneath multiple metatarsal heads (Fig. 8-16). In general, a callus underneath several metatarsals is often due to forefoot overload, such as seen in ankle equinus; plantar flexion of the metatarsals, as in a cavus foot; or first-ray insufficiency. This indicates overload during the foot flat portion of the gait cycle during the second rocker portion of swing phase.15 This type of diffuse lesion is occasionally observed beneath the first metatarsal head if it is plantar flexed. It can be observed beneath the second metatarsal head when the first metatarsal is short, hypermobile, or due to first-ray instability brought about by an advanced hallux valgus deformity or possibly insufficiency after bunion surgery, if the joint has been destabilized. A diffuse callus beneath the second, third, and fourth metatarsal heads is usually observed in a patient with an extremely short first metatarsal, which results in increased weight bearing beneath the three middle metatarsals (Fig. 8-17). Occasionally, a diffuse callus is present beneath the fifth metatarsal head in patients with a varus configuration of the forefoot, or with a plantar-flexed fifth metatarsal associated with a tailor’s bunion. Figure 8-16 Harris mat print demonstrates diffuse keratotic lesion beneath second metatarsal head. Compare with Figure 8-15. (From Mann RA: Intractable plantar keratosis Instr Course Lect 33:293, 1984.) Differentiating the type of callus is essential because the nature of the callus determines the type of surgical procedure that will give the best result. In general, a localized callus will require an elevating procedure, whereas a diffuse callus requires a shortening procedure.15 A localized IPK, which is usually caused by the prominence of the fibular condyle, can be treated by a DuVries metatarsal condylectomy. DuVries12–14 initially described the procedure in which he carried out an arthroplasty of the MTP joint by removing a portion of the distal articular surface and the plantar condyle. Coughlin3 and Mann41 modified the procedure by removing only the plantar condyle. Both procedures seem to lead to satisfactory clinical results. 1. A hockey stick–shaped incision begins in the second web space and is carried across the metatarsal head proximally to about the distal third of the metatarsal shaft (Fig. 8-18A). 2. Passing medially and laterally to the extensor hood, the transverse metatarsal ligament is identified and released. 3. The interval between the long and short extensor tendons is opened and continued through the joint capsule to expose the MTP joint. 4. The collateral ligaments are transected, and the MTP joint is sharply plantar flexed while pressure is applied to the plantar aspect of the foot with the index finger of the same hand (Fig. 8-18B and C). 5. The distal 2 mm of articular cartilage is removed from the metatarsal head in a plane perpendicular to the metatarsal shaft. As this cut is made, the osteotome is angled slightly proximally; otherwise, it will skid off the cartilage and make an oblique cut (Fig. 8-18D). 6. The MTP joint is now sharply plantar flexed to bring into view the plantar condyle. The plantar 20% to 30% of the metatarsal head is removed with a 10- to 12-mm thin osteotome. The osteotome is angled slightly plantarward to avoid inadvertent splitting of the metatarsal shaft (Fig. 8-18E). 7. On completion of the osteotomy in the metatarsal head, the plantar condyle is delivered by use of a Freer elevator or thin rongeur in the adjacent interspace, and the condyle is removed. It is difficult to pull this fragment of bone out directly over the proximal phalanx, so it is pushed into the interspace and removed (Fig. 8-19). 8. The edges are carefully rongeured, and the joint is reduced (see Fig. 8-18F). The skin is closed in a routine manner. 9. A compression dressing is applied for 12 to 18 hours, and the patient is permitted to ambulate in a postoperative shoe. In a review of 100 patients surgically treated by Mann and DuVries,42 there was 93% patient satisfaction. It was observed that 42% of the lesions were beneath the second metatarsal head, 31% beneath the third, 19% beneath the fourth, and 8% beneath the fifth. A transfer lesion occurred in 13% of the patients, and the original lesion failed to resolve in 5%. The modification of the condylectomy by Coughlin is carried out in the same way as the DuVries metatarsal condylectomy, except that the distal portion of the metatarsal is not removed (Fig. 8-20 and
Keratotic Disorders of the Plantar Skin
Plantar Keratoses
Anatomy
Diagnosis
Treatment
Conservative Treatment
Surgical Treatment: Types of Plantar Callosities

Localized Intractable Plantar Keratosis
DuVries Metatarsal Condylectomy
Surgical Technique
Results
Coughlin Modified Metatarsal Condylectomy
![]() Video Clip 69).3,41 This makes removing the plantar condyle a little more difficult. Until now, there has been no published report regarding the results of this modification of the DuVries procedure, although preliminary data indicate about a 5% incidence of transfer lesions. The use of a power rasp with which to shave down the prominent fibular condyle46 has been described. This avoids the potential difficulty of retrieving the osteotomized plantar condyle from the interspace. Thermal necrosis and bone debris can be avoided by use of irrigation.
Video Clip 69).3,41 This makes removing the plantar condyle a little more difficult. Until now, there has been no published report regarding the results of this modification of the DuVries procedure, although preliminary data indicate about a 5% incidence of transfer lesions. The use of a power rasp with which to shave down the prominent fibular condyle46 has been described. This avoids the potential difficulty of retrieving the osteotomized plantar condyle from the interspace. Thermal necrosis and bone debris can be avoided by use of irrigation.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree