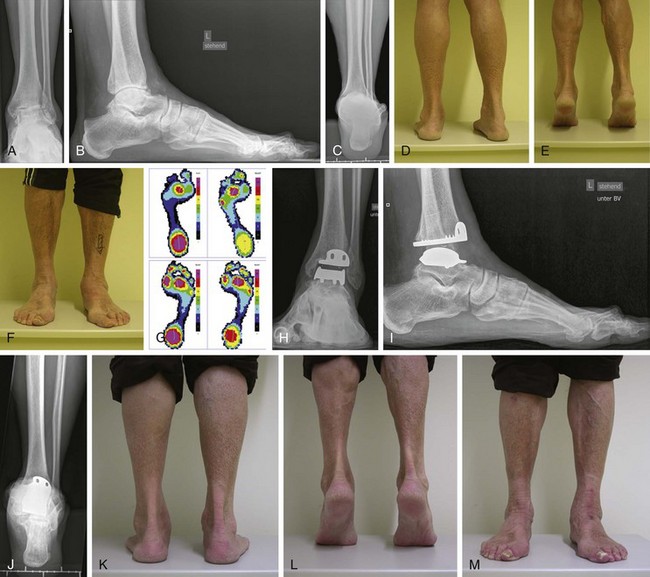
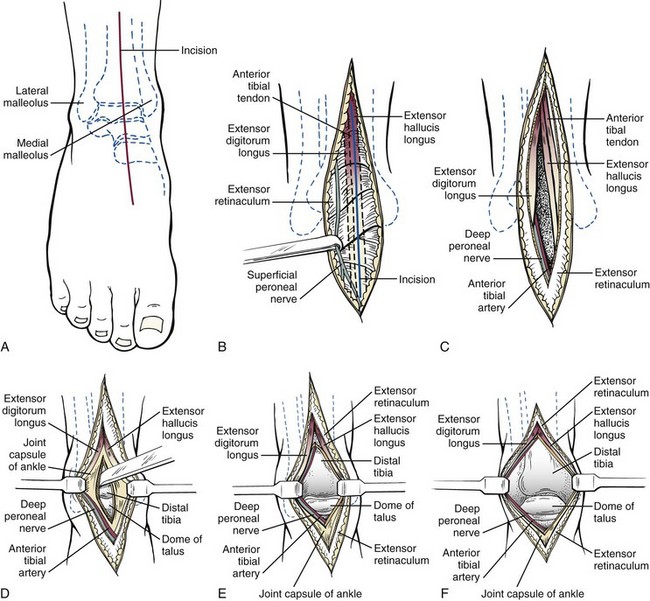
Chapter 22 SHORT HISTORY OF ANKLE REPLACEMENT First-Generation Total Ankle Designs St. Georg–Buchholz Ankle Prosthesis Imperial College of London Hospital Prosthesis Irvine Total Ankle Replacement Richard Smith Total Ankle Replacement Conaxial Beck-Steffee Ankle Prosthesis Bath-Wessex Total Ankle Replacement KINEMATICS AND BIOMECHANICS OF TOTAL ANKLE REPLACEMENT Surgical Technique by Anterior Approach Surgical Technique by Lateral Approach Total Ankle Replacement in the Valgus Osteoarthritis Ankle Morphologic Types of the Valgus Osteoarthritic Ankle Surgical Technique of Total Ankle Replacement in the Valgus Osteoarthritic Ankle Total Ankle Replacement in the Varus Osteoarthritis Ankle CLASSIFICATION OF TOTAL ANKLE REPLACEMENT Clinical Results after Total Ankle Replacement Buechel-Pappas Ankle Prosthesis Scandinavian Total Ankle Replacement (STAR) ( Salto Total Ankle Replacement ( HINTEGRA Total Ankle Replacement ( Ramses Total Ankle Replacement Alphahorm Total Ankle Replacement INBONE Total Ankle Replacement ( Trabecular Metal Total Ankle ( FAILED PREVIOUS REPLACEMENT SURGERY Early results with total ankle replacement (TAR) were highly disappointing. In the search for a workable ankle design, a number of different approaches were tried. Our current ability to critically analyze design strategies from the 1970s and 1980s is limited by the paucity of published data documenting the results of total ankle arthroplasties. Most clinical series from that period included 20 to 40 patients followed for an average of 5 years or less. The length of follow-up was a major factor affecting figures for patient satisfaction because satisfaction generally declined with longer follow-up.290 Rates of radiographic evidence for loosening with early implant designs were extremely high, ranging from 22% to 75%.* Since the 1990s, interest in TAR has resurged with improved designs, better fixation approaches, and a new generation of optimistic surgeons. Whether the optimism is warranted is not yet fully known; however, intermediate-term results with the newer approaches appear to justify the optimism. Both fixed and mobile bearings are now available, but which of the two is better remains a matter of debate.99,353 The fixed bearings can be highly cross-linked and are less likely to break or subluxate. The mobile bearings offer the opportunity for greater congruency and, theoretically, less wear. Head-to-head comparison of fixed- and mobile-bearing–generated wear particles show no major difference and similar overall characteristics as for total knee replacements at short term.2,3,31,197 In the United States, at the time of writing, the Agility implant (Depuy, Warsaw, Ind.), Scandinavian Total Ankle Replacement (STAR) (Small Bone Innovations, Morrisville, Pa.), Salto Talaris (Tornier, Amsterdam, The Netherlands), INBONE (Wright Medical, Arlington, Tenn.), and Zimmer TM Ankle (Zimmer, Warsaw, Ind.) are approved or cleared by the U.S. Foot and Drug Administration (FDA) for general use. All other implants used in the United States at this time must be prescribed on a case-by-case custom basis and fall under the scrutiny of the FDA, which regulates the use of these devices in the United States. Worldwide, many other implants are being used, most with mobile-bearing designs. The vast majority require an anterior approach for access to the joint. Modern prosthetic designs vary in area covered (some cover part of the medial or lateral recesses), contours of the articulating surfaces, materials, and fixation techniques. Limited early and intermediate results have been published for several of these implants with remarkably good results.* However, most of the clinical results with the newer implants are from inventors’ initial series; further independent studies are clearly needed to determine true efficacy. Initial reports, however, show lower rates of early complications than previously published. Several issues are likely to have affected this change, including improved surgical selection, refined indications, meticulous handling of soft tissues, less dissection for lower-profile implants, better instrumentation, and better postoperative care. In general, TAR is continuously becoming recommended as a treatment option in patients with end-stage ankle osteoarthritis. Ankle arthrodesis cannot be accepted as the sole gold standard procedure in this patient cohort. Saltzman et al294 reported initial findings from a prospective controlled trial of the STAR prosthesis versus ankle fusion and showed TAR led to better function and similar pain relief compared with ankles that were fused. Haddad et al128 performed a systematic review of the literature, including 852 ankle arthroplasties and 1262 ankle fusions. Meta-analytic mean results showed 38% of the patients treated with TAR had an excellent result, 30.5% had a good result, 5.5% had a fair result, and 24% had a poor result, with the corresponding values in the ankle arthrodesis group being 31%, 37%, 13%, and 13%, respectively. The revision rate after TAR and ankle fusion was 7% and 9%, respectively.128 In most articles detailing TAR history,* the study by Lord and Marotte223 is identified as the first clinical study to report outcomes in TAR patients. However, in 2002, Muir et al239 reported the clinical outcome in a 71-year-old male who underwent talar dome resurfacing with a custom Vitallium implant for posttraumatic osteoarthritis in 1962. The clinical examination at a 40-year follow-up showed mild hindfoot malalignment with good clinical results, including slightly decreased range of motion (35 degrees of plantar flexion), American Orthopaedic Foot and Ankle Society (AOFAS) score of 85, no pain, and no limitation of daily activities.239 In the aforementioned study by Lord and Morotte,223 an inverted hip stem was implanted into the tibia. The talus had been completely removed, and a cemented acetabular cup was then implanted in the calcaneus. This procedure was performed in 25 consecutive patients, with only 7 patients reporting satisfaction postoperatively.224 Twelve of the 25 arthroplasties failed; the authors did not recommend further use of this prosthesis design.224 At that time, the authors recognized the complexity of ankle biomechanics and concluded that a simple hinge prosthesis system with plantar flexion and dorsiflexion would not be able to mimic the normal ankle joint.224 The St. Georg–Buchholz ankle prosthesis is a semiconstrained prosthesis type introduced in 1973. However, the use of this prosthesis was abandoned after eight TARs because of the high failure rate.48,97 Hay and Smith135 implanted this prosthesis in 15 patients. At a mean follow-up of 10 years, 11 early and 32 late complications were reported.135 The Imperial College of London Hospital (ICLH) TAR was a two-component, constrained total ankle design with a polyethylene tibial component.105,179 For implantation, cemented fixation with polymethyl methacrylate bone cement was used. Freeman et al105 reported laboratory wear and fixation tests and their clinical experience of 2 years.105 Bolton-Maggs et al38 retrospectively reviewed midterm outcomes of 62 TARs performed between 1972 and 1981, using the ICLH ankle prosthesis Mark VII. This version of the prosthesis had a polyethylene tibial component that could be trimmed to an appropriate size at the time of operation.297 At the mean follow-up of 5.5 years, 41 ankles were clinically reviewed. Only 13 patients had satisfactory results. The authors reported high complication rates, including wound healing problems, talar collapse, and loosening of the prosthesis components. By midterm, 13 ankles had to be revised and converted to ankle fusion. Therefore the authors suggested ankle fusion as a superior treatment option, regardless of the underlying etiology of ankle osteoarthritis (OA).38 Samuelson et al297 published their results obtained in 75 patients who received an ICLH prosthesis. The majority of patients (70%) reported acceptable results. The most frequently reported complication was delayed wound healing. Despite acceptable results reported by many patients, complication rates were high; thus the authors stated that the use of this prosthesis should be approached with caution.297 Herberts et al143 performed 18 ICLH ankle arthroplasties in 16 patients and followed them for a mean of 36 months. In four cases, an aseptic loosening was observed; radiolucent zones greater than 2 mm were seen in another 7 ankles. Despite the acceptable results, the authors indicated that the failure rate may increase with longer follow-up.143 The Irvine ankle design (also known as the Howmedica prosthesis) was one of the first ankle prostheses in which a special talus anatomy was closely considered (Fig. 22-1).365 The prosthesis designers performed anatomic measurements of 32 tali to establish the morphology of talus.365 Evanski and Waugh102 performed 29 cemented TARs before December 1975, using 25 Irvine ankle prostheses and 4 Smith prostheses. In all patients, significant functional improvement, including increased range of motion and pain relief, was observed. However, the mean follow-up was only 9 months, and already in this short postoperative period, malalignment occurred in two patients, one of whom needed revision surgery. In two patients, a prosthesis failure was observed (Fig. 22-2). The analysis of failures showed that the unconstrained prosthesis design in combination with its surface geometry led to increased rotation between both components, resulting in an overload of surrounding soft tissue and ligaments. Despite these poor short-term results, the authors stated that TAR would be an acceptable alternative treatment to ankle fusion.102 However, no longer-term results in patients who underwent Irvine TAR are available in the current literature. Richard Smith TAR is a nonconstrained, so-called ball-and-socket (spherocentric) prosthesis that was introduced in 1975 (Fig. 22-3).184 This prosthesis design included a metal tibial component (“socket”) and polyethylene talar component (“ball”); both components were fixed with cement. Besides the aforementioned study by Evanski and Waugh,102 only a few studies have been published addressing the outcome in patients who underwent Richard Smith TAR. Kirkup184 performed 24 Richard Smith TARs in 21 patients (three cases were bilateral). Eighteen ankles were available for a mean follow-up of 7 years. Seven patients developed loosening of the tibial component, requiring revision arthroplasties using Bath-Wessex TAR in three cases at 4.1, 4.3, and 6.8 years, respectively. In one case with loosening, a deep infection occurred, resulting in ankle arthrodesis. The remaining three cases were under observation. In 7 patients, delayed wound healing was observed. Most patients in this cohort experienced substantial pain relief. Because of a high revision rate, the recommendation was not to use this prosthesis design.184 Dini and Bassett88 used the Richard Smith prosthesis in 21 patients. At a mean follow-up of 27 months, failure occurred in five ankles; in other patients, significant pain relief and improved function of the ankle were observed.88 The Conaxial Beck-Steffee TAR is a highly constrained prosthesis type.230 Wynn and Wilde378 presented clinical results in 30 patients treated with Conaxial Beck-Steffee prosthesis between 1975 and 1977. All patients were reviewed at a mean follow-up of 10.8 years. Early postoperative complications were common and included wound healing problems (39%), deep infection (6%), malleoli fractures (22%), and painful talofibular impingement (14%). At 2-year follow-up, 27% of all prosthesis components already showed significant loosening. This negative tendency was confirmed at later follow-ups, resulting in a 90% loosening rate at 10 years. Therefore the authors did not recommend the further use of this prosthesis.378 In the 1970s, St. Elmo Newton252 reported that fused ankles may produce additional stress on the knee and midtarsus joints, thus accelerating the advancement of preexisting degenerative changes.250,251 Therefore he performed 50 TARs since 1973, using a nonconstrained cemented prosthesis, including the high-density polyethylene tibial and Vitallium talar components (Fig. 22-4). In 75% of ankles, aseptic loosening was observed.251 Eighteen failures occurred at a minimum follow-up of 1 year. This finding may explain related increased polyethylene wear caused by incongruency of TAR components: the tibial component was a portion of a cylinder, and the talar component was a portion of a sphere with a slightly smaller radius. Regarding the high failure rate, the following contraindications for TAR were identified: any recent infections, valgus or varus deformity of the talus of 20 degrees or greater, significant ligamentous instability of the ankle, avascular necrosis of the talus, nonunion of prior ankle fusion, and rheumatoid arthritis in patients having long-term steroid therapy.250,251 The Bath-Wessex TAR is an unconstrained, two-component total ankle design. Carlsson et al56 reported a 10-year survivorship analysis of 69 Bath-Wessex prostheses implanted between 1984 and 1996.56 The initial acceptable results published in another earlier study (5-year survivorship of 81%)55 were not maintained in this study (10-year survivorship of 66%).56 Eighteen ankles had to be revised (12 ankle fusions and 6 revision arthroplasties). In the remaining ankles, at least one component showed radiologic loosening signs (67% of all tibial and 82% of all talar components). Therefore the authors strongly discouraged use of this prosthesis type as a standard prosthesis.56 The Mayo TAR was designed as a constrained design by Stauffer in the 1970s. It was a highly congruent two-component design, including a polyethylene tibial component with cement fixation.320,321 Stauffer and Segal320 performed 102 TARs using the Mayo Total Ankle between 1974 and 1977. At a mean follow-up of 23 months, 53 complications were observed in 54% of ankles with posttraumatic OA and in 23% of those with rheumatoid OA. Loosening of prosthesis components in 7 ankles resulted in five revision arthroplasties and two fusions.321 Kitaoka et al187 reported on 204 primary Mayo TARs between 1974 and 1988 at the Mayo Clinic. The mean follow-up in this patient cohort was 9 years, with a range of 2 to 17 years. The overall 5-, 10-, and 15-year survivorship was 79%, 65%, and 61%, respectively. Because of the high failure rate, the use of this prosthesis was not recommended, especially in younger patients.186,187 Demottaz et al80 published a clinical gait analysis study, including 21 TARs performed between 1974 and 1977. Different prosthesis types were used in the study: 14 patients received a single-axis prosthesis (Mayo, Thompson-Parkridge-Richard [TPR], Buchholz, or Oregon) and 7 patients received a multiple-axis prosthesis (Waugh or Smith). At the mean follow-up of 15 months, pain relief and functional improvement results were disappointing. Also, the rate of progressively increasing loosening was alarmingly high at 88%. Therefore the authors suggested ankle fusion as the treatment of choice for ankle OA.80 Lachiewicz et al212 reviewed 17 TARs (14 Mayo ankle prostheses and 1 Buchholz ankle prosthesis) performed between 1976 and 1981.212 The indication for the surgery in all patients was rheumatoid OA. At a mean follow-up of 39 months, all patients experienced pain relief and improved range of motion (ROM). No patients required revision surgeries; however, radiolucencies at the bone–cement interface and the subsidence of six components were observed in 11 ankles.212 The same patient group was included in a long-term study by Unger et al.340 Overall, 21 patients who were treated with TAR were enrolled for retrospective review at a mean follow-up of 5.6 years, with a range of 2 to 10 years. Eight from a final group of 17 available patients reported their results to be fair or poor. In 14 of 15 cases, subsidence and loosening were observed. Twelve tibial components had tilting; however, the postoperative position of the implant showed no significant correlation with radiolucency around the component.340 The Oregon ankle is a single-axis, two-component TAR design. Groth and Fitch126 performed 71 primary cemented TARs using Oregon ankle prosthesis between 1975 and 1985. At a mean follow-up of 6.5 years, reoperations were necessary in 19 patients, including 11 ankle fusions and 5 revision arthroplasties. The authors concluded that TAR should be limited to patients with rheumatoid arthritis and to elderly less-active patients with posttraumatic OA.126 In 1986, McGuire et al231 performed a retrospective comparative study addressing outcome and complication rates in patients who underwent TAR versus ankle arthrodesis. The TAR group consisted of 25 patients with six different prosthesis types (Oregon, TPR, Richard Smith, Newton, Mayo, and Buchholz). The mean follow-up was 3.8 years. Four patients with TAR had infections (vs. 5 of 18 in the arthrodesis group). Loosening occurred in 5 patients with TAR (vs. 6 nonunions in arthrodesis group). The authors concluded that TAR should not be performed in younger patients with posttraumatic OA.231 The Thompson-Richard prosthesis (TRP) was introduced in 1976 as a two-component semiconstrained cemented implant. The prosthesis design included the polyethylene tibial component with a concave articular surface and a lip on each side designed to avoid too-excessive transversal movement of the talar component.28,377 Wood et al377 compared the clinical and radiologic outcome of the cemented TRP prosthesis (seven ankles replaced during 1991 and 1992) and cementless STAR prosthesis (also seven ankles). The mean follow-up for TRP and STAR groups was 7.2 and 5.4 years, respectively. In the TRP prosthesis group, four tibial components showed significant loosening, requiring ankle fusion in two cases, while all components of the STAR prosthesis remained stable at the latest follow-up.377 A similar comparative study—TRP versus STAR prosthesis—was performed by Schill et al,302 including 27 TRP and 22 STAR implants. At a follow-up ranging from 1 to 12 years, 37 patients with 20 TRP and 19 STAR prostheses were reviewed. In patients with TRP prostheses, a high rate of radiolucency around the tibial component (53.3%) was seen; also, in three ankles talar components were found to have significant subsidence. In patients with STAR implants, only three cases showed small radiolucent lines of the flat tibial component, while the talar components showed no signs of loosening or migration. In the TRP group, two revisions were performed, because of prosthesis loosening and malleolar fracture, resulting in a 12-year cumulative survivorship of 87%. In the STAR group, two revisions were necessary because of one meniscal-bearing breakage and correction of meniscal-bearing height, resulting in a 6-year cumulative survivorship of 94.3%.302 Jensen and Kroner174 observed a high rate of radiolucency around prosthesis components in 52% of 30 reviewed ankles. Revision was necessary in only two cases; however, only 69% of all patients were satisfied with the results obtained at a follow-up of 5 years.174 The New Jersey Cylindrical Replacement design was developed in the 1970s by Michael Pappas, a bioengineer, and Frederick Buechel, an orthopaedic surgeon.261 During the development of the design rationale, the authors recognized essential problems regarding ankle anatomy (normal ligamental function, physiologic ROM, intrinsic stability during ROM), surgical technique (component biocompatibility, minimal resection of bone, preservation of blood supply to the talus and distal tibia, postoperative rehabilitation), and mechanical objectives (optimal force transfer at bone–prosthesis interface, minimal wear, anteroposterior [AP] shear load resistance). The treatment options in case of ankle failure (ability to remove prosthesis with minimal tissue damage, revision arthroplasty vs. ankle fusion) were also thoroughly discussed.261 Although the clinical results with the first generation of the New Jersey Cylindrical Replacement design were not satisfactory, the authors identified numerous problems regarding the design of TARs that were addressed later by other surgeons and designers.360 Most first-generation TAR designs used in 1970s and early 1980s were two-component prostheses, including both prosthesis types (constrained and unconstrained)121,147,156 and typically included a concave polyethylene tibial component and a convex metal component for the talus, usually made of a cobalt chrome alloy. Cement fixation was used to secure the talar and tibial components. The reason for the cemented fixation was simple: in the 1970s, cementless fixation and ingrowth surfaces were rare, and cement fixation led to acceptable stability in patients who underwent total knee or hip replacement. However, first-generation TARs were recognized to have unacceptably high complication rates, including aseptic loosening on both tibial and talar sites, wide osteolysis with cyst development, subsidence, and mechanical failure of prosthesis components. Cement fixation usually required substantial bone resection to accommodate the volume of cement at the initial implantation of ankle prosthesis. Larger bone resection resulted in fixation to bone with reduced mechanical quality, especially on the tibial side.170 This may explain some of reasons for the high failure rate. One conspicuous design feature of most first-generation ankle arthroplasty designs was a tibial component that was significantly larger than the talar component. The rationale was to achieve a physiologic range of motion of the replaced ankle as well as axial rotation. However, because of low intrinsic stability, significant shear forces occurred during the gait, which may have resulted in premature prosthesis wear and loosening, especially in patients with preexisting chronic ligamentous instability. Interpretation of all the factors that lead to TAR failure will remain challenging because of limited data. Most clinical reports addressing outcomes in patients who underwent first-generation TAR were case reports or small case series.290 Another critical factor limiting validity of studies were the short follow-ups of mostly 5 years or less. Patient satisfaction with this procedure was reciprocally proportional to the length of follow-up, varying between 19% and 81% of patient cohorts.290 In general, the clinical results of first-generation total ankle arthroplasties were highly discouraging. The alarming failure rate, along with other significant complications, including wound healing problems, inferior postoperative functional results, and so forth, led to the recommendation to use ankle fusion as the primary treatment option for ankle osteoarthritis.* In 1985, Hamblen130 stated the following in an editorial in the British edition of Journal of Bone and Joint Surgery: “Clearly the answer to the question of replacing the ankle joint using current techniques must be ‘no’.” Failure analysis of first-generation total ankle arthroplasties showed that only significant improvements in prosthetic design, change of fixation (elimination of cemented fixation), and improved anatomic access would change the arthroplasty outcome, making this procedure a valuable treatment option in patients with end-stage ankle osteoarthritis.290 Patients with ankle osteoarthritis usually show significant alteration of plantar pressure distribution.163,254 Horisberger et al163 measured plantar pressure distribution parameters in 120 patients with end-stage ankle osteoarthritis by using dynamic pedobarography. In most patients, a significant decrease of maximum force and contact area was observed. These findings might be interpreted as an attempt by patients to reduce the weight-bearing load on the arthritic ankle and to avoid pain.163 Patients with asymmetric ankle osteoarthritis have been found to have reduced peak ground reaction forces and peak kinetic values.254 Valderrabano et al assessed kinematic changes after ankle fusion and TAR with regard to ROM,344 movement transfer,345 and talar movement.346 All measurements were performed in native ankles, then in ankles with two-component (Agility) and three-component prostheses (HINTEGRA [Integra Life Sciences, Plainsboro, N.J.] and STAR), and finally in fused ankles. The results of the study showed near-normal kinematics after prosthesis implantation and significantly impaired measurements in fused ankles.344–346 Komistek et al206 used fluoroscopy to evaluate translational and rotational motions of the hindfoot in the sagittal and frontal planes in 10 subjects having a normal ankle and TAR on the opposite side (Buechel-Pappas prosthesis). The average ROM for normal versus replaced ankles was 37.4 degrees and 32.3 degrees, respectively. Furthermore, comparable kinematic patterns of motion were observed for normal and replaced ankles.206 Yamaguchi et al380 investigated in vivo kinematics of total ankle arthroplasty during non–weight-bearing and weight-bearing dorsiflexion and plantar flexion381 and during the gait. In their first study, the authors measured three-dimensional (3D) kinematics and addressed the articular surface incongruency during non–weight-bearing and weight-bearing activities in 47 patients who underwent TAR using the TNK prosthesis.381 No significant differences between non–weight-bearing and weight-bearing kinematics were detected. The observed kinematic patterns, including internal rotation during plantar flexion were similar to those observed in natural ankles. In more than 75% of all replaced ankles, incongruency of the joint surface was seen.381 In the sequel study of the same working group, in vivo kinematics and congruency of the articular surface during the stance phase of gait were investigated in 18 ankles of 15 patients.380 Three-dimensional–two-dimensional (3D–2D) mode image registration was performed in this study by using lateral fluoroscopic images and implant models. The mean ranges of motion for dorsiflexion/plantar flexion, inversion/eversion, and internal/external rotation were 11.1 ± 4.6 degrees, 0.8 ± 0.4 degrees, and 2.6 ± 1.5 degrees, respectively. In 8 of 18 ankles, at least one type of surface incongruency was observed during the stance phase, including anterior hinging in one ankle, medial or lateral lift-off, or excessive axial rotation. The surface incongruency, which was actually not observed in the static radiographs, has clear potential to lead to increased contact pressure, wear, and implant loosening.380 Detrembleur and Leemrijse85 addressed the effects of TAR on gait disability by analysis of energetic and mechanical variables. The study included patients who underwent TAR using three-component implant designs: Ankle Evolutive System (AES) prosthesis (Biomet, Nimes, France) (n = 16), Mobility prosthesis (Depuy, Warsaw, Ind.) (n = 3), and HINTEGRA prosthesis (n = 1). All patients were analyzed before and approximately 7 months after surgery by using instrumented motion analysis to assess spatiotemporal parameters, ankle kinematics, mechanical work, and electromyographic activity. In addition, energy expenditure was analyzed using an ergospirometer. The authors showed that TAR has a beneficial effect on locomotor function, resulting in improvement of speed, spatiotemporal parameters, ankle amplitude instance, and vertical center-of-mass displacement.85 In a relatively large study, Brodsky et al44 performed 3D gain analysis in 50 consecutive patients who underwent TAR using a STAR prosthesis, at a mean follow-up of 49 months, with a range of 24 to 108 months. The following kinematic and spaciotemporal parameters have been measured in this prospective study: stride length; cadence; sagittal plane range of motion of the ankle, knee, and hip; plantar flexion/dorsiflexion moment; and sagittal plane ankle power. A statistically significant improvement of range of motion from 14.2 to 17.9 degrees was observed; increased motion was also measured at the hip and knee. Furthermore, ankle power and ankle plantar-flexion moment were significantly increased. In this patient cohort, a more normal ankle function and gait were objectively observed after TAR.44 Hahn et al129 compared gait parameters in patients who underwent TAR and compared the results with those measured in patients with ankle arthrodesis. In addition, pain and physical function were assessed in 9 patients with TAR and ankle arthrodesis preoperative and 12 months after the surgery. Both surgical procedures provided significant pain relief and functional improvement in gait. However, patients with TAR had more natural ankle joint function with increased range of motion.129 Valderrabano et al350 addressed patients’ rehabilitation in the first year after TAR in a prospective study, including 15 patients with unilateral posttraumatic ankle osteoarthritis. For comparison, patients were matched to 15 healthy persons without degenerative changes, with the appropriate demographic factors as a control group. Clinical and functional status and 3D kinematic-kinetic analysis was performed preoperatively and postoperatively at 3, 6, 9, and 12 months after TAR when using a HINTEGRA prosthesis. As expected, patients with ankle osteoarthritis showed significant clinical and functional impairments preoperatively as measured using the AOFAS and Short Form-36 (SF-36) scores. Preoperatively, gait analysis revealed a significant deficiency in six of seven measured spatiotemporal variables: a decrease of the triplanar ankle movement, a decrease of the second active maximal vertical and the maximal medial ground reaction force, a reduction of the sagittal and transverse ankle joint moments, and a reduction of the ankle joint power. Three months postoperatively, patients with a replaced ankle experienced worsening of gait. However, by 12 months no differences in the spatiotemporal variables were detected with respect to normal subjects.350 In another study, Valderrabano et al349 addressed the muscle rehabilitation in the same patient cohort. It has been shown that TAR normalizes the muscle function (including torque and electromyographic “intensity”) in OA ankles to a significant extent. However, after 1 year of rehabilitation, patients did not reach the level of the contralateral, unaffected leg.349 Pedobarography may be also used for measurement of plantar pressure distribution in patients after TAR.107,156,240,284 Hintermann and Valderrabano156 reported their preliminary results of 148 consecutive total ankle arthroplasties when using a HINTEGRA prosthesis. The normal plantar pressure distribution and a normal line of center of pressure were observed in 78.1% of all cases. An increased forefoot pressure, a discharge of the forefoot pressure, and an increased lateral pressure were found in 10.4%, 7.3%, and 4.2%, respectively, of all replaced ankles.156 Valderrabano et al342 analyzed results of dynamic pedobarography obtained in 65 consecutive patients with a STAR prosthesis. A normal plantar pressure distribution while walking was found in 53% of all patients. Twenty patients had an increased forefoot loading, and 6 patients had an increased lateral foot loading.342 Frigg et al107 assessed the hindfoot alignment in 28 consecutive patients with TAR by using visual means, radiographs (hindfoot alignment view293), and dynamically with pedobarography. The following pedobarographic parameters were measured: coronal index, initial heel contact on heel strike, heel index, lateral medial area index, center-of-pressure index, lateral-medial force-time integral index, and gait line integral.107 In the opinion of the current authors, pedobarography may be helpful for detailed analysis of hindfoot analysis in patients with end-stage ankle osteoarthritis and concomitant varus (Fig. 22-5) or valgus (Fig. 22-6) deformities. End-stage ankle arthritis is the main indication for this procedure. Unlike the hip and knee, the ankle joint is rarely affected by primary osteoarthritis. In clinical and epidemiologic studies, previous trauma has been shown to be the most common cause of ankle osteoarthritis.295,348 Rotational ankle fractures with consecutive cartilage damage was identified as the most common reason for posttraumatic ankle osteoarthritis.348 However, repetitive ligament injuries can also result in posttraumatic ankle osteoarthritis.343 Other common indications for TAR are systemic (rheumatoid) arthritis279,280,372 and secondary osteoarthritis. Secondary OA has been found to be associated with underlying diseases and/or pathologies, such as hemophilia,22,225,283,357 hereditary hemochromatosis,23,77 gout,29,207 postinfectious arthritis,40,271 and avascular talar necrosis.39,49,103,200 Patients with bilateral ankle osteoarthritis are good candidates for this procedure because bilateral ankle fusion generally has a detrimental influence on gait and functional outcome.113,243,253,288 This can be particularly important in patients with secondary osteoarthritis resulting from hemochromatosis or hemophilia,22,23 and bilateral TAR can be performed in two separate stages.34,104,114,207,358 However, in patients with bilateral end-stage ankle osteoarthritis, simultaneous bilateral TAR has been reported,25,28,178 resulting in significant pain relief and functional improvement comparable to the results achieved with a unilateral procedure.25,28 Patients considered for simultaneous bilateral TAR should be informed about a prolonged initial recovery period.28 In patients with previously performed subtalar, triple, and/or midfoot fusion, the tibiotalar fusion would completely “stiffen” the hindfoot, while the TAR may preserve the functional motion as mentioned before. The clinical outcome of TAR when combined with hindfoot fusion is comparable to that of ankle replacement alone.183 With increased use, an emerging indication for TAR is salvage of failed primary TAR.* A major concern in revision arthroplasty of the ankle can be anchorage of prosthesis components in deficient bone stock to ensure long-term prosthesis stability.153,160 After removal of the prosthesis component and careful debridement, if the residual bone stock is not sufficient, ankle fusion may be a better option.† Another special indication for total ankle arthroplasty is the salvage of painful nonunion or malunion of prior ankle fusion.14,122,154,155 Conversion of fused ankle to TAR is a technically demanding procedure that should be performed only if remaining bone stock is sufficient and soft tissue conditions are not too compromised (especially in patients with previous long-standing ankle arthrodesis).155 The conversion ankle arthroplasty should be limited only to experienced surgeons with adequate experience in primary TAR. If performed by experienced surgeons, this procedure has shown promising early results with low intraoperative and postoperative complication rates comparable to those observed in patients with primary TAR.122,154 The absolute contraindications127,151,156,290 for this procedure include acute or chronic infections. In several studies, avascular necrosis of the talus has been identified as an absolute contraindication for TAR.‡ In patients with avascular necrosis of more than one third of the talus, the use of a standard prosthesis component may lead to significant subsidence and loosening of the talar component and failure.* In these patients, a revision talar component160 or a custom-made talar prosthesis132,214,330 should be used. Patients with neuromuscular disorders, neuroarthropathy (e.g., Charcot arthropathy of the midfoot and/or hindfoot), massive joint laxity (e.g., patients with Marfan disease), or diabetes with clinically significant distal polyneuropathy should be excluded. Patients with severe instability and/or lower-leg malalignment that cannot be surgically corrected (e.g., by corrective osteotomies194,195,259) should not be considered for TAR. At present, there is no concensus for a clinically relevant cut-off for the degree of coronal deformity that can be corrected at the implantation of TAR. In general, a moderate preoperative coronal deformity of less than 10 degrees can be corrected intraoperatively by modification of bone cuts (especially on the talar side). In patients with a coronal deformity of more than 10 degrees, the deformity should be corrected before the implantation of the prosthesis component (as a one- or two-stage procedure). Suspected or documented metal allergy or intolerance is rarely observed; however, these patients should be excluded preoperatively. Although many authors suggest that previous ankle infection is an absolute contraindication for TAR,* the current authors cannot fully embrace this opinion. In a series of 17 consecutive patients with this history, who underwent HINTEGRA total ankle arthroplasty, Dr. Hintermann achieved good functional results and did not observe any recurrence of infection (unpublished data). Eichinger et al93 and Espinosa and Klammer98 also recommend TAR in patients with ankle OA resulting from previous infection. The relative contraindications127,151,156,290 for this procedure include significantly reduced bone quality (e.g., resulting from severe osteoporosis, immunosuppressive therapy, or long-term therapy with steroids) and diabetes without clinically significant polyneuropathy. Smoking is another relative contraindication because it is associated with higher risk of perioperative complications, including wound breakdown.368 Patients with high (e.g., contact sports, jumping) or increased (e.g., jogging, tennis, downhill skiing) demands for physical activities should be informed about possible mechanical failure caused by edge loading with increased wear and a potentially higher rate of aseptic loosening.246,351 Significant preoperative varus or valgus deformity (more than 10 degrees) has also been seen as a contraindication for TAR. With three-part ankle replacements, Doets et al89 found that preoperative deformity in the frontal plane is difficult to correct, causing instability and subluxation of the mobile bearing, which may result in the prosthesis failure.89 In their study of 200 STAR implants, Wood and Deakin373 observed that preoperative varus or valgus deformity of more than 15 degrees may cause edge loading of the mobile bearing. Therefore the authors stated that this may be a relative contraindication for TAR.372,373 However, the preoperative hindfoot deformity should not be an absolute contraindication, as long as additional realignment procedures (supramalleolar and/or calcaneal osteotomies, ligament reconstruction, subtalar fusion) can correct the deformity.47,82,183,195 Karantana et al177 did not observe any differences in functional outcome and prosthesis component survivorship between the patients with and without preoperative deformities, as long the deformity is addressed at the time of prosthesis implantation. Daniels et al76 demonstrated that correction of moderate-to-severe varus deformities is possible and results in good functional outcome and stability of prosthesis components. Kim et al183 reported that the clinical outcome of TAR performed in ankles with preoperative varus deformity of more than 10 degrees is comparable to that of neutrally aligned ankles. However, simultaneous surgical procedures addressing the preoperative deformity are necessary to achieve good results.183 Finally, and perhaps most importantly, the patient and the surgeon must have realistic expectations of this surgery.34,96,213 The high satisfaction of rheumatoid osteoarthritis patients after total ankle arthroplasty likely reflects the low demands and low expectations of this patient cohort.298 On the other hand, the expectations of patients with posttraumatic ankle osteoarthritis are generally higher than those of patients with non-posttraumatic ankle osteoarthritis.246 In particular, predictions regarding postoperative improvement in range of motion should be made carefully; as with current implants (all with an anterior approach), postoperative improvement in ankle range of motion is relatively small (generally <10 degrees) and therefore is not one of the expected benefits from this procedure.20,120 Based on the authors’ clinical experience27,290 and results published in the current literature, these are criteria for the “ideal candidate” with end-stage ankle osteoarthritis when assessing for TAR: All previous medical reports (e.g., surgery reports) and imaging data are collected and carefully analyzed. Especially in patients with posttraumatic ankle osteoarthritis and previously performed surgeries (e.g., open reduction and internal fixation), the exact type of hardware should be identified to ensure the hardware can be removed without any difficulty before implantation of prosthetic components. Actual the patients’ history is carefully assessed to specifically address the following aspects: actual pain (e.g., using a visual analog scale ranging from 0 = no pain to 10 = maximal pain),169 limitations in daily activities and quality of life (e.g., using the SF-36 questionnaire),363 sports activities (e.g., using the following scoring: 0 = none, 1 = moderate, 2 = normal, 3 = high, 4 = elite),351 and current and previous treatment. Patients with any of the aforementioned absolute contraindications are excluded. Especially in patients with significant comorbidities, a consultation in neurology and/or internal medicine should be arranged before planning TAR. The routine physical examination starts with careful inspection of the foot and ankle while sitting, standing, and walking, allowing dynamic comparison of changes at weight bearing versus non–weight bearing. The eventually observed pathologic findings should be compared with the contralateral nonaffected limb. Skin and soft tissue are carefully evaluated, with special attention given to previous surgical scars. Hindfoot stability is assessed manually, with the patient sitting (e.g., using the anterior drawer test).15,69,70 Ankle alignment, including supramalleolar deformities and the position of heel in relation to the longitudinal axis of the lower leg, is assessed with the patient standing. However, clinical assessment of the ankle and hindfoot alignment should be interpreted carefully because visual alignment assessment is often not accurate enough.107 Range of motion of the tibiotalar joint is determined using a goniometer placed along the lateral border of the leg and foot. All goniometric measurement should be performed in the weight-bearing position according to the method described by Lindsjö et al.222 Intrarater and interrater reliability of the goniometric measurements is usually not very high.382 However, the accuracy of the goniometric measurements of the tibiotalar joint range of motion was assessed by direct comparison with ankle range-of-motion measurements obtained from radiographs.20,66,154,157 Another alternative for assessing ankle dorsiflexion and stiffness is the Iowa Ankle Range of Motion (IAROM) device, which provided valid and reliable measurements (Fig. 22-7).369 Because many patients with end-stage osteoarthritis present with lower leg muscular atrophy,349 basic muscle function should be assessed (e.g., the function of tibial and peroneal muscles). Radiographic examination of affected ankles includes weight-bearing radiographs with anteroposterior and lateral views of the foot and an anteroposterior view of the ankle. All radiographs should be performed in the weight-bearing manner for appropriate evaluation of foot and ankle alignment, statics, and biomechanics because non–weight-bearing radiographs are often misleading (Fig. 22-8).95,167,237 Furthermore, the standing position of patients at radiographic examination may standardize the radiographic technique, resulting in a more reliable comparison between preoperative and postoperative radiographs. All possible coexisting degenerative changes in the adjacent joints as well as any deformities (e.g., flattening of the longitudinal arch of the foot) should be identified and carefully analyzed. Concomitant deformities in the osteoarthritic ankles may occur on the supramalleolar, intraarticular, and/or inframalleolar level. Supramalleolar ankle alignment is measured in coronal and sagittal planes by measurement of the medial distal tibial angle and the anterior distal tibial angle, respectively.192,227,323 The medial distal tibial angle has been measured to be 92.4 ± 3.1 degrees (range, 88-100 degrees) in a radiographic study192 and 93.3 ± 3.2 degrees (range, 88-100 degrees) in a cadaver study.172,192 The measurement of the medial distal tibial angle depends on radiograph technique.24,323 The anterior distal tibial angle has been measured to be 83.0 ± 3.6 degrees (range, 76-97 degrees).227 The inframalleolar ankle alignment (especially the heel position in relation to the longitudinal axis of the lower leg) is measured using the hindfoot alignment view.293 The hindfoot alignment view is taken at a 20-degree angle to the floor, with the foot placed with its medial border parallel to the radiographic beam.293 As already mentioned, the visual assessment of the hindfoot alignment is not accurate; therefore the hindfoot alignment view should be performed routinely for appropriate measurement of inframalleolar hindfoot deformities.106,107 A computed tomography (CT) scan may be helpful to assess the bony defects and to analyze the joint incongruency. In patients with degenerative changes of the adjacent joint, single photon emission computed tomography (SPECT-CT) may help to evaluate the morphologic changes and their biologic activities.193,258 Preoperative magnetic resonance imaging (MRI) may help to assess the concomitant ligamental injuries,136,149 pathologic changes of tendons,60,149 and avascular necrosis of osseous structures.136,149 One of the most widely measured parameters for gait analysis is assessment of plantar pressure distribution. In patients with ankle osteoarthritis, the following variables usually are specifically assessed: maximum force, contact time, peak pressure, contact area, and center of pressure index.163,176 The patients are asked to walk at their own preferred speed because prescribed speed may influence and change the normal gait pattern.242 For sufficient reliability of the pressure measurement, at least five dynamic trials of each foot should be recorded.165 For reliable and easier analysis, the pressure distribution measurements are commonly divided into four regions, including hindfoot, midfoot, forefoot, and toes.163 Reliable and accurate assessment of preoperative and postoperative patients’ functional outcomes is crucial in monitoring the effectiveness of TAR. Naal et al247 performed a systematic literature review including 79 original studies. Authors identified a total of 15 outcome instruments. The most commonly used ones were the AOFAS hindfoot score (n = 41),185 the Kofoed ankle score (n = 15),198 the visual analog scale assessing pain (n = 15),169 and the generic SF-36 (n = 6).363 The use of the very popular AOFAS hindfoot score is not without problems because this score has not been validated. This questionnaire has been shown to have enough discriminatory capacity to assess postoperative improvement in patients who underwent TAR.263 However, the research committee of the AOFAS published a policy statement recommending not to use this outcome assessment instrument.264 Hung et al166 developed a lower-extremity physical-function computerized adaptive testing instrument based on the Patient Reported Outcomes Measurement Information System (PROMIS) physical function items. This novel outcome instrument had high reliability and content and construct validity; therefore it should be used in patients with lower-extremity problems, including degenerative changes of the ankle joint.166 1. General or regional anesthesia can be used for TAR. 2. The patient is positioned supine with the feet on the edge of the table. A bump is placed under the ipsilateral hip until a strictly upward position of the lower extremity is obtained. 3. A pneumatic thigh tourniquet is applied. 4. If significant concomitant deformity has to be corrected, the unaffected lower extremity should be also draped to allow intraoperative comparison. 5. The surgical site is prepared in a sterile manner; in addition, a skin drape may be used. 6. After exsanguination by elevation, the thigh tourniquet is inflated. In most cases, a pressure of 250 to 350 mm Hg is sufficient. A total tourniquet time of 2 hours should not be exceeded. 7. A standard anterior ankle approach is used (Fig. 22-9). An anterior longitudinal incision (10-15 cm) is made in line with the extensor hallucis tendon (EHL) tendon. 8. The incision is brought down through the skin only. The medial fascicles of the superficial peroneal nerve’s medial branch are identified and dissected free into the foot. These are usually retracted laterally. Occasionally, the authors intentionally transect a fine fascicle, coursing medially across the neck of the talus to gain more exposure. Before the operation, the authors tell the patient not to be surprised postoperatively by areas of numbness along the medial aspect of the foot. 9. After the nerve has been carefully retracted and the anterior tibial tendon is identified, the authors open the extensor retinaculum in line with EHL tendon sheath and retract the EHL medially. The retinaculum is the thickening of the deep fascia above the ankle, running from tibia to fibula.1,255 10. During preparation of the soft tissue envelope, special attention is paid to the tibialis anterior vascular bundle, which is located behind the extensor hallucis longus or between the extensor hallucis longus and the extensor digitorum longus.314 11. The deep neurovascular bundle is gently teased free and retracted laterally. This preserves the lateral branch of the dorsalis pedis. This vessel supports the extensor digitorum brevis muscle, which is the best local muscle for the salvage of soft tissue coverage for anterior wound dehiscence. 12. The incision is deepened to the level of the joint. The authors to try to preserve the periosteum for later closure. In patients with rheumatoid arthritis or soft bones, the subperiosteal dissection can result in inadvertent malleolar avulsions. Care must be taken to do this gently in those at risk for bone injury. The EHL interval allows the surgeon to see into the lower lateral recessus with reflection of the anterior talofibular ligament. 13. After the ankle joint is sufficiently exposed, a capsulotomy is performed. 14. If a self-retaining retractor is applied to control the soft tissue envelope, it must be relieved when not necessary. Skin hooks should not be used much so as not to disturb wound healing. A deep blunt retractor used strategically at critical times for exposure may protect the tissues best. 15. After the joint is sufficiently exposed, the first step is to remove osteophytes on the tibia (especially on the anterolateral aspect) and the talar neck; however, the bone cortex should not be destroyed. 16. Implantation is performed by following the guidelines of the manufacturer. Every effort must be made to avoid injury to the “shoulder” region of the medial malleolus because this can cause intraoperative or postoperative malleolar fracture, a common intraoperative complication of TAR. Because the lateral malleolus in some patients is relatively more posterior, it can be inadvertently cut with approaches from front to back. 17. All distractors are removed, and the stability and motion of the ankle is checked. 18. The position of prosthesis components is checked and documented using fluoroscopy. 19. Wound closure is performed sequentially in layers, starting with the periosteum, then the extensor retinaculum, subcutaneous tissue, and skin. Skin is usually closed using 4-0 nylon. Drainage with suction may be used but is generally not necessary. 20. Soft wound dressing is used to avoid any pressure so as not to compromise wound healing. A splint is used to keep the foot in a neutral position. 21. Elevation for the first 2 days is absolutely critical. Some surgeons permit early motion. 22. The anterior approach can be used for ankle fusion procedures. It gives excellent visibility of the joint. Anterior plating (single plate or double plates)269 can be used to secure fixation. In some cases, a more limited incision than described here works very well and limits operative time and morbidity.
Ankle Replacement
![]() Video Clip 16)
Video Clip 16)
![]() Video Clip 18)
Video Clip 18)
![]() Video Clip 20)
Video Clip 20)
![]() Video Clip 17)
Video Clip 17)
![]() Video Clip 19)
Video Clip 19)
Short History of Total Ankle Replacement
First-Generation Total Ankle Designs
St. Georg–Buchholz Ankle Prosthesis
Imperial College of London Hospital Prosthesis
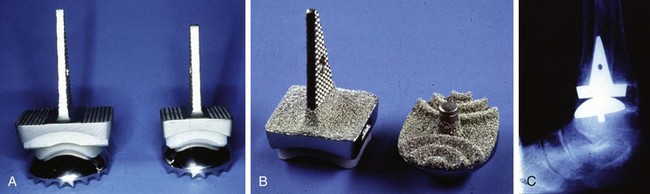
Irvine Total Ankle Replacement
Richard Smith Total Ankle Replacement
Conaxial Beck-Steffee Ankle Prosthesis
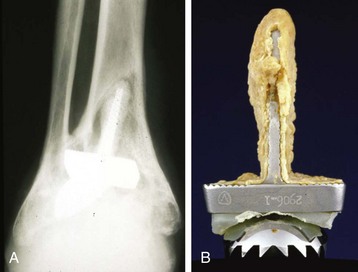
Newton Ankle Implant
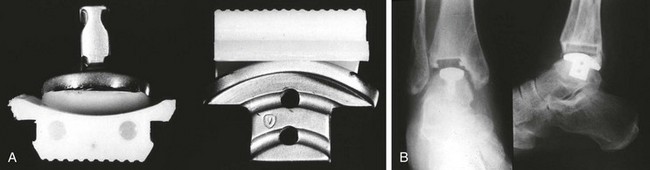
Bath-Wessex Total Ankle Replacement
Mayo Total Ankle Replacement
Oregon Ankle Prosthesis
Thompson-Richard Prosthesis
New Jersey or Cylindrical Total Ankle Replacement
Results of First-Generation Total Ankle Designs
Kinematics and Biomechanics of Total Ankle Replacement
Preoperative Planning
Indications for Total Ankle Replacement
Contraindications for Total Ankle Replacement
“Ideal Candidate” for Total Ankle Replacement
 Middle aged or older (sixth decade or older and, in general, the older the better)
Middle aged or older (sixth decade or older and, in general, the older the better)
 Low demands for physical and sports activities (e.g., hiking, swimming, biking, golfing)
Low demands for physical and sports activities (e.g., hiking, swimming, biking, golfing)
 No obesity/overweight (normal or slightly increased body mass index; however, obesity is not a contraindication for this procedure)17,26
No obesity/overweight (normal or slightly increased body mass index; however, obesity is not a contraindication for this procedure)17,26
 Good bone stock with no risk factors for impaired bone quality
Good bone stock with no risk factors for impaired bone quality
 Well-aligned and stable hindfoot
Well-aligned and stable hindfoot
 Good soft tissue (e.g., no previous surgeries of foot/ankle)
Good soft tissue (e.g., no previous surgeries of foot/ankle)
 Well-preserved preoperative range of motion
Well-preserved preoperative range of motion
 No neurovascular impairment of the lower extremity
No neurovascular impairment of the lower extremity
Preoperative Examination
Clinical Examination
Radiographic Examination
Pedobarography
Outcome Instruments in Studies on Total Ankle Arthroplasty
Surgical Technique
Surgical Technique Using an Anterior Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ankle Replacement