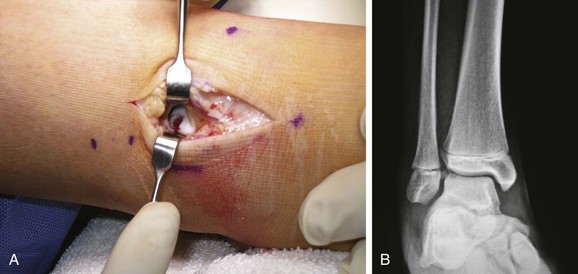
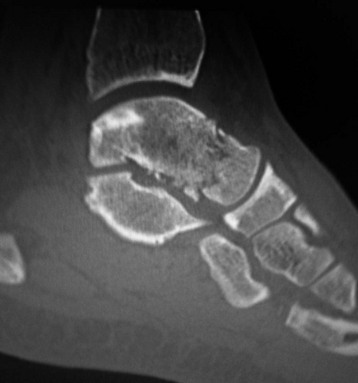
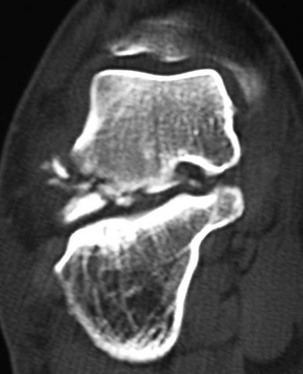
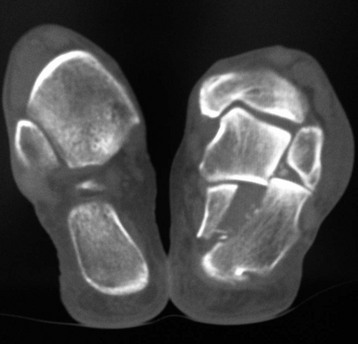
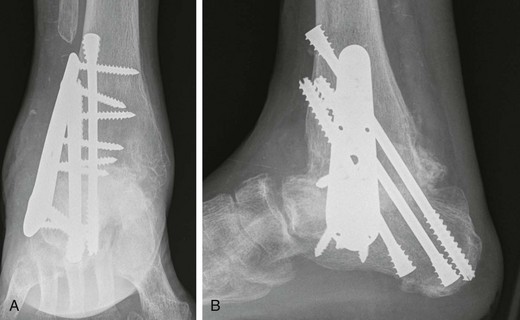
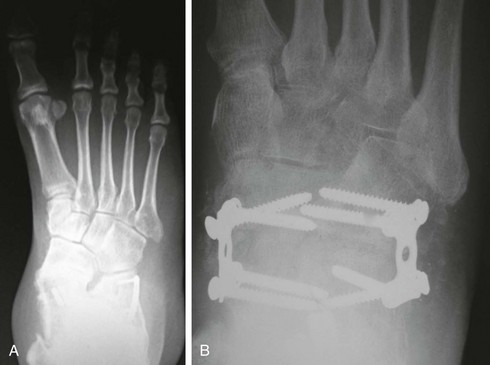
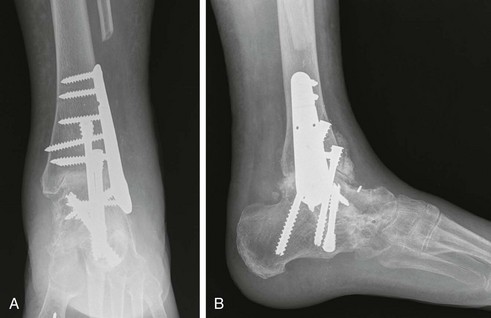
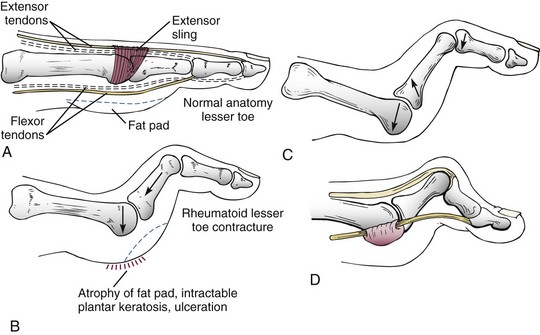
Chapter 19 ARTHRITIC CONDITIONS OF THE FOOT DEGENERATIVE ARTHRITIS OF THE HINDFOOT DEGENERATIVE ARTHRITIS OF THE MIDFOOT FIRST METATARSOPHALANGEAL JOINT ARTHROPLASTY UNCOMMON PROBLEMS ASSOCIATED WITH RHEUMATOID ARTHRITIS (Video Clips 33, 35, 36, 60, 75, and 76 Subluxation or Dislocation of a Single Metatarsophalangeal Joint Interphalangeal Joint Arthritis of the Hallux MISCELLANEOUS ARTHROPATHIES OF THE FOOT AND ANKLE DEGENERATIVE ARTHRITIS OF THE INTERPHALANGEAL JOINT (Video Clip 63 Arthritis is the destruction of articular cartilage, and it comprises one of the most common human diseases. Approximately one fourth of the population will develop foot pain during their lifetime, and a significant percentage of this is due to arthritis.201,548 Arthritic joint disease has affected man from the beginning. The 3300 BC Ötzi Ice Man, found high in the Alps between Austria and Italy, had arthritic joints.250 Older human specimens dating to 4500 BC show evidence of arthritis, and even prehuman Neanderthal specimens demonstrate changes consistent with arthritic disease. One early treatment for arthritis was made from the bark of the willow tree. The active ingredient was later isolated from the bark and named salicin. In 1853, Charles Gerhardt discovered a method to buffer salicin, forming acetylsalicylic acid, which reduced the gastrointestinal side effects; however, he had no interest in marketing the compound. While working for Bayer in 1897, Felix Hoffmann and Arthur Eichengrun503 further purified acetylsalicylic acid, and Hoffman used it to help his father, who was suffering from arthritis. Bayer patented and successfully marketed this compound as “aspirin.” Further discoveries continue to elucidate the various causes of arthritides. Three genes have recently been linked to the degenerative form of arthritis. In addition, all cartilage degeneration appears to have a final common mechanism of chondrocyte apoptosis (programmed cell death), regardless of the type of arthritis.291 Likewise, treatment of arthritis has gone far beyond aspirin; however, there remains much to learn in the diagnosis and treatment of this significant disease. Osteoarthritis of the foot and ankle occurs in all age groups. It occurs in middle and later years as primary idiopathic osteoarthritis (Fig. 19-1) and in a younger population after trauma—a type of secondary arthritis (Fig. 19-2A and B). The disease is characterized by an inherent defect in the chondrocytes and the cartilage matrix they produce. Early in the course of disease, chondrocytes multiply in number. Later they produce interleukin-1 (IL-1) and tumor necrosis factor (TNF), which inhibit the formation of proteoglycans and type 2 collagen. This in turn leads to degeneration and thinning of the cartilage layer. Three genes are now known to be linked to the osteoarthritic process, including GDF5 on chromosome 7 and MCF2L on chromosome 13.124 Microscopically, the normally smooth cartilage surface shows cracks and thinning. The synovium becomes fibrotic and hyperemic, with chronic inflammatory cell infiltratration. With repeated mechanical trauma, fragments of articular cartilage may break off into the joint, forming loose bodies (Fig. 19-3A and B). Physical examination often demonstrates swelling around the affected joint with restricted motion. Surrounding bursae may be inflamed. Crepitation is sometimes present, and with forced motion, pain may be elicited. Periarticular osteophytes are often obvious to palpation and may cause numbness because of compression of an overlying nerve (e.g., deep peroneal nerve coursing over dorsal first tarsometatarsal [TMT] joint) (Fig. 19-4). Skin ulcerations may develop on the plantar tarsometatarsal joints because of longitudinal collapse of the arch of the foot. Typical radiographic findings include joint space narrowing, subchondral sclerosis, subchondral cyst formation, intraarticular loose bodies, periarticular osteophytes, and loss of normal foot alignment. These findings are best demonstrated on weight-bearing radiographs (Fig. 19-5A). Brodén views are helpful for detecting arthritis of the subtalar joint. Talonavicular arthritis is often accompanied by a loss of the Meary angle (Fig. 19-5B), and calcaneocuboid arthritis is best seen on a medial oblique foot radiograph. Menz and colleagues375noted that osteoarthritis is readily diagnosed on anteroposterior (AP) and lateral radiographs and that these findings show good interobserver reliability. Periarticular bone loss and osteoporosis rarely occur. Magnetic resonance imaging (MRI) may show cartilage thinning and signal change on T2-weighted imaging in the subchondral bone. When subtler forms of arthritis are suspected, computed tomography (CT) is useful to document the severity and extent of the disease, although CT scans are routinely non–weight-bearing images. Van Saase et al573 noted the prevalence of first metatarsophalangeal (MTP) joint arthritis to be 28%, lesser MTP joints to be 8%, and the proximal interphalangeal (IP) joints to be 7%. The radiographic prevalence of midfoot and hindfoot joint arthritis has not been reported. Conservative treatment methods, such as weight reduction and activity modification, may reduce symptoms. Thus manual laborers who develop arthritis of the foot or ankle may see pain reduction with more sedentary occupations. Although rest is often advocated, animal studies have shown that increased activity diminishes the symptoms of arthritis and may slow its progression.203 Cross training may also be beneficial to reduce stress on affected joints while maintaining joint mobility (i.e., joggers may substitute cycling or swimming). Over-the-counter footwear or prescription footwear can reduce symptoms over bony prominences.115 Orthoses can support unstable areas and areas with rigid deformities. Semiflexible orthoses appear to be better tolerated than rigid orthoses in treating degenerative joint disease of the hindfoot and midfoot. Orthoses that may be considered include ankle–foot orthoses (AFOs) for ankle, hindfoot, and midtarsal deformities; rocker-bottom shoe modifications for decreased ankle, hindfoot, and forefoot motion; molded-leather ankle braces for hindfoot arthritis; and custom-made and prefabricated orthoses for midfoot and forefoot problems. The University of California Biomechanics Laboratory (UCBL) brace is designed to limit the motion of the subtalar joint. Nonsteroidal antiinflammatory drugs (NSAIDs) are often used as first-line pharmacologic treatment. However, concerns remain regarding potential gastrointestinal and cardiac side effects. All NSAIDs have been linked to an increased cardiac risk.501 Intraarticular corticosteroid injections can provide significant and sometimes prolonged clinical relief; however, the American College of Rheumatology recommends waiting at least 3 months between injections.10 Several studies have noted efficacy for up to 2 years; yet some patients experience much shorter relief. This difference is poorly understood. In larger joints, synovial fluid aspiration before steroid injection may increase effectiveness and duration and may reduce clinical relapse.584 Side effects include periinjection lipodystrophy; skin atrophy; postinjection flare-reaction (1%-10% of patients), thought to be caused by the crystalline preparation of the steroid); and facial flushing (15% more common in women). Prolonged steroid use has many side effects, including hypothalamic-pituitary axis suppression and hepatic gluconeogenesis, which worsens glucose intolerance among diabetics. Intraarticular injections have far less systemic side effects than oral preparations, and the effect is usually transient.425 Contraindications to intraarticular steroid injection include preexisting septic arthritis, surrounding cellulitis, injection into a prosthetic joint, preexisting fracture, or coagulopathy. Although septic arthritis has been reported after intraarticular injection (1 in 3,000 to 1 in 50,000 in the knee80) the risk is small with appropriate skin preparation and technique. Cartilage degeneration after intraarticular steroid injection has been noted in animals, but similar complications in humans have not been reported. Steroids may be effective regardless of the type of arthritis. Preoperative fluoroscopic-guided injections (Fig. 19-6) may help determine which joints would be improved by arthrodesis. However, the anesthetic/steroid mixture may leak to adjacent tarsometatarsal joints in up to 20% of cases.289 To date, there are no pharmacologic agents known to halt cartilage destruction or restore the cartilage matrix. However, Sampson and Hilton490 demonstrated that teriparatide (Forteo), a recombinant parathyroid hormone, increases proteoglycan content and inhibits cartilage degeneration in mice. Although this drug is used to treat osteoporosis, further studies may reveal other applications. A prior talar neck fracture (Figs. 19-7 and 19-8) accounts for 50% to 100% of posttraumatic subtalar joint arthritis.69 Pennal noted that up to 60% of patients with talar fractures required subsequent subtalar arthrodesis.433 In Sanders’ series, 37% of patients with talus fractures required a second surgery; 76% went on to subtalar arthrodesis, 23% had triple arthrodesis, and 11% had pantalar arthrodesis.491 Up to 17% of intraarticular calcaneal fractures will require a second surgery because of symptomatic subtalar arthritis.41 Sanders concluded that this is dependent upon the degree of comminution of the subtalar joint, because 23% of Sanders type II fractures, and 73% of Sanders type IV fractures required subtalar arthrodesis (Fig. 19-9).492 Subtalar arthrodesis in the nontrauma setting has reported success rates of 80% to 90% good-to-excellent results.485 Unfortunately, when performed in the setting of posttraumatic arthritis, good-to-excellent results are reported in only 50% to 60% of cases.350 Thermann noted 41% fair-to-poor results with secondary subtalar arthrodesis after calcaneal fracture,547 and Pennal noted poor results in his small series of early subtalar arthrodesis for talar neck fractures despite high fusion rates in both series. Flemister et al163 noted a fusion rate of 96% in a series of 86 subtalar arthrodeses resulting from complications after calcaneal fracture, yet patients only achieved a mean American Orthopaedic Foot and Ankle Society (AOFAS) Hindfoot score of 75 at 2-year follow-up. Because of poor results with secondary arthrodesis after calcaneal fractures, Huefner et al242 reported results of primary subtalar arthrodesis for comminuted calcaneal fractures. This team noted good-to-excellent results in 5 of 6 patients using the AOFAS scoring system. These differences in outcome between primary and secondary subtalar arthrodesis remain poorly understood.3 Complications after comminuted calcaneal fractures include a loss of calcaneal height, loss of talar declination, and anterior ankle impingement. For these patients, many have advocated a bone block subtalar arthrodesis to restore the calcaneal height, and talar declination. Garras et al179 reported on the use of frozen structural allograft for this purpose and noted a 90% successful fusion rate using structural autograft. Saville et al496 reported using the medial approach for hindfoot arthrodesis when severe valgus deformity is present. In their series, 10 patients underwent subtalar arthrodesis, 6 underwent subtalar and talonavicular arthrodesis, and 2 had triple arthrodesis. All wounds healed, and 17 of 18 patients went on to successful fusion over 5.6 months. The authors suggested that when the hindfoot is in extreme valgus, use of a medial approach may help avoid tension-related lateral wound problems and decrease sural nerve complications. Glanzmann and Sanhueza-Hernandez187 reported their results of arthroscopic subtalar arthrodesis. They noted a 100% fusion rate using a posterolateral portal (just lateral to the Achilles tendon) and an anterolateral portal (centered upon the sinus tarsi). Joint preparation is done primarily through the posterolateral portal with a shaver, curette, and motorized burr. Visualization is achieved via a 3.5-mm arthroscope through the anterolateral portal. Lee et al328 also reported arthroscopic subtalar arthrodesis but with prone positioning through two posterior portals (medial and lateral to the Achilles tendon). Scranton et al505 reported on a comparison of open versus arthroscopic subtalar arthrodesis and noted that there was no large difference in operative time: 58 minutes for the open procedure versus 63 minutes for the arthroscopic procedure. The main advantage of an arthroscopic approach is decreased wound issues. However, fusion rates and other parameters have not been shown to be superior to traditional approaches. Regardless of approach, hindfoot positioning during subtalar arthrodesis can be challenging. Optimally, the calcaneus should be in slight valgus (approximately 5 degrees) relative to the talus. Frigg et al172 suggested that visual inspection is inadequate to determine correct hindfoot position, and that the Saltzman-el-Khoury hindfoot alignment view should be used. This weight-bearing, posterior to anterior radiograph is aimed 20 degrees caudal, with the x-ray beam parallel to the medial border of the foot.486 Unfortunately, this is impractical in an operative setting.172 Thus visual inspection and fluoroscopic imaging are most commonly used to determine hindfoot position during surgery. Graft use (autograft, allograft, or bone substitute) and hardware configuration are additional options the surgeon must consider for hindfoot arthrodesis. The authors routinely use proximal tibial or iliac crest autograft and cannulated lag screw fixation to achieve compression across the joint (Fig. 19-10). Frigg et al171 reported on the use of porous tantalum interposition for ankle and subtalar arthrodesis and found that fusion was successful in nine of nine patients. Tantalum has been used for spine fusions and in the setting of hip and knee surgery. The advantage appears to be rapid ingrowth into the tantalum without donor-site morbidity. The incidence of calcaneocuboid joint arthritis after calcaneal fracture has been reported to be between 33% and 76%, with a higher percentage in joint depression-type fractures.142 However, those with fractures involving the actual calcaneocuboid joint are typically asymptomatic.294 Astion and Wulker15,599 both noted that an isolated calcaneocuboid fusion has little effect on the motion of the adjacent joints and that the motion of the calcaneocuboid is small. Isolated arthritis of the talonavicular joint (either resulting from trauma or degeneration) may require isolated fusion. However, arthrodesis of the talonavicular joint has a high nonunion rate. This is likely due to the spheric shape of the joint and the resultant difficulty in exposure and preparation of the joint surfaces. Published reports demonstrate a union rate between 63% and 97%.165,221 Chen et al82 reported a 94% union rate using either staples or screws without bone graft for isolated talonavicular joint fusions. Jarrell et al256 compared three methods of fixation and determined that there was no significant difference in load to failure between the three constructs. These studies support the notion that excellent joint surface preparation is more important than either fixation type or use of graft. Indications for talonavicular arthrodesis include isolated arthritis (Fig. 19-11), rheumatoid arthritis, or pes planovalgus deformity. Astion15 reported that isolated talonavicular joint fusion limits the subtalar joint to 8% of its native motion. In addition, fusing the talonavicular joint alone behaves similarly to the double hindfoot arthrodesis.546 The double arthrodesis (fusion of the talonavicular and calcaneocuboid joints) may be undertaken when these joints are diseased, while the subtalar joint is spared. Locking of the transverse tarsal joints results in an essentially immobile subtalar joint, and this double arthrodesis functions much like a triple hindfoot arthrodesis.89 Beischer et al28 noted that with a double or triple joint hindfoot fusion, the ankle joint range of motion during stance decreases by 33% while the ipsilateral knee range of motion increases by 13%. Citing less than desireable results after triple arthrodesis, Sammarco et al489 recommended a modified double arthrodesis of the subtalar and talonavicular joints. They noted that all of their patients were satisfied with the result, and only 1 of 16 patients required revision surgery for nonunion. Advantages of this type of double versus triple arthrodesis include reduced operative time and avoidance of potential calcaneocuboid nonunion (reported as 20% with the triple arthrodesis).24 The triple arthrodesis is regarded by many as a salvage procedure. Typical indications include posttraumatic hindfoot arthritis, rheumatoid arthritis, or stage III posterior tibial tendon dysfunction. It is a demanding procedure. The purpose is to restore plantigrade position of the foot, with the hindfoot in slight valgus. Not infrequently, a forefoot osteotomy is required to correct forefoot rotation in the coronal plane. Malunion is not uncommon and frequently leads to dissatisfaction for both the surgeon and patient. Resnick et al461 demonstrated that placing the calcaneus in too much valgus (Fig. 19-12) increases the force on the deltoid ligament by 76% during weight bearing. In contrast, a varus hindfoot places pressure on the lateral column and fifth metatarsal and may lead to lateral ankle instability and ankle arthritis. Figure 19-12 Anteroposterior (A) lateral (B) weight-bearing ankle radiographs after triple arthrodesis. Arthritis in adjacent joints (ankle and tarsometatarsal joints) has been reported after triple arthrodesis in up to 58% of patients in a 21-year follow-up.585 Nonunion and avascular necrosis have been reported. Graves200 and Beischer28 noted that 28% to 33% of their patients walked with a limp after triple arthrodesis despite successful fusion. For those with disabling hindfoot and ankle arthrosis, Acosta et al2 recommended pantalar arthrodesis involving the tibiotalar, subtalar, talonavicular, and calcaneocuboid joints (Fig. 19-13). Although 23 of 27 patients went on to solid fusion, there was a 37% complication rate, and only 5 patients had an excellent result. The authors suggested that, like the triple arthrodesis, this procedure be considered only as a salvage operation.2 Midfoot arthritis frequently develops as a sequela of a fracture or dislocation through the Lisfranc joint but may also develop spontaneously because of osteoarthritis or inflammatory arthritis. Thus it generally has a bimodal presentation: those with a traumatic etiology often seek care in their thirties, while those with a nontraumatic etiology often present in their fifties.270 Zonno and Myerson611 suggested that most midfoot pain is due to atraumatic osteoarthritis, although others maintain that trauma is the primary cause of arthritic change in the midfoot. Davitt et al123 hypothesized that midfoot degeneration is the result of metatarsal length differences. The authors noted that a longer second metatarsal correlated with midfoot arthritis. Wearing high-heeled shoes may also contribute to midfoot arthritis.606 It should also be noted that arthritis in any of the tarsometatarsal joints in the absence of a history of trauma may represent an early Charcot (joint) deformity. Charcot arthropathy can develop with diabetes as well as with peripheral neuropathy and other neurologic disorders (Fig. 19-14). Regardless of the cause, the development of midfoot arthritis can be an extremely disabling condition because of the stress placed on the longitudinal arch with weight bearing. A bony prominence may develop on the dorsal aspect of the midfoot because of osteophyte formation, which makes wearing shoes painful. A progressive flatfoot deformity can also develop from instability of the metatarsocuneiform (MTC) joint, with development of a plantar bony prominence and subsequent callus formation. Jung et al270 noted four presentations associated with tarsometatarsal joint arthritis: no deformity, pes planovalgus, hallux valgus, and the rocker-bottom deformity. Mann et al357 noted that 78% of patients with midfoot arthritis had abnormal foot posture and difficulty with shoe wear. With continued arthritic change, an abduction and dorsiflexion deformity of the midfoot occurs (Fig. 19-15). This progression of pain and deformity makes ambulation difficult. In examination of the foot, passive manipulation of the midfoot involves abduction of the forefoot and a pronation stress test to determine the location of maximal pain. The piano-key test (Fig. 19-16) is positive when a plantarly directed force applied to the metatarsal head elicits pain in the same tarsometatarsal joint. This is a sensitive indicator of a symptomatic joint or joints.282 A complicating factor with midfoot arthropathy is a simultaneous hindfoot deformity. Malalignment at the transverse tarsal joint and a valgus deformity of the hindfoot often are associated with severe midfoot arthritis. A careful preoperative physical examination is necessary to determine the extent of the midfoot and hindfoot malalignment. In the subtle cavus foot with degenerative arthritis, the Coleman block test helps to determine the need for associated hindfoot procedures, such as the addition of a calcaneal osteotomy or creation of plantar flexion through the first MTC joint, with the arthrodesis or opening wedge through the medial cuneiform (Fig. 19-17). Arthritic changes such as joint space narrowing can be seen on the weight-bearing anterior posterior radiograph. On the lateral radiograph, midfoot collapse of the tarsometatarsal joints may or may not be seen. The changes may also coincide with pes planovalgus deformities (forefoot abduction with midfoot collapse). Jung et al270 noted that with primary osteoarthritis of the tarsometatarsal joints radiographs demonstrate a lower medial cuneiform height than that of posttraumatic arthritis. Menz et al376 reported that foot structure differs in elderly patients with midfoot arthritis compared with those without. In those with radiographic evidence of naviculocuneiform and talonavicular joint arthritis, they noted significantly flatter feet as evidenced by a small calcaneal inclination and a larger calcaneal first-metatarsal angle. Conservative management of midfoot degenerative arthritis includes a soft or rigid custom-molded orthosis that provides support to the longitudinal arch. A full-length carbon fiber insert may also be used. Rao et al450 demonstrated that these orthotics significantly lessen the load duration and the intensity borne by the midfoot. Ibuki et al249 also reported that carbon fiber foot plates provided equivalent improvements in pain, activity levels, and walking ability when compared with custom-molded semirigid orthotics. Surgery consists of an arthrodesis of the involved midfoot joints. Most often, the second and third tarsometatarsal joints are involved. The first metatarsal medial cuneiform articulation is involved less often and the fourth and fifth metatarsocuboid articulation least often.304,447 Whether to include the intercuneiform articulations depends on inspection of these areas for arthrosis. Sangeorzan et al493 infrequently incorporated the intercuneiform joints (1 of 16), whereas Mann et al357 and Horton and Olney240 incorporated them in the arthrodesis technique more often. If any doubt exists, Mann et al357 suggest incorporating the intercuneiform joint within the arthrodesis. In the patient with a pes planus deformity and abduction of the forefoot, it is important to reestablish the normal alignment of the midfoot at surgery. This is accomplished by bringing the medial Lisfranc joint into normal alignment with the hindfoot by adducting and plantar flexing the first, second, and third MTC articulations. Although a lateral column arthrodesis is much more difficult to achieve, on occasion, it may be necessary to realign the entire Lisfranc joint in the presence of severe deformity. Komenda et al304 recommended reduction of the lateral column and temporary pin fixation until ambulation is initiated. They found a lateral column arthrodesis typically is unnecessary even in the presence of arthrosis (see Chapter 20). Promising results have been obtained with interposition arthroplasty for lateral column arthritis,36 and this procedure may be used as a second-stage procedure if needed for continued symptoms. Berlet et al36 performed tendon interposition for fourth and fifth tarsometatarsal arthritis and noted that 6 of 8 patients were satisfied. Shawen et al508 used ceramic sphere interposition. Their patients showed an 87% improvement in American Orthopaedic Foot and Ankle Society (AOFAS) scores and, 11 of 11 would undergo the procedure again. Alternatively, reliable results have been reported with arthrodesis of the fourth and fifth tarsometatarsal joints as isolated procedures or in combination with medial column arthrodesis for rocker-bottom deformities in neuropathic conditions.447 Multiple fixation methods have been described, including an in situ bone dowel technique,263 slot graft technique,298 plate and screw fixation,304,357 as well as Kirschner (K)-wire fixation with bone grafting.493 A plantarly placed plate and screws may offer a mechanical advantage over screws alone362; however, a comparison of a dorsomedial locking plate with crossed screws (Fig. 19-18) to secure the first metatarsocuneiform joint showed no significant difference in mechanical strength.206 Whether to perform reduction of a midfoot deformity has been a controversial topic. Johnson and Johnson263 reported on patients with mild and moderate midfoot deformities. They performed in situ fusions using K-wire internal fixation with a supplemental autogenous iliac crest graft technique. Nine of 13 patients (70%) reported good or excellent results and three nonunions. The most often fused joints were the second and third tarsometatarsal (66%) joints. In a review of 16 patients, Sangeorzan et al493 advocated reduction of the pes planus and abduction deformity and noted 11 of 16 cases with satisfactory results (69%). Few patients had excellent results or a normal foot, but many “returned to work.” Horton and Olney240 performed three in situ fusions and six realignment arthrodeses on eight patients (nine feet) for posttraumatic or degenerative arthrosis of Lisfranc joints. They used a five-hole, one-third semitubular plate that spanned the tarsometatarsal joint. An iliac crest graft was packed into the intervals between the tarsometatarsal joints and between the first and second metatarsals. The authors noted a strong correlation between reduction of the deformity and the outcome and reported seven of nine good and excellent results. Mann et al357 reported that 38 of 41 patients with primary, traumatic, or inflammatory arthrosis of the midfoot were satisfied. They advocated reduction of the deformity. Eleven patients had an autogenous bone graft placed at the time of arthrodesis. Komenda et al304 and Sangeorzan et al493 recommend that the lateral column not be included in the arthrodesis because this area is usually asymptomatic even with significant radiographic evidence of arthrosis. They emphasized that realignment of the midfoot contributes to a successful result. Komenda et al304 stated that if there is 15 degrees of malalignment in the transverse or sagittal plane or greater than 2 mm of displacement, reduction of the deformity is indicated. They did use temporary internal fixation when the lateral column was realigned but did not routinely perform arthrodesis for the lateral column. Shereff et al333 reported 81% successful results using iliac crest bone graft and K-wire fixation in 16 patients. They found that fusion of the fourth and fifth TMT joints was associated with significantly poorer functional and subjective scores. The use of an autogenous iliac crest graft often increases the success rate of arthrodesis. Sangeorzan et al493 stated that an additional graft was not necessary. Komenda et al304 used an ancillary graft in one third of cases and Mann et al357 in one fourth of cases. The current authors prefer to avoid using iliac crest unless structural defects require its use. However, the use of bone healing and enhancing substrates, such as platelet concentration systems, have shown promise. Han and colleagues demonstrated that platelet-rich plasma (PRP) enhances osteoinductivity.216 Landi et al317 noted an increase in fusion rates at 3 months as well as an increase in bone density by using a platelet gel in lumbar fusions. Hauschild229 reported on a successful fusion in a canine tarsal joint by using PRP. Gandhi et al176 reported on nine patients with foot and ankle nonunions. Using PRP and autologous bone graft at time of revision, the mean time to fusion was 2 months. Bibbo and colleagues44 also used PRP for foot and ankle fusions, concluding that PRP increased the fusion rate with low complications. Electrical, magnetic, or ultrasonographic bone stimulation can also be helpful. Several studies have reported on the positive influence of each of these modalities. Dhawan131 reported a faster time to fusion with the use of pulsed electromagnetic field (PEMF) therapy in hindfoot fusions. Patient satisfaction after midfoot fusion ranges from very good to acceptable. Nemec and colleagues410 noted 90% patient satisfaction. Mann et al357 reported an overall satisfaction of 86%, and Jung et al270 reported an 87% satisfaction. However, Baumhauer430 suggested that patients may only experience 60% reduction in pain. The magnitude of surgery requires a lengthy postoperative convalescence. After midfoot arthrodesis, most workers have difficulty returning to an occupation that requires standing for a full 8-hour day. Postoperative complications include skin slough, metatarsalgia, and incisional neuromas.43,304,357 Nonunion rates have been reported to be between 3% and 8%, but anecdotal evidence may point to a higher rate.270,341,410 Moreover, in a review of complications associated with midfoot and hindfoot arthrodesis, Bibbo et al43 reported that wound problems can be expected in 3% to 5% of nondiabetic patients undergoing elective arthrodesis procedures, but that rate increased up to 53% in diabetic patients (Fig. 19-19). Given the increasing numbers of diabetic patients in the United States and other countries, every effort should be made to prevent complications by evaluating and treating the vascular, neurologic, and general nutritional status of the patient before arthrodesis. Hindfoot alignment must be considered before midfoot arthrodesis as well, and concomitant osteotomies of staged hindfoot reconstruction, or both, should be considered. Rheumatoid arthritis (RA) is a systemic autoimmune disease characterized by synovitis, periarticular bone loss, and osteoporosis. It can affect both small and large joints, is generally symmetric, and affects both the upper and lower limbs.472 The disease affects 0.3% to 2.1% of the general population, and Rana449 has estimated that five million people in the United States suffer from rheumatoid arthritis. RA is two to four times more common in women than in men, yet no predilection exists for any single ethnic group.259 Onset can occur at any age, but the prevalence increases with age, peaking during the third to fifth decades. The disease course generally follows one of three pathways: (1) a relentless, destructive and aggressive course; (2) a monocyclic course notable for a single episode of synovitis without permanent cartilage damage; and (3) a polycyclic course with multiple episodes of attack followed by remissions. Up to 70% of cases follow the polycyclic course.521 The actual cause of the disease is unknown; however, genetic and environmental factors may play a role in etiology. Patients with an identical twin who has RA are four times more likely to develop RA than nontwin counterparts.336 Associations have also been found with viral infections, including cytomegalovirus, rubella, Epstein-Barr virus, and parvovirus.259 These viral agents may mimic portions of human leukocyte antigen (HLA) DR4, which stimulates the immune system to begin attacking the synovial lining of the joint in genetically susceptible individuals. Further etiologic studies are needed to fully elucidate the cause of RA. The disease can affect all joints of the body but has a predilection for the small joints of the hand and foot. Much attention has been centered on rheumatoid deformities of the hand in terms of initial involvement of individual joints; with acute onset, however, the feet are involved slightly more often than the hand (15.7% vs. 14.7%) (Short et al cited by Calabro65). Foot and ankle symptoms account for more than 50% of the presenting complaints in those initially diagnosed with RA. In addition, it has been estimated that 85% to 90% of patients with RA will eventually experience foot or ankle problems.565,569 Moreover, persons affected with mild-to-moderate rheumatoid arthritis with concomitant foot involvement have marked reduction in mobility and functional capacity.587 An increased incidence of foot problems occurs with duration of the disease process,380 and in chronic RA, Michelson380 reported that ankle and hindfoot symptoms were much more common (42%) than forefoot symptoms (28%) in a series of 99 patients followed in an outpatient setting. In chronic rheumatoid arthritis, symmetric involvement is common. Early on, however, asymmetric involvement may be observed. Early complaints of patients with RA involve poorly defined forefoot pain and metatarsalgia. Typically, these complaints result from synovitis and an intraarticular effusion, which lead to painful ambulation. Poorly defined metatarsalgia can indicate an interdigital neuroma; in time, however, synovitis and deformity can make the diagnosis more straightforward. Zielaskowski610 has reported an association of rheumatoid synovitis, nodule formation, and interdigital neuroma. A variable course of presentation occurs in the symptomatic rheumatoid foot. Nonspecific forefoot swelling is characterized by tenderness to palpation and pain on ambulation. The most common forefoot deformities are hallux valgus, subluxation or dislocation of the lesser MTP joints, and fixed hammer toe or claw toe deformities of the lesser toes (Fig. 19-20). In the early stages of rheumatoid arthritis, specific changes in the foot include inflammation of the synovium, with distention of the MTP joint capsule. Synovial proliferation leads to chronic capsule distention, resulting in loss of integrity of both the MTP joint supporting capsular structures and the collateral ligaments. With continued ambulation in the presence of soft tissue instability and with constant dorsiflexion stress on the MTP joints, subluxation and eventual dislocation occur.380,527 As the MTP joints of the lesser toes dislocate, the base of the proximal phalanx eventually comes to rest on the dorsal metatarsal metaphysis (Fig. 19-21). Progressive contracture of the long flexor tendons and the plantar intrinsic muscles lock the base of the proximal phalanx on the dorsal metatarsal neck. The proximal phalanx becomes fixed in a dorsiflexed position, creating a plantar-directed force on the metatarsal head.115 Simultaneously, the plantar fat pad is drawn distally, leaving only an extremely thin soft tissue covering on the plantar aspect of the metatarsal heads (Fig. 19-22). The loss of the protective plantar fat pad cushion, coupled with increased stress on the underlying skin, can lead to the development of intractable plantar keratotic (IPK) lesions and, in time, ulceration of the plantar skin (Fig. 19-23). The rheumatoid plantar fat pad is also significantly different than those of nonrheumatoid patients. Analysis with liquid gas chromatography demonstrates that the rheumatoid fat pad has a significantly higher ratio of saturated to unsaturated fat, as well as a higher viscosity. This is thought to reduce absorption of energy with foot strike, which may contribute to development of IPK lesions.460 Michelson et al380 reported that within the first 1 to 3 years of rheumatoid arthritis, 65% of patients are noted to have MTP synovitis. With chronic rheumatoid arthritis, Vidigal et al575 and others369,527 have reported that approximately two thirds of patients develop subluxation and dislocation of the lesser MTP joints (Fig. 19-24). Michelson et al380 and others369,565,575 have reported that the incidence of hammer toe or claw toe deformity of the lesser toes varies from 40% to 80%. Hallux valgus increases in incidence and severity in the chronic stages of rheumatoid arthritis.65 Michelson et al380 and others527,565,575 have reported a high incidence of hallux valgus in patients with chronic rheumatoid arthritis (59%-90%). With progressive clawing of the lesser toes, little lateral stability is afforded to the great toe, and the hallux migrates laterally to a fixed position either under or over the second and third toes. Progression of the rheumatoid process includes destruction of articular cartilage and resorption of subchondral bone, which tends to destabilize the hallux. As the hallux valgus deformity worsens, the weight-bearing function of the first ray lessens and a greater proportion of weight is borne on the lesser metatarsal heads. Craxford et al117 reported increased pressure beneath the second and third metatarsal heads with chronic rheumatoid arthritis. With time, the total number of diseased forefoot joints increases, as does the severity of the disease.244 In a longitudinal study, van der Leeden et al569 studied newly diagnosed patients with rheumatoid arthritis over an 8-year span, specifically looking at clinical impairment and walking disability. On presentation, 67% of patients had clinically painful and swollen MTP joints, which decreased to 40% to 50% over a 2-year period, while being treated medically. Even though the clinical numbers appeared to stabilize, the severity of radiologic forefoot damage increased. Once forefoot disease is present, deformity tends to progress rapidly over time, especially in the absence of pharmacologic treatment. Vidigal et al575 reported midtarsal joint involvement in approximately two thirds of patients with chronic rheumatoid arthritis. Chronic synovitis and eventual chondrolysis of the tarsometatarsal joints often occur with chronic disease. Associated with this, flattening of the longitudinal arch occurs in approximately 50% of patients.527 With disease progression, the talar head assumes a plantar medial position (Fig. 19-25) as the soft tissue structures supporting the talar head become attenuated. This midfoot collapse may have a mutlifactorial etiology. Several reports have linked arthritis and ligamentous laxity to pes planus, although others have indicated posterior tibial tendon rupture as the source.135,281,295 In reality, all of the above likely contribute to the clinical picture. Often with pes planus, a valgus deformity of the hindfoot occurs. The resultant ambulatory pattern is a shuffling, flat-footed steppage gait. Fu and Scranton173 noted that with progressive rheumatoid arthritis the foot changes to a passive weight-bearing platform for ambulation. Usually, because of the limitation of motion at the midfoot joints, a fibrous or bony ankylosis develops, but reduced motion is rarely restrictive. Vainio565 reported that 72% of women and 59% of men with chronic rheumatoid arthritis had involvement of either the midtarsal or the subtalar joint but that surgical intervention was relatively infrequent. Clayton91 reported that the forefoot was involved 10 times more often than the hindfoot. Kavlak278 noted that patients often show an obvious hindfoot valgus position and that a varus hindfoot is seldom seen (Figs. 19-26 and 19-27). Changes in the hindfoot occur with much longer duration of rheumatoid arthritis. Spiegel and Spiegel527 observed that in patients with rheumatoid arthritis of less than 5 years’ duration, only 8% demonstrated hindfoot arthrosis, whereas in those who had had rheumatoid arthritis longer than 5 years, 25% were symptomatic. They concluded that hindfoot arthrosis was an acquired deformity that developed from the mechanical stress of weight bearing. The underlying pathophysiology with hindfoot involvement relates to progressive destruction of the capsular and ligamentous supporting structures of the subtalar joint. Because subtalar joint function is intimately associated with transverse tarsal joint function, instability of these joints can result in altered function and gait. Often, the end result is a progressive pes planovalgus deformity of the hindfoot (Fig. 19-28). Posterior tibial tendon dysfunction with rheumatoid arthritis can lead to a unilateral progressive flatfoot deformity as well.135,360 Keenan et al281 reported that pes planovalgus deformities in patients with rheumatoid arthritis resulted from exaggerated pronation forces on the weakened and inflamed subtalar joint. They demonstrated with electromyographic studies that an increased period of activity of the tibialis posterior muscle occurred, which was interpreted as an “attempt to stabilize” an unstable foot. Flattening of the longitudinal arch also can develop secondary to naviculocuneiform joint deterioration or first metatarsocuneiform joint collapse. In some patients, severe valgus of the hindfoot may be associated with a concomitant valgus deformity of the ankle joint as well (Fig. 19-29). Gait analysis of patients with chronic rheumatoid arthritis when compared to those of nonarthritic subjects demonstrates delayed and reduced forefoot loading, resulting in a shorter stride length.419 This effect may be related to pain in the forefoot which, in turn, causes a reduction of the functional lever arm of the foot during push-off. Platto et al439 reported an association between impaired ambulation and foot deformity. They observed a greater association between hindfoot disease and gait impairment compared with forefoot disease.439 On the other hand, Shi et al512 studied 100 feet with rheumatoid arthritis and reported no correlation between a loss of arch height and hallux valgus or forefoot splaying. The classic radiographic signs of rheumatoid arthritis are that of a synovial inflammatory disease. The hyperemia involved with acute synovitis leads to periarticular osteoporosis,207 and early radiographic examination might reveal only soft tissue swelling and diffuse juxtaarticular osteoporosis. In contrast, normal bone mineralization is usual in psoriasis, reactive arthritis, ankylosing spondylitis, and crystalline arthropathies. Synovial inflammation eventually leads to marginal cortical erosions188 at the reflection of synovium and capsule attachment (Fig. 19-30). These peripheral erosions eventually progress to central erosions with resultant joint space narrowing, subluxation, and dislocation. Eventual destruction of the articular cartilage occurs as the rheumatoid pannus spreads around the cartilaginous surface. The articular cartilage is thought to be destroyed by proteolytic enzymes, resulting in joint space narrowing.64 Gold and Bassett188 noted that rheumatoid arthritis tends to strike earliest at the first, fourth, and fifth MTP joints. They reported that the medial aspect of the first, second, third, and fourth metatarsals and the lateral aspect of the fifth metatarsal were involved initially. The earliest visible erosions probably occur on the lateral aspect of the fifth metatarsal. The IP joints are typically spared except for the hallux.535 Of interest, in patients with preexisting periarticular erosions, the erosions progress with time, whereas in those patients with preexisting joint space narrowing, it is the joint space narrowing that progresses with time. These two processes seem to be independent of one another.567 Midfoot and hindfoot changes include midfoot collapse, pes planus, and subtalar sclerosis. Localized inflammation in the areas of the retrocalcaneal bursa and at the attachment of the Achilles tendon and plantar aponeurosis are common with long-standing disease (Fig. 19-31). Gold and Bassett188 reported the talonavicular joint is typically the first tarsal joint to be involved. Although radiographic midfoot arthritic changes are seen in up to 62%, clinically, these are far less symptomatic (27%).575 In a series of patients with rheumatoid arthritis who were evaluated with CT scans, Seltzer et al506 noted talonavicular joint involvement in 39%, calcaneocuboid involvement in 25%, and subtalar involvement in 29%. Radiographically, the subtalar joint is involved to a lesser extent than the midfoot, with changes noted in 32% to 42% of patients. Only 21% of rheumatoid arthritis patients actually have clinical symptoms in the hindfoot.380,575 Rarely are all three of the hindfoot joints simultaneously affected.251 Hattori and colleagues227 noted two distinct patterns of pes planovalgus deformities in the rheumatoid foot. One group demonstrated degenerative changes in both the subtalar and talonavicular joints, with the talar head subluxated plantarward in relation to the navicular. A second group showed only subtalar joint involvement. Neither group demonstrated involvement of the calcaneocuboid joint. Radiographic progression of rheumatoid arthritis can be evaluated by various methods, but commonly used methods are those described by Larsen,321 Rau,451 and Steinbrocker.533 The methods of Rau and Larsen were found to be equivalent, as reported by Tanaka et al542 in assessing progression of early rheumatoid arthritis, which indeed affects pharmacologic treatment. Moreover, the magnitude of 5-year disability as measured by the Health Assessment Questionnaire Disability Index (HAQ-DI) was associated with joint space–narrowing scores in the first year rather than periarticular erosion.346 Lindqvist et al334 noted more rapid radiographic progression in those patients with higher levels of inflammatory markers, such as sedimentation rate and rheumatoid factor. Another report suggested that 59% of 190 patients with early rheumatoid arthritis could be classified as nonprogressive based on radiographic joint changes432 and that radiographic progression may be slowed by treatment with disease-modifying antirheumatic drugs (DMARDs) and other pharmacologic agents, including antibiotics (sulfonamides, doxycycline), salicylates, cytotoxic drugs (methotrexate, leuprolide acetate, cyclophosphamide), NSAIDs, corticosteroids, and cytokine inhibitors (etanercept, infliximab). In patients with nonspecific pain or diffuse foot pain, or both, with no visible radiographic findings and subtle or minimal clinical findings, a technetium-99 (99Tc) bone scan can help to localize disease (Fig. 19-32).421
Arthritis of the Foot and Ankle
![]() )
)
![]() )
)
Arthritic Conditions of the Foot
Overview
Degenerative Joint Disease
History and Physical Examination
Radiographic Examination
Treatment
Degenerative Arthritis of the Hindfoot
Subtalar Arthrodesis
Calcaneocuboid Arthrodesis
Talonavicular Arthrodesis
Double Arthrodesis
Triple and Pantalar Arthrodesis

Degenerative Arthritis of the Midfoot
Treatment
Inflammatory Arthropathies
Rheumatoid Arthritis
History and Physical Examination
 Stage I: Discomfort and synovitis; no bone deformity or significant joint space narrowing
Stage I: Discomfort and synovitis; no bone deformity or significant joint space narrowing
 Stage II: Early involvement with flexible deformity; minimal erosive changes
Stage II: Early involvement with flexible deformity; minimal erosive changes
 Stage III: Fixed soft tissue deformity; significant erosive joint changes
Stage III: Fixed soft tissue deformity; significant erosive joint changes
 Stage IV: Severe hallux valgus, dislocation of the lesser MTP joints with fixed hammer toe or claw toe deformities, pes planovalgus (flatfoot), and hindfoot arthroses; articular destruction on radiographs
Stage IV: Severe hallux valgus, dislocation of the lesser MTP joints with fixed hammer toe or claw toe deformities, pes planovalgus (flatfoot), and hindfoot arthroses; articular destruction on radiographs
Forefoot
Midfoot
Hindfoot
Imaging Modalities
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Arthritis of the Foot and Ankle