Peroneal Tendon Injuries
Alex Kline
Mollie Manley
Dane Wukich
BACKGROUND/ANATOMY
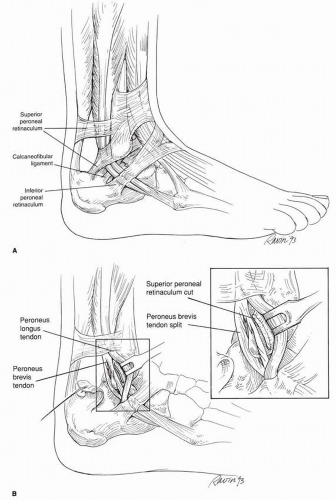
Peroneal tendon disorders are frequently missed and can be a source of lateral ankle pain in athletes (1). Several common pathologies can affect the peroneal tendons in the athletic population, including tendonitis, tears, and instability. The peroneus longus and brevis muscles form the lateral compartment of the leg and are innervated by the superficial peroneal nerve. The peroneus brevis originates from the lateral surface of the middle one third of the fibula and intermuscular septum and inserts at the peroneal tuberosity at the base of the fifth metatarsal. It acts primarily as an everter of the ankle joint and also provides some lateral ankle stability. Its primary antagonist is the tibialis posterior. The peroneus longus originates from the lateral condyle of the proximal tibia and the head and lateral aspect of the fibula. Distal to the tip of the fibula, it crosses the peroneal tubercle and turns sharply to obliquely cross the plantar aspect of the foot, inserting on the plantar aspect of the first metatarsal base. Its primary action is to plantarflex the first ray and also to assist in eversion of the foot. Its primary antagonist is the tibialis anterior. In its muscular portion, the peroneus longus lies posterolateral to the peroneus brevis. At the level of the ankle joint, the longus tendon lies posterior to the peroneus brevis, which hugs the posterior aspect of the fibula (Fig. 52.1).
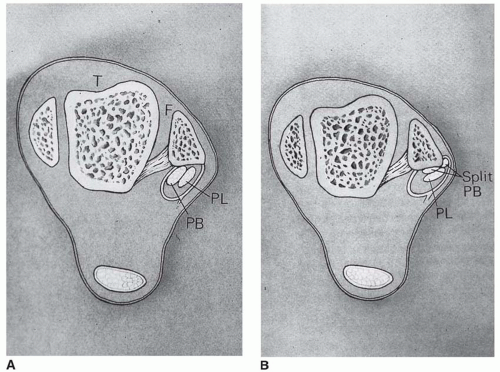
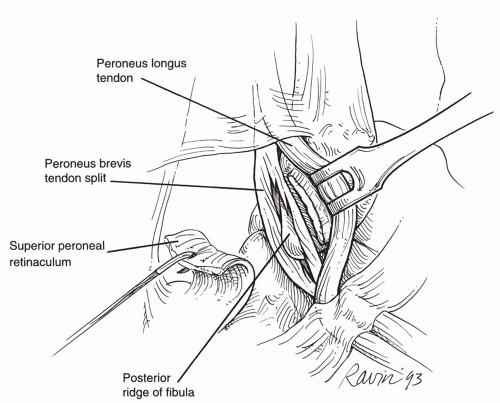
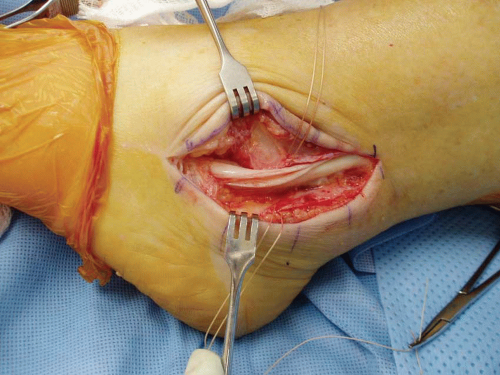
Approximately 4 cm proximal to the distal end of the fibula, the peroneal tendons enter a common synovial sheath. At the level of an ankle, the tendons course through a fibroosseous tunnel bordered anteriorly by the fibula; medially by the calcaneal fibular ligament, the posterior inferior tibiofibular ligament, and the posterior talofibular ligament; and posterolaterally by the superior peroneal retinaculum. The superior peroneal retinaculum acts as the primary restraint to subluxation and dislocation of the peroneal tendons and is always torn in an acute peroneal tendon dislocation (Fig. 52.2). In the majority of patients, the posterior aspect of the distal fibula forms a recess or groove (the retromalleolar groove), and this concavity deepens the area available for the peroneal tendons. Flattening or convexity of this groove may predispose patients to subluxation and tearing (2) (Fig. 52.3). Approximately 1 cm distal to the tip of the fibula, the peroneal tendons enter distinct synovial sheaths and head to their respective insertion sites.
Several distinct pathologic processes can affect the peroneal tendons in the athletic population. These include tenosynovitis/tendonopathy, tendon tears, tendon subluxation, and ganglion cyst formation (Fig. 52.4). Tendonitis or tenosynovitis of the peroneal tendons involves inflammation within the tendon sheath of either the peroneus longus or peroneus brevis. Generally, it results from prolonged repetitive activity such as that seen with dancers and distance runners. They develop chronic lateral ankle pain, with swelling and tenderness along the course of the involved tendon. This is also commonly seen concomitantly with lateral ankle instability. Subluxation or frank dislocation of the peroneal tendons can occur acutely as the result of athletic endeavors when a sudden dorsiflexion inversion injury of the ankle is sustained with a simultaneous violent peroneal muscle contraction. This generally causes the superior peroneal retinaculum to peel off of its fibular insertion. This has been classically described in the skiing population but also occurs in football, tennis, basketball, soccer, and ice skating.
Longitudinal tendon tears may affect either the peroneus longus or the peroneus brevis (Fig. 52.5). Acute tears in the athletic population generally result from sudden inversion injuries. Theoretical mechanisms of the injury include impingement of the peroneus brevis between the longus tendon and the posterior aspect of the fibula, split tears that occur in the setting of instability as the tendons sublux out of the retromalleolar groove, and a low-lying peroneus brevis that “overstuffs” the retrofibular groove. Peroneus brevis tears tend to occur in the retromalleolar sulcus, while longus tears often occur distal to the tip of the fibula near the peroneal tubercle.
PREOPERATIVE EVALUATION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree