Fig. 9.1.
Initial radiographs at first consultation.
The arthrocentesis was performed after the patient had been off of antibiotics for 3 weeks. Synovial fluid analysis revealed a synovial white cell count of 24,000 with 90 % polymorphonuclear cells. An extensor mechanism tear was suspected due to the lack of knee extension and a history of previous tibial tubercle osteotomy. Thus, a repeat two-stage exchange arthroplasty was performed.
9.2 Diagnosis/Assessment
The patient was diagnosed with a chronic right knee PJI. The diagnosis of PJI remains challenging due to confounding factors and lack of a gold standard test. The definition was first standardized by the Musculoskeletal Infection Society workgroup in 2011 [1]. This was later modified in 2013 by the International Consensus Meeting (ICM) on PJI [2]; the definition consisted of two major criteria and five minor criteria that must be present for diagnosis (Table 9.1). PJI is confirmed when one major or three minor criteria are met.
Table 9.1.
Periprosthetic joint infection (PJI) definition according to the International Joint Commission.
PJI is present when one of the major criteria exists or three out of five minor criteria exist | |
|---|---|
Major criteria | 1. Two positive periprosthetic cultures with phenotypically identical organisms |
2. A sinus tract communicating with the joint | |
Minor criteria | 1. Elevated serum CRP AND ESR |
2. Elevated synovial fluid white blood cell count OR ++change on leukocyte esterase test strip | |
3. Elevated synovial fluid polymorphonuclear neutrophil percentage | |
4. >5 neutrophils per high power field in 5 high power fields (400×) | |
5. A single positive culture | |
The American Academy of Orthopedic Surgeons (AAOS) has developed a clinical guideline to successfully diagnose PJI [3]. The guideline acts as a flowchart as opposed to a fixed protocol. The initial step is risk stratification of individuals to determine whether or not they are at high or low risk of developing PJI. In this particular case, the patient was considered to be at higher risk because he exhibited two symptoms related to PJI: pain and stiffness [3]. Along with increased temperature, the knee was swollen. A positive history of PJI and obesity are risk factors that are supported in the literature [4, 5]. Another important aspect of this case is early implant loosening (<5 years), which has been associated with a positive likelihood ratio (LR) of infection of 2.1 (1.36, 3.25; 95 % confidence interval [CI]) and a negative LR of 0.53 (0.29, 0.96; 95 % CI).
The next step involved investigating ESR and CRP. The ICM thresholds for chronic infections are stated [3] as >30 mm/h and >10 mg/L for ESR and CRP, respectively. Recently a positive leukocyte esterase test was added as a minor criterion, according to the ICM [2]. If the inflammatory markers are negative, the probability of infection is unlikely (negative LR: 0.0–0.06) and infection can be ruled out. However, if both are positive (positive LR: 4.3–12.1), a conclusive diagnosis of infection is not established and warrants further workup due to many variables and diseases that can skew the final result of the inflammatory markers. Positivity of the markers stratifies the patient into the high-risk group for infection and means that the patient needs further investigation.
If positive inflammatory markers are identified, a synovial fluid sample should be obtained. The superolateral approach is preferred to obtain synovial fluid from the knee; the use of contrast or local anesthetic should be avoided, since their antimicrobial activity may lead to a false negative [6].
The patient should be taken off antibiotic therapy for at least 2 weeks prior to obtaining intra-articular cultures [7]. The fluid should be tested for synovial white cells and polymorphonuclear cells, with a threshold for chronic PJI of >3,000 (cells/μ[mu]l) and >80 %, respectively, for chronic infections [3].
9.3 Management
The patient underwent the first stage of treatment, which consisted of removing all the prosthetic components, bone cement, and foreign material; and an extended synovectomy and implantation of a dynamic spacer with antibiotic-loaded bone cement. The extensor mechanism was intact and the tibial tubercle osteotomy had consolidated. Two cultures were positive for Staphylococcus coagulase negative and the infectious disease team was consulted, recommending intravenous vancomycin for 6 weeks. The patient was seen by a physical therapist, an occupational therapist, and a social worker, postoperatively. At discharge, he was able to toe-touch weight bear and was placed in a hinged brace that restricted range of motion from 0° up to 60°.
After a course of antibiotics, the knee remained swollen and painful during gait. Inflammatory markers remained above normal. Throughout this time the patient suffered from multiple urinary tract infections, which could have affected the results of the inflammatory markers. The synovial fluid cell count decreased compared to initial values but remained abnormal. On plain films, it was noted that the tibial component had failed and shifted anteriorly (Fig. 9.2). Three months after the first stage of the procedure, there was a high suspicion of persistent infection, and the patient was scheduled to undergo a spacer exchange and repeat I&D.
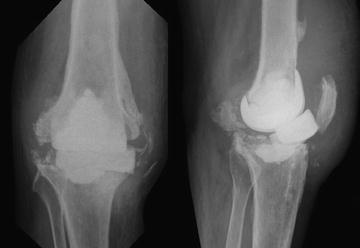
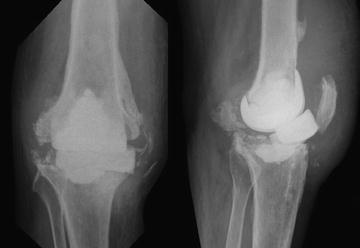
Fig. 9.2.
AP and lateral view of the initial dynamic spacer showing the anterior shift of the tibial component.
A new dynamic spacer was implanted and a thorough synovectomy was performed with removal of all foreign material. Clinically, the appearance of the knee was benign. Cultures taken during the spacer exchange procedure were all negative. With intraoperative findings, negative cultures, and a clinical improvement during the follow up period, the patient was scheduled for reimplantation at 5 weeks after the spacer exchange.
Reimplantation occurred without any complications (Fig. 9.3). At the time of reimplantation, two cultures were positive for Candida ssp. Given these findings, the infectious disease team recommended placing the patient on long-term suppressive therapy, including antibiotics and antifungal therapy. Within the first year of reimplantation, the patient presented with mild effusion and minimal pain, tolerating gait without external support. Two years after reimplantation, pain and swelling increased and the patient’s function diminished. The inflammatory markers were noted to increase and a new synovial aspiration was demonstrated to be above the threshold cell count. The patient was considered to benefit from a new I&D, although intraoperatively the decision was made to perform a two-stage exchange arthroplasty. At this time a static spacer that contained antibiotic and antifungal loaded cement bone was chosen. In follow-up, the patient sustained a diaphyseal peri-spacer femoral fracture (Fig. 9.4). The fracture was managed nonoperatively due to lack of pain. At this point the patient was not considered a suitable candidate for reconstruction; he was placed on lifelong antibiotic suppression therapy and was able to walk with the use of external support and a brace.










