Femur
Tibia
Patella
Increasing age
Female sex
Patella resurfacing
Female sex
Revision surgery
Revision surgery
Osteoporosis
Long diaphyseal stems
Over-resection of patella
Rheumatoid arthritis
Implant loosening
Osteonecrosis of patella
Neurological conditions
Tibial tubercle osteotomy
Large central peg
Osteolysis
TKR malalignment
Revision surgery
Lateral release
Stiff TKR
Excessive fat pad resection
Ipsilateral stemmed THR and TKR
Osteopenia represents the greatest risk factor for periprosthetic fractures. It can also occur secondarily to prolonged use of steroids, excessive alcohol consumption and inflammatory arthritis. Neurological abnormalities, osteolysis, large anterior femoral notching, knee stiffness and revision TKR can be considered as independent risk factors.
13.3 Femoral Fractures
Typically females have a higher risk of sustaining a periprosthetic femoral fracture [4]. This is partly due to the fact that osteoporosis and osteolysis increase the prevalence of these fractures. It is unclear to what extent anterior femoral notching during primary TKR has a significant influence on the occurrence of supracondylar fractures. Biomechanical studies demonstrated high stresses at the notch site and the authors believe that under some circumstances notching could increase the risk of a periprosthetic fracture [5]. Large clinical studies have been unable to demonstrate a clear relationship between notching and occurrence of a fracture [6, 7]. Modern condylar TKR design often has an anteriorly sloped flange, which makes the TKR instrumentation less prone for anterior notching. It will be interesting to see if such designs lead to overall reduced rates of supracondylar fractures. Most fractures occur after a low energy trauma such as a simple fall from a standing height [8]. Intraoperative periprosthetic fractures usually happen whilst preparing the box or seating the implant in posterior stabilised TKR components.
There are multiple risk factors for periprosthetic femoral fractures. Femoral notching is closely scrutinised because it is a surgeon-controlled risk factor, although its clinical relevance is unclear.
13.4 Tibial Fractures
Periprosthetic tibial fractures are also more prevalent in females [9]. In contrast to femoral fractures, they are more frequently associated with a loose prosthesis. Osteolysis is often associated with fractures around the tibial baseplate [10]. Tibial shaft fractures are usually seen in patients with long-stemmed or poorly aligned implants and in association with tibial tubercle osteotomy [10].
Tibial periprosthetic fractures are associated with female sex, implant loosening, revision surgery, long diaphyseal stems and tibial tubercle osteotomy.
13.5 Patellar Fractures
Patellar fractures are one of the rarest but most complicating forms of periprosthetic fractures after TKR. Fractures predominantly occur in resurfaced patellae. One study found a rate of only 0.05 % in non-resurfaced patellae as compared to the literature rates of 0.5–3.6 % for resurfaced patellae. In addition, intraoperative fractures of the patella are very rare except in the revision situation [4]. The risk factors for patellar fracture are shown in Table 13.1. A defined event causing the fracture is also unusual, with most fractures being recognised on routine follow-up radiographs [11, 12].
Malalignment of TKR increases the risk of patellar fracture, probably due to the increased patellofemoral contact forces. The resulting clinical outcome following treatment of a patellar fracture in malaligned TKR is clearly inferior to those with perfectly aligned TKR [13]. Fractures are more prevalent in males than females [12] Excessive resection of the patella increases the risk of occurrence of a patellar fracture; the thickness of the remaining patella should be at least 12–15 mm to reduce this risk.
The blood supply of the patella is another important factor to consider. It has been shown that the patella has an extraosseous and an intraosseous blood supply. The extraosseous blood supply comes from a vascular anastomosis that encircles the patella and consists of the supreme geniculate artery, the medial superior geniculate artery, the medial inferior geniculate artery, lateral superior geniculate artery, lateral inferior geniculate artery and the anterior recurrent tibial arteries. The intraosseous blood supply comes from two sources, the mid-patellar vessels that enter through foraminae in the middle third of the anterior surface of the patellar and the infrapatellar anastomosis behind the patellar tendon [14]. A lateral release may compromise the blood supply, therefore increasing the risk of patellar fracture. This is particularly true when combined with a medial parapatellar approach [13]. An excessive fat pad resection may also damage the blood supply to the patella [11].
Patellar fractures are a rare complication, predominantly associated with resurfaced patellae. Malalignment increases the risk of patellar fracture, and the patellar blood supply should be kept in mind when performing TKR.
13.6 Classification Systems
Classification systems are useful for the surgeon if they guide further treatment and give information on the prognosis after fracture treatment.
The factors important in any classification are:
The location of the fracture with regard to the prosthesis, whether the component is well fixed or loose and consideration of the available bone stock. No classification is perfect and currently there is no recognised classification for inter-prosthetic fractures.
A brief overview about the most commonly used classifications is given below.
13.6.1 Femoral Fractures
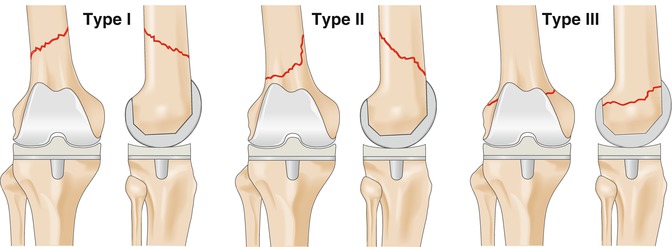
The most frequently used classification for femoral fractures is the Lewis and Rorabeck [12] (Fig. 13.1). They grade fractures into type 1 which are undisplaced with a stable prosthesis, type 2 which are displaced fractures with a stable prosthesis and type 3 which have a loose or failing prosthesis with an undisplaced or displaced fracture. They suggest that type 1 fractures are treated conservatively. Type 2 fractures are treated with open reduction and internal fixation with either an intramedullary nail or plate. Type 3 fractures require revision arthroplasty with usually long-stemmed implants or distal femoral replacement. A criticism of this classification is that it does not take into account the proximity of the fracture line to the implant. This is of importance as very distal fractures may not have sufficient bone stock available for retrograde locking screws or screws for locked plates.
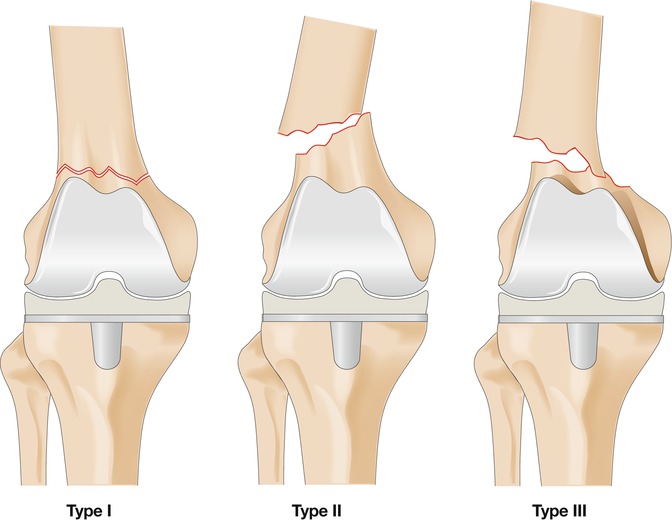
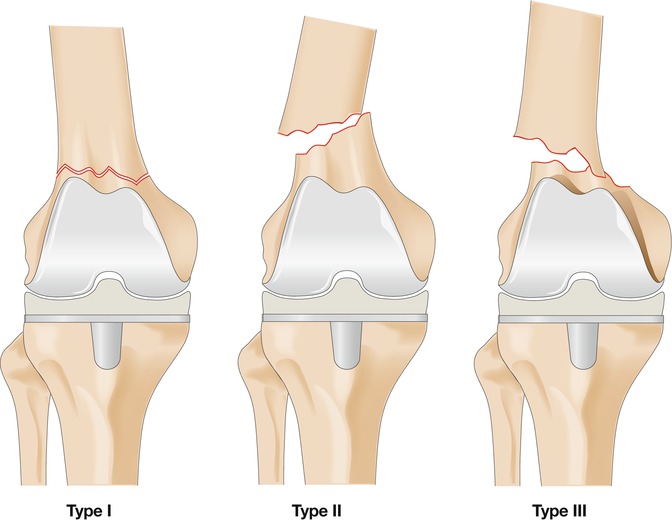
Fig. 13.1
The Lewis and Rorabeck classification for periprosthetic fractures. Type I: undisplaced fracture; prosthesis intact. Type II: displaced fracture; prosthesis intact. Type III: displaced or undisplaced fracture; prosthesis loose or failing
More recently developed classifications by Backstein et al. [13] (Fig. 13.2) and by Su [14] (Fig. 13.3) are based around the distance of the fracture from the prosthesis. An advantage of the Backstein classification is that it can be applied to the femur and the tibia. Another new classification developed by Kim et al. guides treatment by classifying fractures according to whether the fracture can be reduced, the bone stock available and whether the implant is well fixed or loose [15].
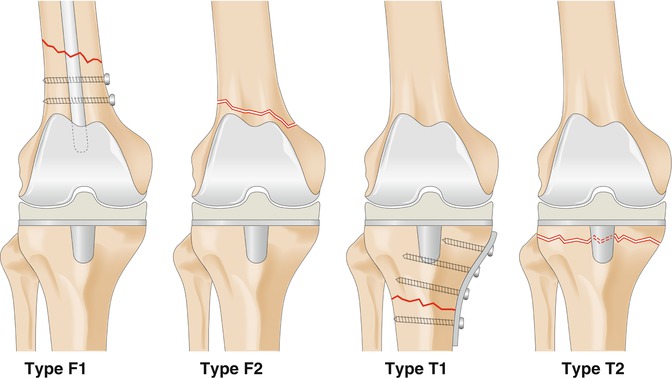
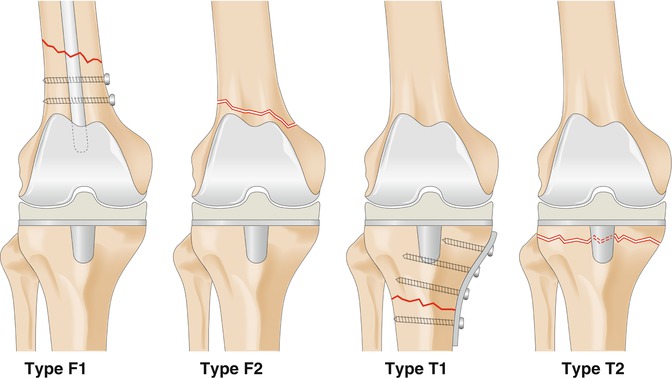
Fig. 13.2
Backstein supracondylar periprosthetic fracture classification. Femur (defined: supracondylar femur fracture within 15 cm of the femoral prosthesis). Type F1: extent of distal fracture fragment provides adequate bone for retrograde nail locking screws. Type F2: extent of distal fracture fragment does not provide adequate bone for retrograde nail locking screws. Tibia (defined: tibial fracture within 15 cm of the tibial component). Type T1: extent of proximal fracture fragment large enough to allow internal fixation. Type T2: extent of proximal fracture fragment not large enough to allow internal fixation. Additional qualification of all fractures includes the prosthesis stability and the bone stock quality, as follows: S stable prosthesis, L loose prosthesis, g good bone stock, p poor bone stock