Patient/client management comprises five elements1: The examination process involves a complex relationship between the clinician and the patient. The aims of the examination process are to provide an efficient and effective exchange and to develop a rapport between the clinician and the patient. The success of this interaction involves a myriad of factors. Successful clinicians are those who demonstrate effective communication, sound clinical reasoning, critical judgment, creative decision making, and competence. The primary responsibility of a clinician is to make decisions in the best interest of the patient. Although the approach to the examination should vary with each patient, and from condition to condition, there are several fundamental components to the examination process. The principles outlined in this chapter and integrated throughout this text, are based on the views of a number of experts,2–12 as well as principles I have learned, and used, over the years. All clinicians should commit to being lifelong students of their profession and should strive toward a process of continual self-education. Part of this process involves the utilization of the expertise of more experienced clinicians. This necessitates that the early years of practice are spent in an environment in which the novice is surrounded by a staff of varying levels of clinical and life experiences, both of which can serve as valuable resources. The clinician can also improve by investing time in reading relevant material, attending continuing education courses, completing home study courses, watching videos specializing in techniques, and observing exceptional clinicians. Exceptional clinicians are those who demonstrate excellent technical skills, combined with excellent people skills.
CHAPTER 4
Patient/Client Management
OVERVIEW
Finally, one must also never forget that the patient can serve as the most valuable resource. Each interaction with a patient is an opportunity to increase knowledge, skill, and understanding. Integral to this relationship is patient confidentiality. Except when discussing the patient’s condition with other clinicians with the object of teaching or learning, the clinician should not discuss the patient’s condition with anyone without the patient’s permission.
Much about becoming a clinician is being able to communicate with the patient, the patient’s family, and the other members of the healthcare team. The nonverbal cues are especially important because they often are performed subconsciously. Special attention needs to be paid to nonverbal communication such as voice volume, postures, gestures, and eye contact. The appearance of the clinician is also important if a professional image is to be projected.
Communication between the clinician and the patient begins when the clinician first meets the patient and continues throughout any future sessions. Communication involves interacting with the patient using terms he or she can understand, and being sensitive to cultural diversity as appropriate. The introduction to the patient should be handled in a professional yet empathetic tone. Listening with empathy involves understanding the ideas being communicated and the emotion behind the ideas. In essence, empathy is seeing another person’s viewpoint, so that a deep and true understanding of what the person is experiencing can be obtained.
At the end of the first visit and at subsequent visits, the clinician should ask if there are any questions. Each session should have closure, which may include a handshake if appropriate.
Disablement Models
Perhaps one of the most important developments in health care in the past few decades has been the increased recognition of the importance of the patient’s perception of health and functional outcomes.14 This increased recognition has shifted the focus of the physical therapy examination, evaluation, and subsequent diagnosis to the recognition of impairments and their relationship to any functional limitation or disability.
The field of physical therapy has long recognized the traditional biomedical approaches to pain have been problematic in describing patient functioning.15 This is due mainly to the fact that there is an inconsistent relationship between pain and functioning, and the fact that pain may not be the patient’s chief concern. Ideally, a disablement model is designed to detail the functional consequences and relationships of pain, disease, impairment, and functional limitations. Many disablement models have been proposed over the years, most of which are based on the Nagi original model which depicted the relationship between the following series of linked events:16,17
Pathology/Pathophysiology (the presence of disease), which may lead to impairments (anatomic and structural abnormalities), which may in turn lead to functional limitations (restrictions in basic physical and mental actions), which may then progress to disability (difficulty in doing activities of daily life). The Guide of Physical Therapist Practice18 employed terminology from the Nagi disablement model, but also described its framework as being consistent with other disablement models. Although a degree of inevitability is implied in many of the disablement models, many factors can have an impact on the pathology–disability pathway or disablement process.
In 2001 the Executive Board of the World Health Organization, in an attempt to provide a common language used by all health professions for documentation and communication, approved the International Classification of Functioning, Disability and Health (WHO-ICF). The WHO-ICF framework includes all of the following elements: the health condition, body functions/structures, activity, participation, and contextual factors, all of which are interrelated and can potentially have an impact on each other. The WHO-ICF places less emphasis on disease and greater emphasis on “components of health” rather than “consequences of disease” (i.e., participation rather than disability) and environmental and personal factors as important determinants of health. The two main components of the WHO-ICF model, which provides a method that considers biological, individual, and social contributions, are functioning and disability, and contextual factors:15,19
1. Part 1: Functioning and disability. Functioning and disability consider the relationships among the physical phenomena and within the individual that are represented by the domains of body functions and structures, activities, and participation. Part 1 is further subdivided into two components:
- Body functions and structures. Body functions and structures are assessed in terms of change in a physiological function and anatomical structure such that a deficit in body structure is associated with a deficit in functional mobility.15 For example, limited knee flexion range of motion may be associated with limitation in the ability to ascend stairs.
- Activities and participation. An activity involves the execution of a task or action (e.g., moving from sitting to standing), while participation is defined as involvement in life affairs (e.g., the ability to drive a car).
Thus, functioning is characterized by the integrity of body functions and structures, and the ability to participate in life activities.
2. Part 2: Contextual factors. Each component of functioning and disability can be broken down into standard categories referred to as contextual factors. Part 2 is also further subdivided into two components: environmental and personal contextual factors, both of which can influence functioning and disability:
- Environmental factors, including environmental barriers and facilitators to both the capacity and performance of actions and tasks in daily living. These include social attitudes, architectural characteristics, legal and social structures, as well as climate, and terrain.
- Personal factors, including age, sex, ethnic background, depression or comorbidity (e.g., pressure sores, contractures, urinary tract infections), and socioeconomic status.
Characteristics of an illness that are not amenable to modification may be termed contextual variables. Contextual factors can be viewed as secondary conditions that may influence the level of disability but are not directly related to the disease process itself.20 Broader definitions for these conditions include self-concept, work, and social participation, health-related economic consequences for the individual or family, and other family members.21,22
In addition to these two basic components, the WHO-ICF has an extensive list of descriptions, classifications, and coding for all of the functions and structures of all body systems, personal activities and participation, and environmental factors. The WHO-ICF model has been advocated in the physical therapy literature as a potential successor to the Nagi model because it explicitly acknowledges bidirectional relationships among domains of function and contextual factors, while recognizing the impact of the patient’s affective, social, and environmental factors that may be either barriers or facilitators to the physical therapy prognosis.15
The various disablement models introduced a number of terms throughout the years which are described in the following sections.
Health Condition
The original term that Nagi used, pathology, is perhaps self-explanatory. It refers to any diagnosed disease, injury, disorder, or abnormal condition that is (1) characterized by a particular cluster of signs and symptoms and (2) recognized by either the patient or clinician as abnormal.18,23,24 Although knowledge of pathology and pathophysiology can help the clinician predict the range, severity, and prognosis of a particular condition, a medical diagnosis does not tell the clinician how to manage the patient. In contrast, the term health condition better identifies the impact of a condition on function. The WHO-ICF framework refers to acute or chronic diseases, disorders, or injuries that have an impact on a person’s level of activity. While the presence of pathology may lead to distress or interference with functional status, different people with the same condition can be impacted differently. For example, consider the impact that hip osteoarthritis would have on someone who has a desk job, compared to that of a manual laborer. While pathology is primarily identified at the cellular level and is usually determined by the physician’s medical diagnosis,18,24 it does not necessarily tell the clinician the underlying etiology, or how the disease/dysfunction manifests itself as an alteration in, or attribute of, an individual’s health status. Determining the underlying etiology is important in creating an optimal management plan. It is thus important to determine whether the abnormal movement resulted from the tissue pathology, or whether the abnormal movement caused the tissue pathology.15 For example, if a patient presents with a chief concern of shoulder pain without a history of traumatic onset, the clinician must determine whether the shoulder pain was caused by an abnormal movement pattern, a muscle imbalance, a disease process, a postural dysfunction or whether the pain is being referred from elsewhere, to name but a few potential causes.
Impairment
The “Guide to Physical Therapist Practice” defines impairment as any loss or abnormality of anatomic, physiologic, mental, or psychological structure or function that both (1) results from underlying changes in the normal state, and (2) contributes to illness.18 The ICF model subdivides impairments into impairments of body function and body structure where impairments can be viewed as abnormalities of structure or function as indicated by signs and symptoms. Physical therapists typically encounter patients with impairments of body function and/or body structure of the following systems: musculoskeletal, neuromuscular, integumentary, and cardiovascular/pulmonary.
Impairments of body function and body structure have the potential to create pain and subtle alterations in the normal functions of the involved joint and surrounding tissues. Such impairments can be manifested objectively, for example, by impaired balance or coordination, reduced range of motion, articular deformity, abnormal gait, and the loss of muscle performance (strength, power, endurance), or proprioception. Impairments can also be manifested subjectively, for example, through pain, tenderness, morning stiffness, or fatigue.
Thus, impairment refers to some form of loss. Loss or loss of use refers to a change from the normal or pre-existing state. The term normal refers to a range representing healthy functioning that can vary with age, gender, and other factors such as environmental conditions. For example, the normal range of motion for knee flexion is deemed to be 150 degrees.24 Although a loss of more than 70 degrees of knee flexion may prevent a patient from performing such activities as getting in and out of a bathtub or walking up and down steps, the patient may still be able to ambulate around the house.
The ICF model describes primary, secondary, and composite impairments. Primary impairments arise directly from the health condition, whereas secondary impairments may be the result of a pre-existing impairment. A composite impairment is the result of multiple underlying causes that typically arises from a combination of primary or secondary impairments. As an example, consider a patient with low back pain. In this scenario, the patient may exhibit primary impairments of body function, such as limited range of motion of the trunk, pain, and muscle guarding during the examination. The secondary impairment may be osteoarthritis of the hip that produced a change in the patient’s gait pattern, altering the biomechanics of the lower extremity, and resulting in low back pain. A composite impairment would be a loss of balance and coordination as a result of both the low back pain and the osteoarthritis of the hip.
One of the goals of the examination process is to determine which impairments are related to the patient’s functional limitations while remembering that impairments affect people in different ways. For example, in two patients with a rotator cuff tendinitis, the impairment of one may be greater than the other due to pain. The perception of pain is highly individual, and different individuals may be impaired by pain to different degrees.
One of the goals of the examination process is to determine which impairments are related to the patient’s functional limitations—the functionally relevant impairments—and to determine whether there are any underlying causes.
Functional Limitation
A functional limitation can be defined as a restriction of the ability to perform a fundamental physical action, task, or activity in an efficient, typically expected, or competent manner.18 In other words, functional limitations are restrictions in performing expected basic physical and mental actions. Examples of such functional limitations include difficulty with walking, and an inability to put on shoes. The vast majority of the traditional tests used in physical therapy clinics, such as range of motion and strength, are measures of impairments and not function. Measurements of functional limitations include sensorimotor performance testing during such activities as walking, climbing, bending, transferring, lifting, and carrying.18 It is important that these measurements assess the patient’s ability to perform tasks that the patient feels are important. The process of identifying meaningful, achievable functional goals should be a collaborative effort between the clinician and the patient, the patient’s family, or the patient’s significant other.18 To identify functional goals, Randall and McEwen25 recommend the following steps:
- Determine the patient’s desired outcome of the intervention.
- Develop an understanding of the patient’s self-care, work, and leisure activities and the environments in which these activities occur.
- Establish goals with the patient that relate to the desired outcomes using the following questions25,26:
- If you were to concentrate your energies on one thing for yourself, what would it be?
- What activities do you need help with that you would rather perform yourself?
- What are your concerns about returning to work, home, school, or leisure activities?
- What about your current situation would you like to be different in about 6 months? What would you like to be the same?
- If you were to concentrate your energies on one thing for yourself, what would it be?
Once the goals have been agreed upon, the clinician must write the goals so that they contain the following elements:25,27
 Who (the patient)
Who (the patient)
 Will do what (activities)
Will do what (activities)
 Under what conditions (the home or work environment)
Under what conditions (the home or work environment)
 How well (the amount of assistance or number of attempts required for successful completion)
How well (the amount of assistance or number of attempts required for successful completion)
 By when (target date)
By when (target date)
Thus, the functional examination creates a functional diagnosis with functional goals. Once these functional goals are established, the clinician can grade them according to difficulty. Functional tasks can reproduce the whole task in its entirety or can break down the task into its required fundamental components and the physical demands necessary to perform each task. Regaining the smaller requirements may constitute the short-term goals whereas completion of the whole task may become the long-term goal. For example, exercises to improve sit-to-stand transfers could be initiated by having the patient perform triceps push-ups on the chair handle, perform bilateral mini-squats, or exercise on the leg press before progressing to the full functional activity.
Participation Restrictions and Disability
The term Disability was used in the Nagi disablement model. The ICF model uses the term Participation Restrictions. Both terms may be defined as having difficulty in the performance of social roles and tasks within a sociocultural and physical environment (from hygiene to hobbies, errands, to sleep), as a result of a health or physical problem.21,28,29 Both disability, and participation restrictions, describe something that may be temporary or permanent, and is the gap between what a person can do and what the person needs or wants to do. The ICF definition is not just related to any health impairment or medical condition, as it can encompass any activity limitation or participation restriction although a medical condition or impairment may cause or contribute to disability.
It is important that the clinician avoid viewing the disablement process as a unidirectional pathway with an inevitable progression to disability. Various factors, including the patient’s level of interaction with the environment, the patient’s coping skills, and the potential effects of rehabilitation, may cause a bidirectional interaction or reversal between the components of the disablement process.18,30 This bidirectional interaction may be referred to as the enabling process.30 The term health-related quality of life is often used interchangeably with the terms functional status, health status, and health outcomes. The definitions of these terms, however, might range from negatively valued aspects of life, such as death, to more positively valued aspects, such as social functioning or happiness.21,22,31–35
Clearly, the role of a physical therapist is to either reduce the impact of disability or, better still, prevent the disability from occurring whenever possible. The Guide outlines three prevention categories:1
 Primary. Prevention of disease in a susceptible or potentially susceptible population through specific measures such as general health promotion offers.
Primary. Prevention of disease in a susceptible or potentially susceptible population through specific measures such as general health promotion offers.
 Secondary. Efforts to decrease duration of illness, severity of the disease, and sequelae through early diagnosis and prompt intervention.
Secondary. Efforts to decrease duration of illness, severity of the disease, and sequelae through early diagnosis and prompt intervention.
 Tertiary. Efforts to decrease the degree of disability and promote rehabilitation and restoration of function in patients with chronic and irreversible diseases.
Tertiary. Efforts to decrease the degree of disability and promote rehabilitation and restoration of function in patients with chronic and irreversible diseases.
Early preventative measures can involve addressing modifiable risk factors. Modifiable factors are characteristics that an individual can control or adjust. The impact that the modifiable factors have on the pathology–disability pathway or disablement process can depend on both the capacities of the individual and the expectations that are imposed on the individual by those in the immediate social and occupational environment.36 Specific examples of modifiable patient factors include the following:
 The patient’s activity level. A number of studies have made associations between low physical activity levels and the onset of disability.37–48
The patient’s activity level. A number of studies have made associations between low physical activity levels and the onset of disability.37–48
 The patient’s reaction to the illness. Different cultural backgrounds are associated with different beliefs about pain, coping strategies, expressions of pain, and response to health care.49,50 The term sick role has been used to define a status accorded to the individual by himself or herself and other members of society that may be variably associated with a medical condition.36 An individual’s sick role reflects not only his or her primary condition but also any additional or secondary conditions.51,52
The patient’s reaction to the illness. Different cultural backgrounds are associated with different beliefs about pain, coping strategies, expressions of pain, and response to health care.49,50 The term sick role has been used to define a status accorded to the individual by himself or herself and other members of society that may be variably associated with a medical condition.36 An individual’s sick role reflects not only his or her primary condition but also any additional or secondary conditions.51,52
 The patient’s educational background. Patients with less formal education tend to have an increased frequency of disability.53,54
The patient’s educational background. Patients with less formal education tend to have an increased frequency of disability.53,54
 The patient’s compensatory and coping strategies. Some people simply do not have the emotional and social resources to deal with life, particularly in times of adversity.55
The patient’s compensatory and coping strategies. Some people simply do not have the emotional and social resources to deal with life, particularly in times of adversity.55
 The patient’s pain tolerance and motivation. Various studies50,56 have revealed both ethnic and gender differences in response to both clinical and experimental pain. Specifically, investigators have recently indicated that African Americans report greater levels of pain than whites for such conditions as glaucoma, acquired immunodeficiency syndrome, migraine, headache, jaw pain, postoperative pain, myofascial pain, angina pectoris, joint pain, nonspecific daily pain, and arthritis.57 Interpretations of such findings remain difficult, however, because of potential group differences in disease severity and physician management.57 There are also disparate reports about gender differences in sensitivity to pain in humans and in animals, indicating that women have a lower tolerance of pain than men.58–60 Whether women are more willing to report pain than men are, or experience pain differently than men do, is unclear. Whatever be the reasons for the differences in pain tolerance and motivation, there is perhaps a reason to suppose that improved pain tolerance and motivation might be instrumental in reducing impairment and disability. The chronic pain-adaptation model of Lund et al.61 describes a decreased activation of the muscles during movements in which they act as agonists and an increased activation during movements that require that they adopt the role of antagonists. These changes in muscle activation, characteristic of several types of chronic musculoskeletal pain, are described as a normal protective adaptation to avoid further pain and possible damage.61
The patient’s pain tolerance and motivation. Various studies50,56 have revealed both ethnic and gender differences in response to both clinical and experimental pain. Specifically, investigators have recently indicated that African Americans report greater levels of pain than whites for such conditions as glaucoma, acquired immunodeficiency syndrome, migraine, headache, jaw pain, postoperative pain, myofascial pain, angina pectoris, joint pain, nonspecific daily pain, and arthritis.57 Interpretations of such findings remain difficult, however, because of potential group differences in disease severity and physician management.57 There are also disparate reports about gender differences in sensitivity to pain in humans and in animals, indicating that women have a lower tolerance of pain than men.58–60 Whether women are more willing to report pain than men are, or experience pain differently than men do, is unclear. Whatever be the reasons for the differences in pain tolerance and motivation, there is perhaps a reason to suppose that improved pain tolerance and motivation might be instrumental in reducing impairment and disability. The chronic pain-adaptation model of Lund et al.61 describes a decreased activation of the muscles during movements in which they act as agonists and an increased activation during movements that require that they adopt the role of antagonists. These changes in muscle activation, characteristic of several types of chronic musculoskeletal pain, are described as a normal protective adaptation to avoid further pain and possible damage.61
 The patient’s personal and health habits. The link between disability and health behavior, such as excessive alcohol use, is subtle because there are many potential pathways. The link between body weight and both morbidity and mortality has been examined extensively, but relatively little research has investigated the relation between body weight and disability. Among the studies that have investigated this relation, the findings are inconsistent.62–65
The patient’s personal and health habits. The link between disability and health behavior, such as excessive alcohol use, is subtle because there are many potential pathways. The link between body weight and both morbidity and mortality has been examined extensively, but relatively little research has investigated the relation between body weight and disability. Among the studies that have investigated this relation, the findings are inconsistent.62–65
 The patient’s level of social support. The family is the primary unit of society and the one in which the earliest and most powerful social learning occurs.36 The literature on the role of the family in the development and maintenance of chronic pain and disability is extensive. Dysfunctional family systems may promote, permit, and maintain chronic pain and disability.36
The patient’s level of social support. The family is the primary unit of society and the one in which the earliest and most powerful social learning occurs.36 The literature on the role of the family in the development and maintenance of chronic pain and disability is extensive. Dysfunctional family systems may promote, permit, and maintain chronic pain and disability.36
 The patient’s marital status. Considerable research shows that the spouse’s reaction can modify the behavior of patients with chronic pain and disability.36
The patient’s marital status. Considerable research shows that the spouse’s reaction can modify the behavior of patients with chronic pain and disability.36
 The extent to which the patient is involved in litigation and compensation. Few issues around disability have given rise to more controversies than the question of litigation, compensation, and secondary gain. Anecdotal clinical and legal experience shows general agreement that some claimants magnify or exaggerate their symptoms and disability to varying degrees during the medical examination carried out specifically for legal proceedings.36
The extent to which the patient is involved in litigation and compensation. Few issues around disability have given rise to more controversies than the question of litigation, compensation, and secondary gain. Anecdotal clinical and legal experience shows general agreement that some claimants magnify or exaggerate their symptoms and disability to varying degrees during the medical examination carried out specifically for legal proceedings.36
The Examination
An examination refers to the gathering of information from the chart, other caregivers, the patient, the patient’s family, caretakers, and friends in order to identify and define the patient’s problem(s), and to design an intervention plan.18 In addition, the examination allows the clinician to confirm their pre-examination hypothesis regarding the pathology and movement dysfunction underlying the patient’s symptoms and disablement.15 In contrast, an evaluation is the level of judgment necessary to make sense of the findings in order to identify a relationship between the symptoms reported and the signs of disturbed function.18
Obtaining the necessary information to determine the clinical presentation of the patient’s symptoms, is an important initial step in the diagnostic process. The information obtained will guide the physical examination for the purpose of identifying specific impairments and functional limitations that are associated with the injury. The examination is an ongoing process that begins with the patient referral, or initial entry into the health system and continues throughout the course of rehabilitation. During the examination phase, the clinician hypothesizes the clinical problem then chooses and implements measures to test the hypotheses. The examination must be performed in a systematic manner with scientific rigor that follows a predictable and strictly ordered thought process. The purpose of the examination is to obtain information that identifies and measures a change from normal. This is determined using information related by the patient, in conjunction with clinical signs and findings. The examination should not be viewed as an algorithm. Rather, it is a framework that has specific points that can be applied to various situations. The strength of an examination relies on the accuracy of the findings of the testing procedures. Diagnostic tests are divided into two main categories:66
- Tests that result in a discrete outcome—they permit interpretations from the test as present/absent, disease/not disease, mild/moderate/severe.
- Tests that result in a continuous outcome—they provide data on an interval, or a scale of measurement, such as degrees of range of motion.
For the clinician to formulate an appropriate interpretation and an accurate final diagnosis, the tests chosen must be useful. Reliability, validity, and significance are essential in determining the usefulness of a test (see Evaluation):
 Reliability. A test is considered reliable if it produces precise, accurate, and reproducible information.67
Reliability. A test is considered reliable if it produces precise, accurate, and reproducible information.67
 Validity. Test validity is defined as the degree to which a test measures what it purports to be measuring, and how well it correctly classifies individuals with or without a particular disease condition.68–70
Validity. Test validity is defined as the degree to which a test measures what it purports to be measuring, and how well it correctly classifies individuals with or without a particular disease condition.68–70
 Significance. The term significance is used in statistics to describe the probability of something happening.
Significance. The term significance is used in statistics to describe the probability of something happening.
Patient discomfort should always be kept to a minimum. It is important that examination procedures only be performed to the point at which symptoms are provoked or begin to increase if they are not present at rest.
The examination consists of three components of equal importance: (1) patient history, (2) systems review, and (3) tests and measures.18 These three components are closely related, in that they often occur concurrently. One further element, observation, occurs throughout.
History
The history taking, specific to each joint, is detailed in each of the chapters. The history usually precedes the systems review and the tests and measures components of the examination. Whenever it occurs, it should always be used in conjunction with the findings from the system review and the tests and measures rather than performed in a vacuum. One of the purposes of the history (Table 4-1) is to collect enough clinical data to establish a diagnostic hypothesis that will focus the examination in terms of a complete differential diagnosis at the level of pathology, determining any potential underlying etiology, and prioritizing the tests and measures to be used, especially if the clinician has a good understanding of the underlying anatomy and biomechanics. There has been a recent trend to put less emphasis on the history and use the results from imaging studies to determine a clinical diagnosis, which is ironic given the fact that much of these diagnostic tests would be unnecessary if more attention was paid to the clinical examination.72 Indeed, multiple studies have demonstrated the incidence of MRI abnormalities in the spine,73 the shoulder,74 the knee,75 and other areas in normal subjects. Obviously, an improper diagnosis leads to inappropriate treatment.
TABLE 4-1 | Data Generated from a Patient History |
General demographics | Includes information about the patient’s age, height, weight, and marital status and primary language spoken by the patient.a |
Social history and social habits | Includes information about the patient’s social history, including support systems, family and caregiver resources, and cultural beliefs and behaviors.1 An individual’s response to pain and dysfunction is, in large part, determined by his or her cultural background, social standing, educational and economical status, and anticipation of functional compromise.b |
Occupation/employment | Includes information about the patient’s occupation, employment, and work environment, including current and previous community and work activities.1 The clinician must determine the patient’s work demands, the activities involved, and the activities or postures that appear to be aggravating the condition or determine the functional demands of a specific vocational or avocational activity to which the patient is planning to return. Work-related low back injuries and repetitive motion disorders of the upper extremities are common in patients whose workplaces involve physical labor. Habitual postures may be the source of the problem in those with sedentary occupations. Patients who have sedentary occupations may also be at increased risk of overuse injuries when they are not at work, as a result of recreational pursuits (the weekend warrior). |
Growth and development | Includes information about the patient’s developmental background and hand or foot dominance. Developmental or congenital disorders that the clinician should note include such conditions as Legg–Calvé–Perthes disease, cerebral palsy, Down syndrome, spina bifida, scoliosis, and congenital hip dysplasia. |
Living environment | The clinician should be aware of the living situation of the patient, including entrances and exits to the house, the number of stairs, and the location of bathrooms within the house. |
Functional status and activity level | Includes information about the patient’s current and prior level of function, with particular reference to the type of activities performed and the percentage of time spent performing those activities. |
Past history of current condition | It is important for the clinician to determine whether the patient has had successive onsets of similar symptoms in the past, because recurrent injury tends to have a detrimental effect on the potential for recovery. If the patient’s history indicates a recurrent injury, the clinician should note how often, and how easily, the injury has recurred and the success or failure of previous interventions. |
Past medical/surgical history | Includes information with regard to allergies, childhood illnesses, and previous trauma. In addition, information on any health conditions, such as cardiac problems, high blood pressure, or diabetes, should be elicited, as these may impact exercise tolerance (cardiac problems and high blood pressure) and speed of healing (diabetes). If the surgical history is related to the current problem, the clinician should obtain as much detail about the surgery as possible from the surgical report, including any complications, precautions, or postsurgical protocols. Although this information is not always related to the presenting condition, it does afford the clinician some insight as to the potential impact or response the planned intervention may have on the patient. |
Family history and general health status | Certain diseases, such as rheumatoid arthritis, diabetes, cardiovascular disease, and cancer, have familial tendencies. The general health status refers to a review of the patient’s health perception, physical and psychological function, as well as any specific questions related to a particular body region, or complaint.1 |
aGuide to physical therapist practice. Phys Ther. 2001:81;513–595. bJudge RD, Zuidema GD, Fitzgerald FT. The medical history and physical. In: Judge RD, Zuidema GD, Fitzgerald FT, eds, Clinical Diagnosis. 4th ed. Boston, MA: Little, Brown and Company;1982:9–19. | |
The other purpose of the subjective examination is to develop a working relationship with the patient and to establish lines of communication with the patient. Ideally, the interview of a patient should be conducted in a quiet, well-lit room that offers a measure of privacy. To encourage good communication, the clinician and the patient should be at a similar eye level, facing each other, with a comfortable space between them (approximately 3 ft). The clinician must record the history in a systematic fashion so that every question has a purpose, and no subject areas are neglected. Formal questioning using a questionnaire (Table 4-2) helps to ensure that all of the important questions are asked. A body chart (Fig. 4-1) can be used to ascertain the specific location and the nature of the symptoms. Discussing the information provided on the medical history form with the patient helps to establish a rapport with the patient. Knowing the importance of each question is based on the didactic background of the clinician, as is the ability to convert the patient’s responses into a working hypothesis. For example, if the patient reports that lumbar flexion relieves their low back pain, but that lumbar extension aggravates it, the clinician needs to know which structures are stressed in lumbar extension, but unstressed in lumbar flexion.
TABLE 4-2 | Sample Medical History Questionnaire |
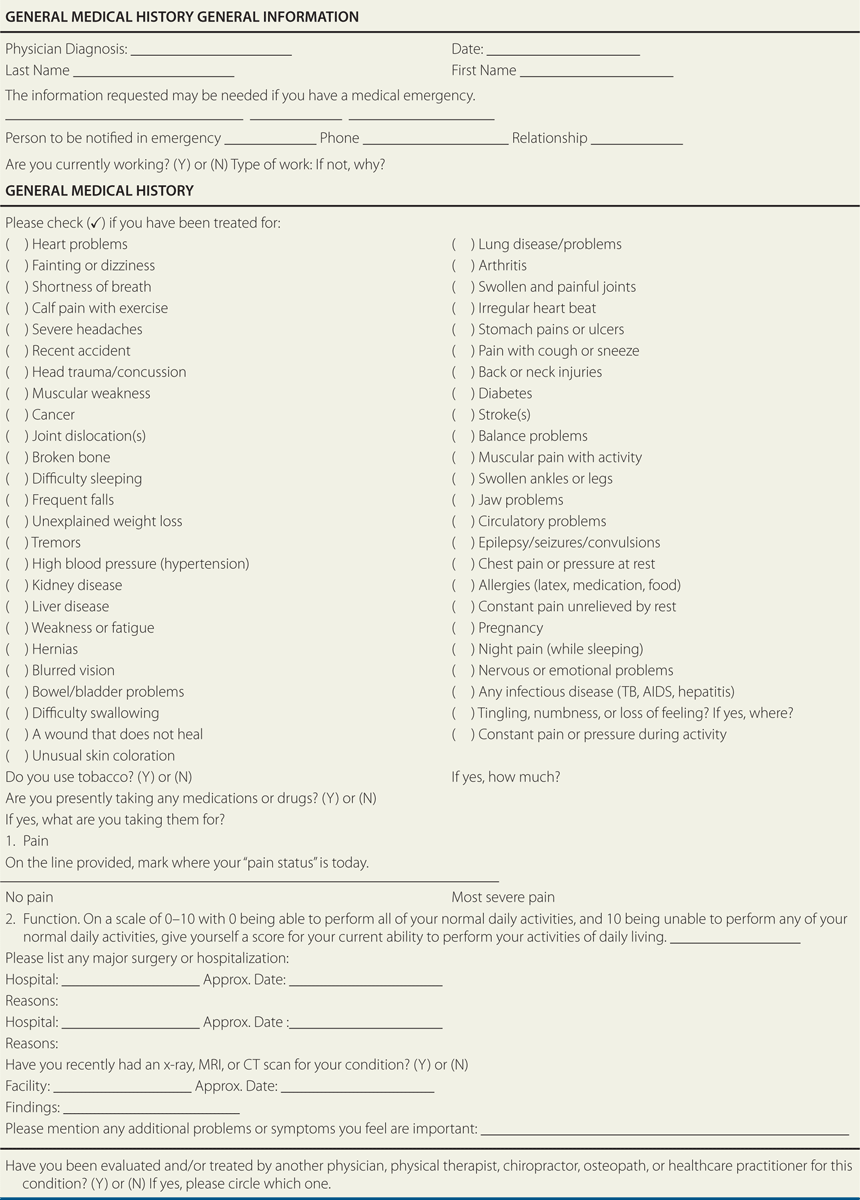
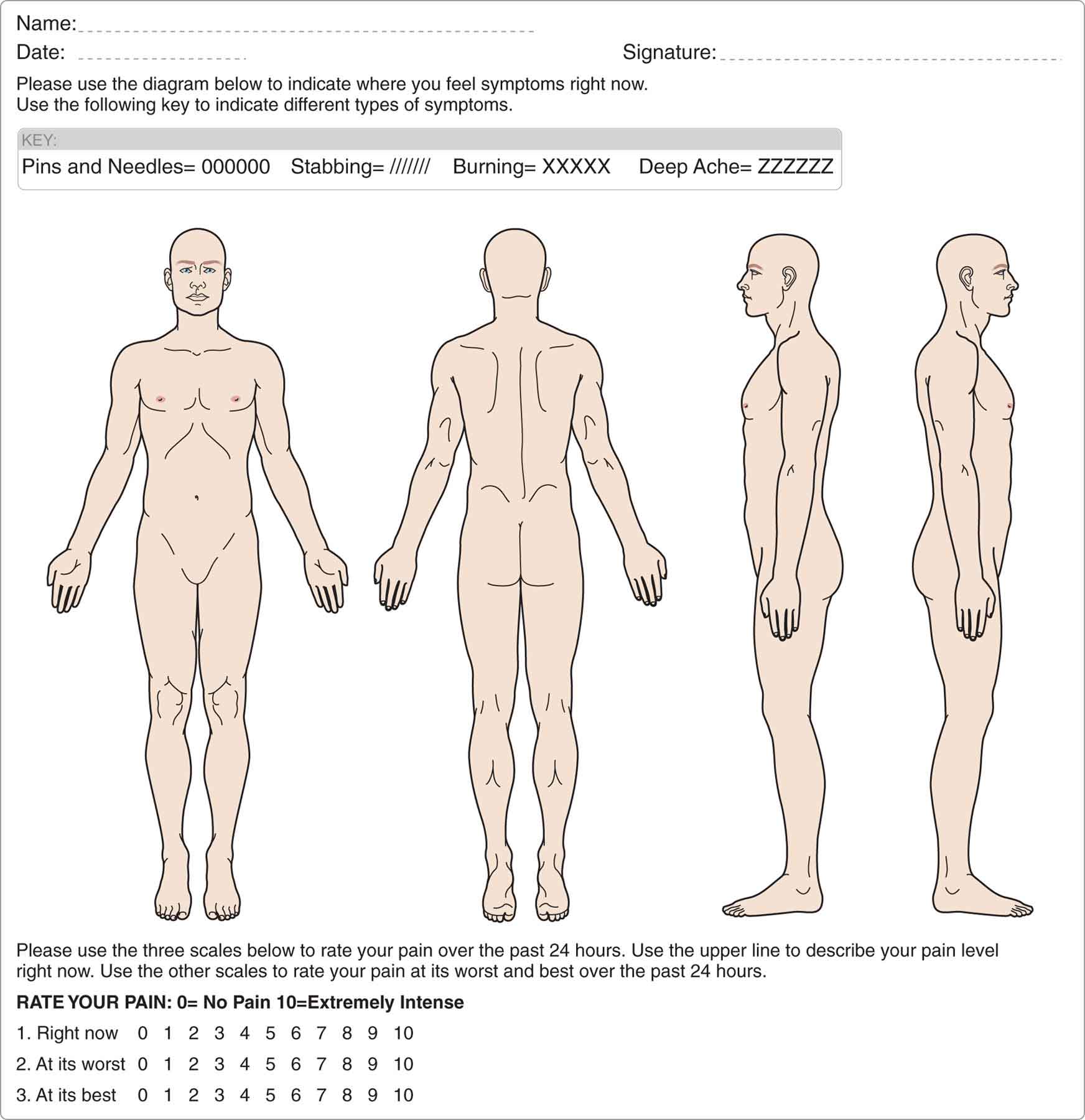
FIGURE 4-1 Body chart.
A transfer of accurate information must occur between the patient and the clinician. The method of questioning should be altered from patient to patient, as the level of understanding and answering abilities varies between each individual. In general, the interview should flow as an active conversation, not a question-and-answer session. A successful learning process requires the clinician to have patience, focus, and self-criticism.6
Open-ended questions or statements, such as “Tell me why you are here today,” are used initially to encourage the patient to provide narrative information, help determine the patient’s chief complaint, and to decrease the opportunity for bias on the part of the clinician.77 More specific questions, such as “How did this pain begin?” are asked as the examination proceeds (Table 4-3). The specific questions help to focus the examination and deter irrelevant information. The clinician should provide the patient with encouraging responses, such as a nod of the head, when the information is relevant and when needed to steer the patient into supplying the necessary information. Neutral questions should be used whenever possible. These questions are structured in such a way so as to avoid leading the patient into giving a particular response. Leading questions, such as “Does it hurt more when you walk?” should be avoided. A more neutral question would be, “What activities make your symptoms worse”?
TABLE 4-3 | Contents of the History |
History of Current Condition
Did the condition begin insidiously or was trauma involved?
How long has the patient had the symptoms?
Where are the symptoms?
How does the patient describe the symptoms?
Reports about numbness and tingling suggest neurologic compromise. Reports of pain suggest a chemical or mechanical irritant. Pain needs to be carefully evaluated in terms of its site, distribution, quality, onset, frequency, nocturnal occurrence, aggravating factors, and relieving factors.
Past History of Current Condition
Has the patient had a similar injury in the past?
Was it treated or did it resolve on its own? If it was treated, how was it treated and did intervention help?
How long did the most recent episode last?
Past Medical/Surgery History
How is the patient’s general health?
Does the patient have any allergies?
Medications Patient is Presently Taking
Other Tests and Measures
Has the patient had any imaging tests such as x-ray, MRI, CT scan, bone scan?
Has the patient had an EMG test, or a nerve conduction velocity test, which would suggest compromise to muscle tissue and/or neurologic system?
Social Habits (Past and Present)
Does the patient smoke? If so, how many packs per day?
Does the patient drink alcohol? If so, how often and how much?
Is the patient active or sedentary?
Social History
Is the patient married, living with a partner, single, divorced, or widowed?
Is the patient a parent or single parent?
Family History
Is there a family history of the present condition?
Growth and Development
Is the patient right- or left-handed?
Were there any congenital problems?
Living Environment
What type of home does the patient live in with reference to accessibility?
Is there any support at home?
Does the patient use any extra pillows or special chairs to sleep?
Occupation/Employment/School
What does the patient do for work?
How long has he or she worked there?
What does the job entail in terms of physical requirements?
What level of education did the patient achieve?
Functional Status/Activity Level
How does the present condition affect the patient’s ability to perform activities of daily living?
How does the present condition affect the patient at work?
How does the patient’s condition affect sleep?
Is the patient able to drive? If so, for how long?
CT, computed tomography; EMG, electromyogram; MRI, magnetic resonance imaging.
Data from Clarnette RG, Miniaci A. Clinical exam of the shoulder. Med Sci Sports Exerc. 1998:30;1–6.
In addition to the details listed in Table 4-3, the history can help the clinician to:
 determine the chief complaint, its mechanism of injury, its severity, and its impact on the patient’s function. It is worth remembering that a patient’s chief complaint can sometimes differ from the chief concern, but both should be addressed.
determine the chief complaint, its mechanism of injury, its severity, and its impact on the patient’s function. It is worth remembering that a patient’s chief complaint can sometimes differ from the chief concern, but both should be addressed.
 determine the irritability of the symptoms. Irritability is the amount of activity necessary to cause symptom worsening or improvement.15
determine the irritability of the symptoms. Irritability is the amount of activity necessary to cause symptom worsening or improvement.15
 establish a baseline of measurements.
establish a baseline of measurements.
 ascertain which medications the patient is currently taking and whether they are prescribed or over the counter (see Chapter 9).
ascertain which medications the patient is currently taking and whether they are prescribed or over the counter (see Chapter 9).
 elicit information about the past history of the current condition.
elicit information about the past history of the current condition.
 determine the goals and the expectations of the patient from the physical therapy intervention. It is important that the clinician and the patient discuss and determine mutually agreed upon anticipated goals and expected outcomes. The discussion can help the clinician determine whether the patient has realistic expectations or will need further patient education concerning his or her condition and typical recovery time frames.
determine the goals and the expectations of the patient from the physical therapy intervention. It is important that the clinician and the patient discuss and determine mutually agreed upon anticipated goals and expected outcomes. The discussion can help the clinician determine whether the patient has realistic expectations or will need further patient education concerning his or her condition and typical recovery time frames.
 elicit reports of potentially life-threatening symptoms, or red flags, that require an immediate medical referral (see Chapter 5). Examples include reports of pain made worse by rest but better with activity, fever or chills, and a sudden or insidious onset of symptoms.
elicit reports of potentially life-threatening symptoms, or red flags, that require an immediate medical referral (see Chapter 5). Examples include reports of pain made worse by rest but better with activity, fever or chills, and a sudden or insidious onset of symptoms.
There are key questions in every subjective examination of inquiries regarding:78
 the patient’s age, general health, and medications;
the patient’s age, general health, and medications;
 the mode of onset of symptoms;
the mode of onset of symptoms;
 the location and behavior of symptoms, such as aggravating and relieving factors;
the location and behavior of symptoms, such as aggravating and relieving factors;
 the results of any imaging studies;
the results of any imaging studies;
 the impact of the patient’s pain/symptoms on sleeping;
the impact of the patient’s pain/symptoms on sleeping;
 the patient’s current occupation/leisure/sports activities and desired levels of activities and goals; and
the patient’s current occupation/leisure/sports activities and desired levels of activities and goals; and
 the patient’s thoughts, beliefs, and feelings around their problem.
the patient’s thoughts, beliefs, and feelings around their problem.
Age, Ethnicity, Gender, Morphology, and Family History
Certain conditions are related to age, ethnicity, gender, morphology, and family history. For example,
 Degenerative and overuse syndromes are more frequent in the over 40 age group.
Degenerative and overuse syndromes are more frequent in the over 40 age group.
 Cervical spondylosis is often seen in persons 25 years of age or older, and it is present in 60% of those older than 45 years and 85% of those older than 65 years of age.79–81
Cervical spondylosis is often seen in persons 25 years of age or older, and it is present in 60% of those older than 45 years and 85% of those older than 65 years of age.79–81
 The onset of ankylosing spondylitis often occurs between the ages of 15 and 35 years.82
The onset of ankylosing spondylitis often occurs between the ages of 15 and 35 years.82
 Both osteoporosis and osteoarthritis are more often associated with the older population.
Both osteoporosis and osteoarthritis are more often associated with the older population.
 Diseases such as Legg–Perthes disease or Scheuermann’s are seen in adolescents or teenagers.
Diseases such as Legg–Perthes disease or Scheuermann’s are seen in adolescents or teenagers.
 Prostate cancer has a higher incidence in men older than 50 years of age.83
Prostate cancer has a higher incidence in men older than 50 years of age.83
 Among African Americans in the United States, 1 in 600 has sickle cell anemia.84
Among African Americans in the United States, 1 in 600 has sickle cell anemia.84
 Caucasians experience higher osteoporotic fracture rates than either Asians or African Americans.85
Caucasians experience higher osteoporotic fracture rates than either Asians or African Americans.85
 Some diseases, such as hypertension and renal disease, are more prevalent in African-American populations than among Caucasians.86,87
Some diseases, such as hypertension and renal disease, are more prevalent in African-American populations than among Caucasians.86,87
 Basal cell carcinoma and melanoma are more common among Caucasians.
Basal cell carcinoma and melanoma are more common among Caucasians.
 The male-to-female ratio of bladder cancer is 2:1 to 4:1 and the disease is twice as common in male Caucasians as in African-American men in the United States.88,89
The male-to-female ratio of bladder cancer is 2:1 to 4:1 and the disease is twice as common in male Caucasians as in African-American men in the United States.88,89
 Breast cancer is the most frequently diagnosed cancer and the second leading cause of cancer-related deaths among women in the United States.90
Breast cancer is the most frequently diagnosed cancer and the second leading cause of cancer-related deaths among women in the United States.90
 Melanoma is the leading cause of cancer death in women aged 25–36 years.91
Melanoma is the leading cause of cancer death in women aged 25–36 years.91
 Anterior knee pain caused by patellofemoral syndrome is most common in young teenage girls and young men in their 20s.92
Anterior knee pain caused by patellofemoral syndrome is most common in young teenage girls and young men in their 20s.92
 Obesity has been linked to many diseases such as diabetes, cardiovascular disease, and degenerative joint disease.
Obesity has been linked to many diseases such as diabetes, cardiovascular disease, and degenerative joint disease.
 Many diseases can be linked to family history, including diabetes, cardiovascular disease, and Charcot Marie Tooth disease.
Many diseases can be linked to family history, including diabetes, cardiovascular disease, and Charcot Marie Tooth disease.
Mode of Onset of Current Condition
This portion of the history-taking can prove to be the most challenging as it involves the gathering of both positive and negative findings, followed by the dissemination of the information into a working hypothesis. An understanding of the patient’s history of the current condition can often help determine the prognosis and guide the intervention.
The clinician should determine the circumstances and manner in which the symptoms began and the progression of those symptoms.6 The onset and duration (stage) of symptoms provide clinicians with information as to whether the injury is acute or chronic. This information is very important in that the mechanisms of a certain injury may be similar; however, the time associated with symptom presentation may differ significantly.93 For example, an acute muscle strain injury that occurs during a sport will present with immediate pain and an easily identifiable mechanism. Conversely, a muscle strain injury that occurs through an overuse mechanism may present insidiously.93 Establishing a symptom timeline can help the clinician collect information about the duration of symptoms.94 The symptom timeline is a brief description that lists any significant event during the course of the patient’s symptoms such as the number of times that the symptoms improved, the number of times that the symptoms worsen, any interventions that were tried, and any visits to healthcare providers that occurred.15
The mode of onset, or the mechanism of injury, is usually either a major traumatic event over a short period of time, such as a fall or motor vehicle accident (macrotraumatic), or a series of minor traumatic events over a prolonged period of time, such as the habitual use of a lifting/sitting/training technique (microtraumatic) either of which can give clues as to the extent and nature of the damage caused. However, it is important to remember that the patient’s description of injury mechanism should be interpreted with caution because the mechanism ascribed to the onset of symptoms could be falsely assumed, causing the clinician to overlook the presence of an another pathology.15
If the injury is traumatic, the clinician should determine the time of onset, and the specific mechanism in terms of both the direction and the force, and relate the time and mechanism to the presenting symptoms. If the injury is recent, an inflammatory source of pain is likely. A sudden onset of pain, associated with trauma, could indicate the presence of an acute injury such as a soft tissue tear or even a fracture, whereas immediate pain and locking are most likely to result from an intraarticular block. Joint locking and twinges of pain may indicate a loose body is moving within the joint. Reports of a joint “giving way” usually indicate joint instability, or a reflex inhibition or weakness of muscles. An injury that is not recent but which the symptoms have persisted could indicate a biomechanical dysfunction. Often-times a particular motion or posture may continue to aggravate the condition.
If the onset is gradual or insidious, the clinician must determine if there are any predisposing factors, such as changes in the patient’s daily routines or exercise programs. Symptoms of pain, or limitations of movement, with no apparent reason, are usually a result of inflammation, early degeneration, repetitive activity (microtrauma), or sustained positioning and postures.95 However, such symptoms may also be associated with something more serious, such as a vascular insufficiency, a tumor, or an infection.
If pain is present, the clinician’s major focus should be to seek the cause and methods to control it. Pain may be constant, variable, or intermittent.
 Variable pain is pain that is perpetual, but that varies in intensity. Variable pain usually indicates the involvement of both a chemical and a mechanical source. The mechanical cause of constant pain is less understood but is thought to be the result of the deformation of collagen, which compresses or stretches the nociceptive-free nerve endings, with the excessive forces being perceived as pain.96 Thus, specific movements or positions should influence pain of a mechanical nature.
Variable pain is pain that is perpetual, but that varies in intensity. Variable pain usually indicates the involvement of both a chemical and a mechanical source. The mechanical cause of constant pain is less understood but is thought to be the result of the deformation of collagen, which compresses or stretches the nociceptive-free nerve endings, with the excessive forces being perceived as pain.96 Thus, specific movements or positions should influence pain of a mechanical nature.
 Chemical, or inflammatory, pain is more constant and is less affected by movements or positions than mechanical pain.
Chemical, or inflammatory, pain is more constant and is less affected by movements or positions than mechanical pain.
 Intermittent pain is unlikely to be caused by a chemical irritant. Usually, this type of pain is caused by prolonged postures, a loose intraarticular body, or an impingement of a musculoskeletal structure.
Intermittent pain is unlikely to be caused by a chemical irritant. Usually, this type of pain is caused by prolonged postures, a loose intraarticular body, or an impingement of a musculoskeletal structure.
Unfortunately, the source of the pain is not always easy to identify, because most patients present with both mechanical and chemical pain.
Finally, the clinician should determine if this is the first episode requiring treatment, or if a specific intervention has been used in the past for the same condition and, if so, the clinician should ask about the effectiveness of that intervention. If it is a repeat episode, the clinician should ascertain how long it took to recover from the previous one, and what therapy was beneficial if any.
Location
The clinician should determine the location of the symptoms because this can indicate which areas need to be included in the physical examination. However, it must be remembered that the location of symptoms for many musculoskeletal conditions is quite separate from the source, especially in those peripheral joints that are more proximal, such as the shoulder and the hip. For example, a cervical dysfunction can produce symptoms throughout the upper extremity. The term referred is used to describe symptoms that have their origin at a site other than where the patient feels the symptoms (see Chapter 3). For example, pain due to osteoarthritis of the hip is often felt in the anterior groin and thigh. The term radicular is used to describe the distribution of symptoms associated with nerve root compression, in which the symptoms radiate from the source. For example, a patient who has a compressed spinal nerve in the cervical spine may feel the symptoms in the neck and throughout certain areas in the upper extremity. The concepts of referred and radicular symptoms are often difficult for a patient to understand, so it is important that the clinician provide an explanation so that the patient has a better understanding and can answer questions about symptoms they might otherwise have felt irrelevant.
Information about how the location of the symptoms has changed since the onset can indicate whether a condition is worsening or improving. In general, as a condition worsens, the pain distribution becomes more widespread and distal (peripheralized). As the condition improves, the symptoms tend to become more localized (centralized). A body chart may be used to record the location of symptoms (see Fig. 4-1).
