CHAPTER 19 Patient Education and Support
This chapter was designed with the purpose of providing insight into the role of the medical staff in patient education and assessment, both prior to and after spinal injection procedures. This chapter will also discuss the importance of appropriate and effective communication in carrying out the algorithmic approach to patient care that was initially formulated. Education and assessment are a continuous process that begins with the initial consultation and continues throughout the patient’s course of care.
NEW PATIENT VISIT
At the initial consultation and evaluation, a thorough, detailed history and physical examination is conducted. This information, in addition to the findings of other pertinent diagnostic studies such as radiographic and neurophysiologic data (i.e. magnetic resonance imaging and electrodiagnostic studies) is incorporated into formulating a comprehensive plan of care. Once spinal injections are integrated into the course of care, there are several ways in which education is provided. First, the physician explains the algorithmic approach to spinal injections which may include selective nerve root, facet joint, piriformis, hip, and sacroiliac joint injections of a diagnostic or therapeutic nature. The physician obtains informed consent, and discusses in detail the nature and purpose of the procedure, as well as the potential side effects, risks, and complications of the specific spinal injections being considered.1–4
In order to provide a better understanding of what may be expected the day of the procedure, a spinal injection guide is handed out at the initial visit. Information found inside this guide includes definitions of relevant terms, medications administered, and expectations prior and subsequent to the procedure, as well as an explanation of possible complications. Since oftentimes one may forget that these important details surrounding the injection procedure were discussed, the authors ask that a patient information form be signed (Fig. 19.1). The form simply states that they have received an information booklet, and that the logistics of the procedure have been discussed.
PREPROCEDURE
Prior to any procedure, informed consent must be obtained. The importance of properly obtaining informed consent cannot be overemphasized. The components of informed consent include discussion of the nature, purpose, and potential benefits of a procedure, as well as potential side effects, risks and complications.1–4 These issues are discussed in fine detail at the initial consultation, and at many other times during the course of care.
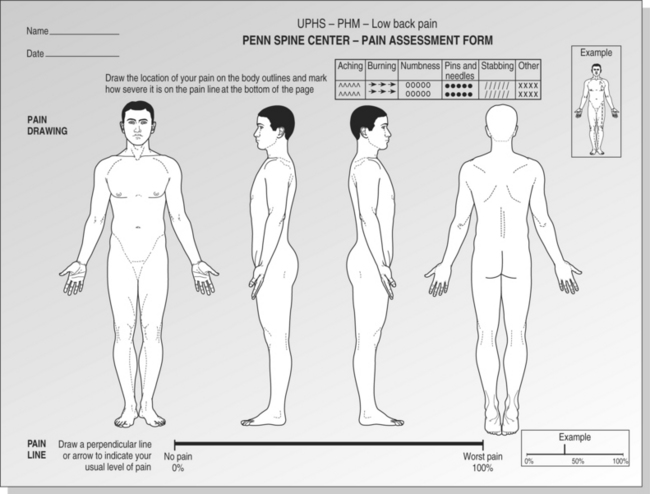
In addition to obtaining written informed consent prior to the injection procedure, a pain assessment drawing must be completed. (Fig. 19.2)
According to the National Institutes for Health (NIH), patient self-reporting is the ‘most reliable indicator of the existence and intensity of pain.’5 The pain drawing is completed according to the patient’s discomfort pattern at the specific moment in time just prior to the procedure, as opposed to where the discomfort was at the initial visit, or where it is on average. A pain drawing is to be completed at every encounter, including injection procedures. The location and character of the pain complaint (e.g. numbness, stabbing, burning) as well as the intensity of pain on the 11-point visual analog scale (VAS) is to be documented. By illustrating the discomfort present at the specific encounter, a visually recorded diary of symptom progression is created. If the case is one of successful pain mitigation, or failure to progress, it will be illustrated upon review of the pain drawings. Studies have shown that there is an ‘amnestic property of pain.’ This means that one may not remember the level of pain which was previously experienced. This is true especially if the current pain is severe.6
The VAS was introduced in the early part of the last century as a psychologic assessment tool for the measurement of pain and mood. The popularity of the VAS stems from its simple construction and ease of use.7 It is best used in the sequential evaluation of pain; the broad range of scores allows for subsequent statistical analysis. The VAS ranges from 0 to 10 (or 100), and is most often measured on a 10 cm horizontal line.8,9 The VAS is a unidimensional assessment tool based on self-report and is the most commonly used and validated scale to assess pain.10–12 The ideal tool in the assessment of pain should include the identification of the presence of pain, as well as the progress of pain with time or treatment.10,13 Studies have shown that outside observers are often inaccurate in their assessment of a patient’s pain on an individual basis; thus, pain drawings and VAS ratings are of utmost importance.14,15 Incidentally, a study by Todd and Funk correlated a change of 1.8 cm on a scale of 10 cm in the physician’s assessment of the patient as the patient’s feeling ‘a little bit better.’16 In another recent study, Farrar et al. showed that widely different patient populations interpret changes in VAS similarly.17
In some instances, even after a thorough explanation of the algorithmic approach at the initial consultation, some questions may still remain regarding the ‘next step’ in the process. For example, if a patient had a positive diagnostic selective nerve root block, usually a therapeutic selective nerve root injection is scheduled to follow. In this case, it would be explained that steroids are to be administered along with either 2% or 1% lidocaine. In addition, it is important to present an estimated duration for the procedure. If, on the other hand, a diagnostic injection were to be performed, in order to ensure that the usual symptoms were present, ‘yes’ or ‘no’ would need to be checked on a form that states ‘Are you experiencing your usual pain right now?’ (Fig. 19.3).
The words ‘right now’ are the key words in this particular situation. In order to receive the necessary information that a diagnostic injection may provide, the usual symptoms must be present preprocedure. This is because the diagnostic test injection determines the plan of care based upon symptom presence right before the diagnostic injection and symptom attenuation or persistence approximately 20–30 minutes afterwards. It is important to note that diagnostic injections are not performed for numbness alone, and that there must be a significant ‘pain’ component. While these concepts may seem intuitive to the reader they are not so obvious to the patient. The authors have encountered numerous instances in which highly educated individuals, who had received a detailed explanation of the purpose and method of interpretation of diagnostic injections, presented for a diagnostic injection despite the complete absence of pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree