Chapter 91 Patellar Instability
Patellofemoral instability is a common cause of subjective complaints and activity impairment in the pediatric population. Conditions may vary from fixed, in utero dislocations to macrotraumatic injuries in previously asymptomatic, scholastic athletes. As discrepant as these scenarios may seem, they have in common a “relative” imbalance of the extensor mechanism of the knee. Effective evaluation and treatment of patellofemoral instability is based on an understanding of the “normal envelope”29 of extensor mechanism function and the multitude of factors that may disrupt its complex activity.
Embryology
The appendicular skeleton appears very early in embryologic development. By the fourth week of gestation, the limb buds are easily identifiable, with maturation of the lower extremities trailing the upper ones by several days. The leg buds begin to bend anteriorly at the developing knee during the fifth week. By week 7, the distal end of the femur and the patella have undergone chondrification, and the patellofemoral articulation is recognizable in its adult form. Initially, the lower limbs extend from the torso with the soles of the feet facing medially, toward one another. By the eighth week of gestation, the lower limbs complete a 90-degree, internal rotation, which brings them into their adult orientation.32,67,84,94 It is thought that failure of the quadriceps myotome to complete this internal rotation is the most probable cause of in utero, congenital patellofemoral dislocation.40,41,98 Failure of rotation leaves the extensor mechanism in a contracted, laterally dislocated position relative to the distal end of the femur.
Initial formation or malformation of the patellofemoral joint and other knee structures appears to be genetically driven without dependence on function.32,50 However, abnormal motion and stress across the articulation appear to play a role in progressive, developmental dysplasia. Individual abnormalities such as a shallow femoral sulcus, patellar hypoplasia, and patella alta tend to appear in relative amounts within a constellation of dysplastic changes. In cases of congenital, developmental, and habitual dislocation, early surgical restoration toward more normal extensor mechanism biomechanics may lead to partial normalization of patellofemoral architecture.38,41,52
Anatomy and Biomechanics
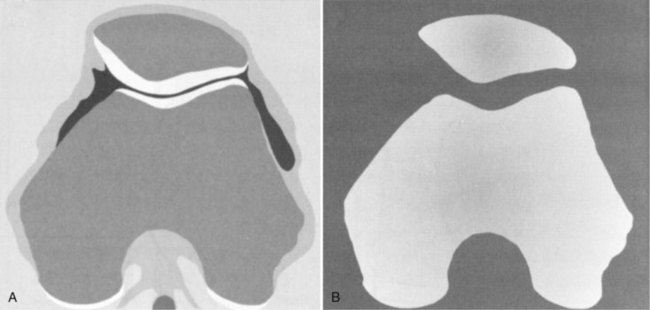
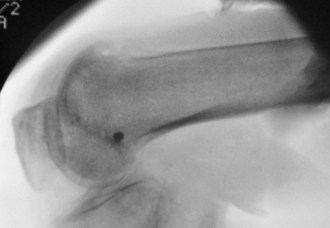
The patella lies within the trochlea of the femur, bounded by the medial and lateral femoral condyles. Cartilaginous at birth, the patella begins ossification from multiple centers during early childhood. The relatively cartilaginous composition of the immature patella has diagnostic and clinical implications. Apparent lack of patellofemoral congruity and excessive shallowness of the femoral sulcus in the child’s knee are in large part an illusion (Fig. 91-1). Nietosvaara71 has shown that although the osseous patellofemoral sulcus angle is inversely proportional to age, ultrasound measurements of the cartilaginous sulcus are nearly constant throughout growth. Gradual thinning of the articular cartilage from the outer areas of the sulcus and retropatellar facets leads to apparent deepening of the sulcus with age.77 Even in a mature knee, a significant mismatch is seen between the osseous outlines of the patellofemoral articulation and the geometry of the true articular cartilage surfaces (Fig. 91-2).97 For these reasons, congenital and acquired patellofemoral dysplasia may be better represented on magnetic resonance imaging (MRI) than on plain radiographs.
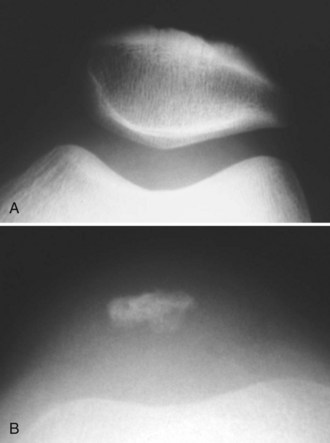
Figure 91-1 Sunrise view of the patellofemoral joint in an adult man (A) and an 8-year-old boy (B).
(From Hinton RY, Sharma KM: Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am 34:285–396, 2003.)
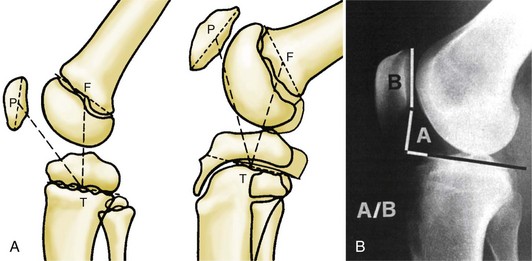
Patellar height is an important factor to consider during the evaluation of patellofemoral disorders. Patella alta is one of the best substantiated radiographic risk factors for patellar instability.* However, reliable measurement of this condition is limited by the cartilaginous nature of the patella and the tibial tubercle in the younger knee.102 Alternatives to the traditional Insall-Salvati method aim to minimize these effects (Fig. 91-3). Koshino and Sugimoto’s method51 uses relationships of the midpatella to the midepiphyseal lines of the tibia and femur. This scheme may be most appropriate for younger children. The Blackburne-Peel12 modification uses the relationship between posterior facet length and the distance to the tibial articular surface. This method is helpful in adolescents, in whom the inferior pole of the patella is not fully ossified, or who have secondary tibial tubercle changes associated with Osgood-Schlatter disease.
The tibial tubercle also undergoes gradual ossification during childhood. Genu recurvatum is a potential complication with tubercle osteotomies and distal extensor realignment procedures. The appropriate age cutoff is not well described. However, older case series45,57 report such complications in patients younger than but not older than 14.
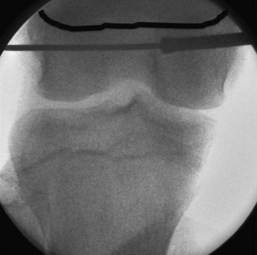
The femoral origin of the medial patellofemoral ligament (MPFL) is just distal to the femoral physis. The femoral physis is cup shaped at its periphery, and the MPFL attachment on the medial epiphyseal bone is actually superior to the more central physeal plate. This must be taken into consideration when drilling tunnels or using various fixation devices for the femoral side of MPFL reconstructions. These must be angled downward and parallel to the physis, not perpendicular and inadvertently into the physeal plate. As will be discussed in later text, erring slightly more distal in the femoral insertion of an MPFL reconstruction has fewer adverse consequences for the biomechanics of the graft within its functional range of full extension to 40 degrees of flexion. This distal “malposition” can help to protect the physis (Fig. 91-4).
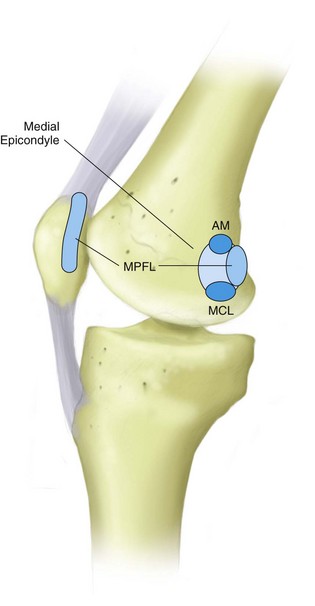
The multilayer soft tissue envelope about the patellofemoral joint has been described as having three layers on both medial and lateral sides.25,95,96,103 Medially, the superficial layer is the investing fascia over the sartorius muscle. The second layer includes the MPFL, the parapatellar retinaculum, and the superficial medial collateral ligament (MCL). The third medial layer contains the deep MCL and joint capsule. This arrangement places the MPFL in the same extracapsular environment as the MCL (Fig. 91-5). Such an environment is one that may promote ligamentous healing, as seen by the ability of the MCL to regain function and structure even after major injury. Laterally, fascial interconnections are seen between the fibers of the iliotibial band, lateral hamstrings, lateral patellofemoral ligaments, and lateral quadriceps retinaculum that feed into the lateral aspect of the patella. Tightness in these structures may cause excessive posterior and lateral pull, thereby contributing to lateral patellar tilt and increased retropatellar pressure.
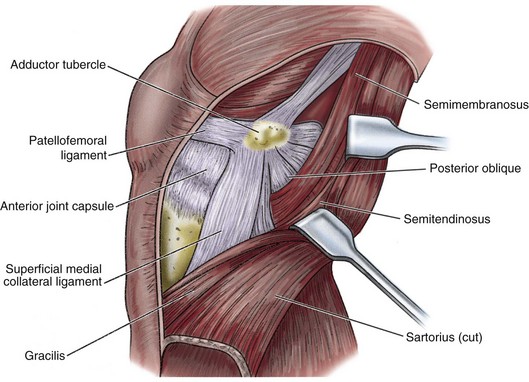
Figure 91-5 Diagram of layer II medial-side knee structures.
(From Clarke HD, Scott WN, Insall JN, et al: Anatomy. In Insall JN, Scott WN [eds]: Surgery of the knee, Philadelphia, 2001, WB Saunders, p 52.)
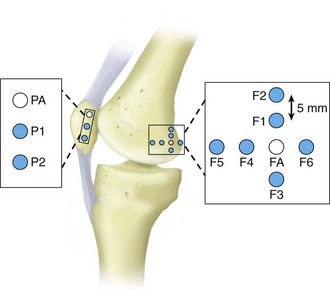
The MPFL is an hourglass-shaped, ligamentous structure that runs transversely from the posterior part of the medial epicondyle, approximately 1 cm distal to the adductor tubercle, to the superomedial part of the patella. Although present as a distinct structure in 90% of specimens, this ligament can vary greatly in size and strength.14,25,46 The femoral origin is intimately associated with insertions of the adductor tendon and the superficial MCL (Fig. 91-6). The MPFL originates in the saddle area distal to the adductor tubercle, just superior to the MCL origin and posterior to both.76,80,95 Radiographically, on a true lateral, the center of femoral origin is 1 mm anterior to an extension line from the posterior cortex, 2.5 mm distal to the origin of the medial femoral condyle, and proximal to the level of the posterior point of Blumensaat’s line (Fig. 91-7).91 The ligament courses from its femoral origin to attach to the superior medial border of the patella and the undersurface of the vastus medialis. Several studies14,25,39,46,75 undertaken to compare the roles of the MPFL, medial patellar retinaculum, patellotibial ligament, patellomeniscal ligament, and lateral retinaculum have found that the MPFL provides between 50% and 80% of soft tissue restraint to lateral patellar displacement in functional positions of slight knee flexion. Several authors31,95 have investigated the isometricity of various origin and insertion positions for MPFL reconstruction. The best results were obtained by using the anatomic femoral and patellar attachments (Fig. 91-8). Superior displacement of the femoral attachment resulted in increased distance between insertion sites as the knee moved into greater flexion, which could lead to loss of knee flexion or disruption of the graft after MPFL reconstruction. Proximal malposition coupled with a shorter than anatomic MPFL graft substitute appears to result in significantly increased medial patellar tilt and retropatellar pressure.31 Inferior displacement of the femoral insertion (see Fig. 91-5, position F3) results in minimal changes in graft length and tension during the first 40 degrees of knee flexion, followed by decreased graft tension with continued flexion, at which point the bony architecture has taken on a primary stabilizing role.
Imaging and surgical exploration studies60,88,89 have found the MPFL to be routinely injured at the time of patellar dislocation. Disruption appears to occur most often at the adductor tubercle, but it may take place along the length of the ligament or its patellar attachment. In patients with chronic dislocation, Nomura75 reported that the MPFL is healed throughout its course with scar tissue, unhealed with femoral avulsion, or atrophied throughout its course. Laboratory studies and clinical reports* have indicated that repair or reconstruction of the MPFL is integral to reestablishing lateral patellar stability.
Muscle contraction may affect patellofemoral stability by “seating” the articulation as a result of increased joint reaction forces, or by generating dynamic medial or lateral displacement forces.96 Relative vectors of the individual quadriceps muscular components are determined by their level of attachment, angle of pull, and cross-sectional area. The vastus medialis obliquus (VMO) is a primary dynamic stabilizer. It is intimately associated with the MPFL and the adductor musculature. Although conceptually interesting, independent function, disuse, or rehabilitation of the VMO separate from the remaining quadriceps has not been proved.1,53,83 Musculotendinous units are primarily dynamic actors, and advancement of the VMO to increase passive restraint to lateral patellar dislocation is unpredictable.96
The bony architecture of the patellofemoral joint also plays a role in stability. Trochlear dysplasia, altered convexity of the retropatellar surface, patella alta, and patellar hypoplasia all have been found to be risk factors for initial and recurrent patellar instability.34,47,50 The normal sulcus angle for young normal individuals has been reported to be 138 ± 3 degrees.86,103 Mild trochlear dysplasia corresponds to a sulcus angle of 143 degrees, moderate dysplasia to an angle of 149 degrees, and severe dysplasia to an angle of 171 degrees.22 Runow87 found the average sulcus angle in a large group of young patients with documented patellar dislocation to be increased to 146 ± 6 degrees. A very similar increase to 147 degrees has been reported by Aglietti and associates2 in symptomatic patellar subluxers.
With the knee in full extension, the patella rests lateral and superior to the trochlea. Engagement occurs between 10 and 30 degrees of flexion. This is dependent on relative patellar tendon length, and in individuals with patella alta, engagement will occur later in flexion. This condition leads to less stability in early degrees of knee flexion, in which most sporting activity occurs. For the adolescent and young adult population, the Insall ratio has been measured as 0.98 ± 0.13 for males and 1.08 ± 0.15 for females.87 In a study of 104 patellar dislocators, Runow87 found that the average Insall ratio was greater than 1.0 in all patients, and that a ratio greater than 1.3 was significantly correlated with recurrent and bilateral dislocation. Several other studies have reported that patella alta is a significant risk factor for initial and recurrent patellar instability.*
The Q angle is subtended by a line drawn from the anterior superior iliac spine to the center of the patella or the trochlear groove, and a second line drawn from the center of the tibial tubercle. An increased Q angle suggests a greater lateralizing vector on the patella. Unfortunately, no agreed-on standards are available for Q angle measurement with regard to the most appropriate degree of knee flexion, weight-bearing status, and quadriceps activity. Axial computed tomography (CT) scans can be used to generate more reproducible measurements of relative tibial tubercle “lateralization” by providing anterior tibial tuberosity–trochlear groove (TT-TG) distances9 and tibial tubercle–lateral condylar (TT-LC) angles.68 An increased Q angle is often discussed as a risk factor for instability, but it has not been reliably associated with patellar instability in many large-group studies.8,18,33,56 This may reflect the inability of a static measurement, made in a static situation, to capture dynamic, functional impairment. However, we do incorporate TT-TG and TT-LC measurement data when considering the need for distal realignment in combination with MPFL repair or reconstruction.
Risk Factors
As with other musculoskeletal injuries, risk factors for patellofemoral instability are best viewed within the disease triad of host (patient characteristics), agent (macrotraumatic or repetitive microtraumatic energy exchange), and environmental (physical and social milieu of athletic participation) risk factors.47,61 We classify young patients with patellofemoral instability into two large, somewhat overlapping groups (TONES and LAACS) based on “relative” risk factors, natural history, and characteristics (Table 91-1).
Table 91-1 Classification of Patellofemoral Instability in Young Patients: TONES and LAACS
Host factors that may play an important role in patellar instability include age, gender, previous history of patellar instability, generalized ligamentous laxity, and patellofemoral dysplasia. Patellar dislocation rates are highest during the second decade of life,8,34,87 probably because of higher athletic activity during this period and an underlying musculoskeletal predisposition in this age group. During a period of rapid growth, children and early adolescents are in the seemingly dichotomous situation of simultaneous musculotendinous tightness and relative ligamentous laxity. This is particularly apparent with the straplike, two-joint musculotendinous units crossing the knee. Tightness in the iliotibial band, abductors, and lateral hamstrings may lead to increased valgus vector on the patella, which may be poorly balanced by lax medial ligamentous restraints and poorly developed quadriceps musculature. Age is also a significant risk factor for recurrence, with earlier initial dislocation being a positive predictor of higher recurrence rates.* Generalized ligamentous laxity is correlated with earlier onset, more frequent recurrence, and dislocations that occur with lesser trauma.87 However, patellar dislocation in a hyperlax patient carries a significantly lower risk of concurrent osteochondral fracture.87,99 Patellofemoral markers that have been linked most reliably to increased dislocation and recurrence risk are patella alta, increased sulcus angle, and lateral dominance of the retropatellar surface. These dysplastic changes usually occur as a constellation and are more often seen in younger, hyperlax female LAACS-type patients (see Table 91-1). However, subtle abnormalities in these measurements are often noted among TONES-type patients as well (see Table 91-1). A key host characteristic of recurrent dislocation is a history of previous dislocation.34
Trauma, in varying degrees, is almost always associated with patellar dislocation. A large population-based study conducted by Atkin and colleagues8 points to the “agent” of high sports participation as the major risk factor for first-time, acute patellofemoral dislocators. The most common mechanism of patellar dislocation—noncontact external rotation of the lower part of the leg on a planted foot, resulting in valgus overload of the extensor mechanism—is common in sports participation. In their group of TONES-type patients, investigators reported no predictive role for gender, family history, increased Q angle, or excessive hip rotation. Patella alta was the one traditional factor associated with higher risk in this patient group. In TONES patients, patellar dislocation is a more traumatic event, with higher rates of magnetic resonance imaging (MRI)-documented disruption of the MPFL, VMO, and medial retinaculum. Fithian and coworkers34 suggested that increased soft tissue trauma is a sign of macrotrauma to normal structures, and that given adequate chance to heal, a lower risk of recurrence will be seen than in cases in which the patella dislocates with less trauma. Osteochondral fracture rates are significantly higher in TONES patients as a result of the greater stress required to dislocate the patellofemoral joint in patients with more normal soft tissue function. It is interesting to note that fractures tend to be avulsion-type or intra-articular osteochondral in nature, but the two rarely occur concurrently.103 An initial avulsion may serve to decompress the patellofemoral joint, thus decreasing stress between the retropatellar surface and the lateral femoral condyle. Sports, dance, and other high-demand activities are often the primary cause of injury in initial dislocators. Even most LAACS-type patients will report some level of trauma as precipitating a recurrent event. Only in the small group of “habitual” dislocators does the patella routinely dislocate with normal gait.
Classification
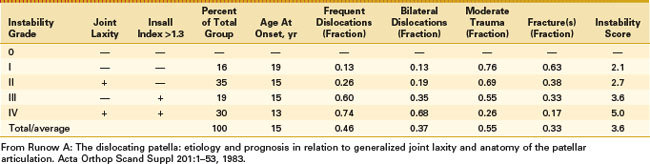
A myriad of classification systems for patellofemoral instability and maltracking have been devised. In his classic treatise on patellofemoral instability, Anders Runow87 grouped initial dislocators into four groups. Group I had only minimal patella alta (Insall ratio of 1.0 to 1.3), minimal trochlear dysplasia, and no generalized hyperlaxity. Seventy-six percent of these patients experienced significant trauma causing the dislocation; they had an average age at initial onset of 19 and a low rate of recurrence, and osteochondral fractures occurred in 63%. Group II had generalized hyperlaxity and an Insall ratio of 1.0 to 1.3, whereas group III had normal soft tissue function but an Insall ratio greater than 1.3. Group IV demonstrated both hyperlaxity and severe patella alta. Among group IV patients, the age at onset was 13, the recurrence rate was 74%, bilateral involvement occurred in 68%, significant trauma played a role in only 28%, and osteochondral fractures occurred in only 17% (Table 91-2). In a recent comprehensive population study, Fithian and coworkers34 classified acute dislocators into those with and without a history of previous dislocation. Those with a history of previous dislocation were more likely female and had a higher risk of future dislocation, a positive family history for patellar instability, higher rates of dysplastic hip disease, and increases in patella alta, patellar tilt, and patellar subluxation. As discussed earlier, we have found that grouping patients generally into the TONES and LAACS classifications is useful in assessing risk factors, discussing the natural history, and guiding treatment options.
Natural History
Well-controlled, population-based studies have estimated the per capita risk for first-time dislocation in children and adolescents to be between 29 and 43 per 100,000.8,34,71 The natural history of this fairly common major knee malady is not benign. A significant number of patients experience recurrent instability and/or patellofemoral pain related to maltracking or osteochondral injury. For nonoperative patients, reported redislocation rates vary widely from 15% to 45%, and 30% to 50% may be expected to suffer anterior knee pain.10,47 Less than perfect outcomes after nonoperative care suggest the need for early surgical intervention. However, the results of early operative repair have been mixed.* Results of early surgical intervention appear to decline over time and may be less favorable in LAACS-type patients.101 As discussed earlier, the natural history after an acute dislocation is dependent on host, agent, and environmental risk factors for the individual patient. Fithian and associates,34 in their group of first-time dislocators, reported recurrent instability in 49% of patients with a previous history of instability and only a 17% recurrence rate. Runow87 reported a redislocation rate of only 13% in his group I patients without laxity or patellofemoral dysplasia. However, the rate jumped to 74% in group IV patients with both generalized hypermobility and patellofemoral dysplasia. In their study of 100 young acute dislocators, Mäenpää and colleagues58 found a redislocation rate of 44%, patellofemoral pain in 19%, and no complaints after nonoperative treatment in only 37% of patients. However, of 14 patients who underwent surgical reconstruction, 47% continued to have a positive apprehension sign and 79% had significant retropatellar crepitance. In a randomized study of nonoperative and operative treatment, Nikku and coworkers reported recurrent instability rates of 20% in their nonoperative group and 18% in their operative group and overall better function in their nonoperative patients.74 In a large group of male Army conscripts with an average age of 20 years who underwent surgery for acute or recurrent patellar dislocation, Mäenpää and associates58 found that only 19% had excellent results. Just 35% were able to finish their military service normally after surgical intervention.
A systematic review of 70 articles on first-time dislocators speaks to the lack of a definitive treatment algorithm for treating young patients with acute patellar dislocation.100 Many studies are retrospective in nature, are short term in follow-up, use various and sometimes dated surgical interventions, suffer from subject/treatment selection bias, and lack defined outcomes variables. This review recommended nonoperative care for the first-time dislocator except in cases of comorbid osteochondral injury, early recurrent dislocation, substantial disruption of the MPFL-VMO-adductor mechanism, or failure to progress with nonoperative care. We follow similar guidelines but would also offer early operative intervention to LAACS-type patients who have had contralateral repetitive dislocation (often proximal and distal reconstruction) and to high-demand athletes whose competitive schedules will not tolerate downtime or future dislocation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree