Overuse Injuries of the Upper Limb
INTRODUCTION
Sports are inseparably woven into the fabric of our lives. Be it as recreational participants, serious competitors, supportive parents, professional coaches, backyard teachers, or avid fans, all of us are directly or indirectly involved in sporting activities. And it is no different for our children.
While the physical, emotional, and developmental benefits of physical activity are well established, life is full of risks.1 Inherent in any sports participation is the risk for traumatic or overuse injury. Given the spectrum within which these sports-related injuries affect the upper limb, it is common for these conditions to present to the pediatric hand and upper extremity surgeon. Although the vast majority of sports injuries may be managed via nonoperative means, often surgical treatment is required to alleviate pain, restore function, and allow return to prior levels of participation.
The purpose of this chapter is to describe the evaluation and treatment of sports-related injuries. While this chapter focuses on several common overuse conditions amenable to nonoperative care, the ensuing chapters discuss injuries of the upper extremity commonly requiring surgical treatment.
YOUTH SPORTS PARTICIPATION AND INJURY
I’m tired of hearing about money, money, money, money, money. I just want to play the game, drink Pepsi, wear Reebok.
—Shaquille O’Neal
The number of children and adolescents involved in sports continues to grow. While it is estimated that 32 million were involved in organized sports in the United States in 1997, it is now believed that over 44 million US children and adolescents participate in organized sporting activities.2 As the enthusiasm for youth athletics grows, so too will participation rates among children and adolescents.
With this increased participation has come an increased incidence of sports-related injuries. An estimated 2.5 million emergency room visits are due to sports-related injuries each year in the United States.3 Furthermore, it is estimated that sports-related injuries account for up to 20% of all primary care physician evaluations for injuries in the pediatric population.4 Prior epidemiological studies have demonstrated an incidence of 2.51 injuries: 1,000 athlete exposures among US high school students alone, accounting for approximately 1.5 million injuries per year.5,6
Skeletally immature athletes are particularly vulnerable to sports-related injury due to a variety of physiologic and environmental factors. Growing athletes are growing children, and physiologically their bodies are changing. Bones are lengthening and muscles are maturing, leading to an inherent imbalance between strength and flexibility, predisposing to injury.7 Open physes are also susceptible to traumatic and overuse injuries, as they are less resistant to compression and shear forces than the adjacent bone.8,9 Furthermore, the extremities in young athletes may be subjected to greater forces given the changes in body composition. The increased obesity seen in the United States and other developed nations is further cause for concern.
In addition to these physiologic factors, a number of societal and environmental trends may be raising the frequency of youth sports injuries. The age of first sports participation is becoming younger and younger. Youth athletes are now raised in an era of specialization, in which sports participation is year-round, with few breaks between seasons or opportunities to pursue varied physical activities.10 In addition, the financial investment and rewards of youth sports participation continue to increase. Scholarships are given, television contracts are negotiated, and money is made in the industry of youth sports. (e.g., every game of the Little League World Series was televised in
2010. For the 2009 financial year, Little League Baseball reported net revenues of over $21 million and had net assets worth over $70 million!) Given the social climate, families and coaches are now pushing their young athletes to participate at unprecedented levels. All of these factors are leading to startling increases in repetitive, overuse injuries and more violent acute injuries at a young age. The extreme sports are at an entirely different level of concern.
2010. For the 2009 financial year, Little League Baseball reported net revenues of over $21 million and had net assets worth over $70 million!) Given the social climate, families and coaches are now pushing their young athletes to participate at unprecedented levels. All of these factors are leading to startling increases in repetitive, overuse injuries and more violent acute injuries at a young age. The extreme sports are at an entirely different level of concern.
COMMON OVERUSE INJURIES BY ANATOMIC REGION
I’ve come to accept that the life of a frontrunner is a hard one, that he will suffer more injuries than most men and that many of these injuries will not be accidental.
—Pele
SHOULDER: INTERNAL ROTATION DEFICIT AND PHYSEAL STRESS INJURY
Shoulder complaints are common in the youth overhead athlete, particularly in the baseball pitcher and other repetitive overhead athletes. Indeed, in a previous longitudinal study of 298 youth baseball pitchers, for example, approximately one-third developed shoulder pain over the course of two seasons.11 Epidemiological data like this reinforce the common observation that shoulder pain is a frequent complaint in young throwers and overhead athletes.
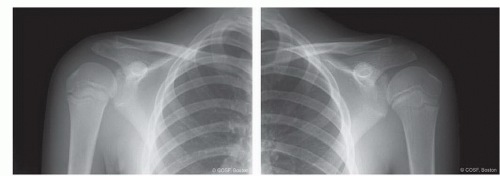
The term “Little League shoulder” has often been used to describe shoulder pain in skeletally immature throwers. While this term is liberally used to describe a host of different clinical entities, in most situations it denotes a repetitive stress injury to the proximal humeral physis12 (Figure 39-1). While the exact mechanism is unknown, it is theorized that repetitive throwing imparts excessive rotational torque and tension to the proximal humeral physis, resulting in pain, tenderness, and characteristic radiographic changes.
Previous biomechanical analyses have demonstrated that external rotation torques approximate 18 Nm during pitching, 400% of the mechanical tolerance of physeal cartilage. Distraction forces may be as high as 200 Nm in the adolescent shoulder, representing 5% of the physeal cartilage strength.13,14 These forces are thought to be highest during the late cocking to late release phases of the pitching motion. It has been hypothesized that these rotational and tensile forces cause “microfractures” across the physeal zone of hypertrophy, which may be vulnerable to greater injury due to the orientation of the collagen fibers and relatively low mechanical strength.15,16
Not surprisingly, this condition is most commonly seen in skeletally immature athletes between the ages of 9 and 15, at a time in which the physis is metabolically active and vulnerable to injury. Additional risk factors include arm pain and fatigue during pitching, pitch counts of higher than 80 per game, and pitching over more than 8 months per calendar year.17
Clinical Presentation and Evaluation
Patients will typically present with insidious onset shoulder pain, exacerbated during and after throwing. The pain is usually localized to the anterior and lateral aspect of the shoulder, and there is often tenderness to percussion and deep palpation of the proximal humerus. Abduction and forward flexion motion and strength are frequently unaffected but may be limited at the time of presentation due to pain.
Careful examination of internal and external rotation will often demonstrate greater external rotation and less internal rotation than the unaffected, nonthrowing shoulder, the so-called glenohumeral internal rotation deficit (GIRD).18, 19, 20, 21 and 22 Unlike older adults, it should be noted that young overhead athletes may often have GIRD without an associated increase in external rotation.18 Care should be made during assessment of shoulder rotation to prevent scapular elevation and protraction, which is typically
recruited to compensate for loss of glenohumeral joint internal rotation. This may lead to scapulothoracic dyskinesis and asymmetric scapulothoracic motion during shoulder range-of-motion testing. If the GIRD and/or scapulothoracic dyskinesis are severe, provocative testing for internal impingement and superior labral/long head of biceps pathology may be positive.
recruited to compensate for loss of glenohumeral joint internal rotation. This may lead to scapulothoracic dyskinesis and asymmetric scapulothoracic motion during shoulder range-of-motion testing. If the GIRD and/or scapulothoracic dyskinesis are severe, provocative testing for internal impingement and superior labral/long head of biceps pathology may be positive.
Radiographic Evaluation
Plain radiographs of the shoulder should be examined in patients with significant pain and tenderness, even in the absence of an obvious traumatic event. Standard anteroposterior (AP), scapular Y, and axillary views are sufficient, though an AP in external rotation may allow for better visualization of the undulating proximal humeral physis. Characteristic findings consistent with epiphysiolysis include physeal widening, cystic changes, juxtaphyseal sclerosis, or periosteal reaction.23 As these findings are often subtle and difficult to distinguish from the normal physis, contralateral comparison radiographs are helpful (Figure 39-1).
Treatment
As with all overuse sporting injuries, prevention remains the key to treatment. For youth baseball pitchers, a number of formal guidelines have been developed to regulate the quantity and quality of throwing allowed to young throwers (Tables 39.1 and 39.2). Derived from epidemiological data of shoulder injuries in youth throwers and formulated by a consensus of baseball and medical experts, these guidelines attempt to minimize the risk of overuse injury.27,28
Table 39.1 Youth baseball pitching guidelines | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In addition to rules and guidelines, efforts should be made to educate young throwers on proper pitching mechanics, appropriate warm-up and cool-down activities, and pertinent stretching and strengthening regimens to avoid injury due to mechanical failure.
However, further work needs to be done. Guidelines are helpful and applicable to the general population, yet to date they are mostly based upon chronological age rather than physiological status. (While some 12-year-olds are shaving, others have yet to begin their preadolescent growth spurt.) In addition, there is little oversight and monitoring of athletes involved with multiple teams in multiple leagues during the same season, an increasingly common phenomenon in today’s highly competitive climate. Furthermore, though great attention has been paid to youth baseball pitchers, little scientific information exists on the risks and recommendations for other position players or other overhead sports (e.g., softball, tennis). Finally, in the era of specialization and earlier sports participation, better guidelines need to be created regarding the optimal time spent away from throwing and baseball between seasons.
In patients with established proximal humeral physeal stress injury, treatment is predicated on rest until there is resolution of pain and tenderness. While highly variable, this typically involves cessation of all throwing activities for 6 to 12 weeks. After the acute pain—and presumably physeal stress injury—has resolved, physical therapy is initiated for range of motion and strengthening. Particular attention is given to “sleeper stretches” to improve internal rotation and periscapular strengthening to address scapulothoracic dyskinesis, hyperangulation, and internal impingement. Advancement to an interval throwing program with attention to pitching mechanics is then begun, adhering to the “soreness rules”23,29,30 (Tables 39.3 and 39.4). Patients and families should be counseled that this process is dynamic and may indeed take months to complete.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree