Chapter 19 Otorhinolaryngology
Emergencies
Epiglottitis
Differential diagnosis includes tonsillitis, peritonsillar abscess, retropharyngeal abscess, airway foreign body, and croup. Physical examination with laryngoscopy is extremely useful in differentiating these diagnoses. Endoscopy should not be performed if there is concern of impending airway obstruction. Endoscopy will typically show erythema and edema of the epiglottis and arytenoid cartilages. Other findings include laryngeal tenderness on neck palpation, although palpation should be avoided when the diagnosis is being considered.
Any time the diagnosis of epiglottitis is in question, otorhinolaryngologic (ear-nose-throat, ENT) and infectious disease consultations are warranted. Placement of a tongue depressor has been known to precipitate acute airway obstruction and should be avoided entirely if epiglottitis is strongly suspected. Differentiation from croup can be difficult because there is considerable overlap of symptoms (Table 19-1) (Berry and Yemen, 1994). A lateral extended neck radiograph can help in the diagnosis. X-ray evidence includes the classic “thumbprint” sign. If epiglottitis is suspected or lateral neck radiography is confirmatory, the patient should be taken to the operating room (OR) for orotracheal intubation in the presence of an anesthesiologist and an otorhinolaryngologist. In any case of airway obstruction, cricothyrotomy or tracheotomy can be lifesaving, because orotracheal intubation can be difficult and sometimes impossible. Some patients, usually adults, may be treated expectantly with intravenous (IV) medications and intensive care unit (ICU) observation as long as personnel are available for control of the airway if necessary. If airway stability is questionable, observation is not recommended.
Table 19-1 Distinguishing Features of Epiglottitis and Croup
| Feature | Epiglottitis | Croup |
|---|---|---|
| Cause | Bacterial | Viral |
| Age | 1 year to adult | 1 to 5 years |
| Location of obstruction | Supraglottic | Subglottic |
| Onset | Sudden (hours) | Gradual (days) |
| Fever | High | Low grade |
| Dysphagia | Marked | None |
| Drooling | Present | Minimal |
| Posture | Sitting | Recumbent |
| Toxemia | Mild to severe | Mild |
| Cough | Usually none | Barking, brassy, spontaneous |
| Voice | Clear to muffled | Hoarse |
| Respiratory rate | Normal to rapid | Rapid |
| Larynx palpation | Tender | Not tender |
| Clinical course | Shorter | Longer |
From Berry FA, Yemen TA. Pediatric airway in health and disease. Pediatr Clin North Am 1994;41:153.
Peritonsillar Abscess
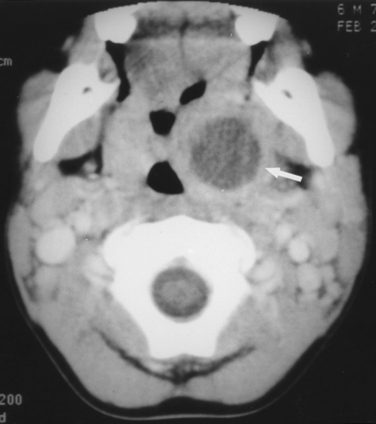
The typical signs and symptoms of peritonsillar abscess include fever, sore throat for 3 to 5 days, dysphagia, odynophagia, and a muffled, “hot potato” voice. Trismus is extremely common. Examination confirms asymmetric tonsils and peritonsillar edema and erythema. The soft palate and uvula are swollen and displaced away from the side of the abscess. It is often difficult to distinguish between abscess and peritonsillar cellulitis. If possible, it is helpful to palpate because fluctuance indicates a loculation of pus. Diagnosis is often made by clinical impression, but computed tomography (CT) can be confirmatory and useful when the diagnosis is uncertain (Fig. 19-1).
If untreated, a peritonsillar abscess may spontaneously drain, progress to involve the deep neck, or even lead to airway obstruction. The most important part of the treatment is drainage of the abscess cavity by needle aspiration, incision and drainage, or tonsillectomy. Cultures of the aspirate can be obtained, and broad-spectrum antibiotics should be started. Appropriate antibiotics include ampicillin-sulbactam (Unasyn) or clindamycin (Cleocin). Many patients present with dehydration, and parenteral fluids should be given if necessary. Analgesics should be prescribed as needed. One or two doses of IV corticosteroids may be given to decrease inflammation and pain.
Foreign Bodies
Esophagus
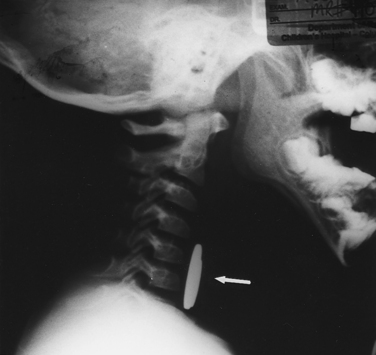
Plain radiographs (including lateral films) are often diagnostic in pediatric patients because most esophageal foreign objects are radiopaque (Fig. 19-2). Other radiologic findings that can suggest a foreign body include increased soft tissue density in the prevertebral space, mediastinal widening, air-fluid levels in the esophagus, and paraesophageal air. Disk batteries require a high index of suspicion because they can cause significant tissue injury and lead to esophageal perforation if they are not removed emergently. They have a classic appearance when viewed laterally, approximating a dime resting on a nickel (similar to the appearance of Fig. 19-2).
Airway
As with esophageal foreign bodies, airway foreign bodies are much more common in infants and young children. Many deaths from foreign-body aspiration occur in the home before medical intervention can be administered. The most frequently aspirated foreign bodies are foods, with nuts leading the list. Foreign bodies aspirated into the airway are usually found lodged in the bronchial tree but can also be found in the larynx or trachea. If the event is witnessed and results in complete airway obstruction, a Heimlich maneuver should be administered; however, the event is often not witnessed. Symptoms can include hoarseness, persistent cough, wheezing, or stridor if the foreign body is lodged in the trachea or larynx. Because the potential for morbidity and mortality is substantial, this condition requires urgent diagnosis and timely intervention to prevent catastrophe.
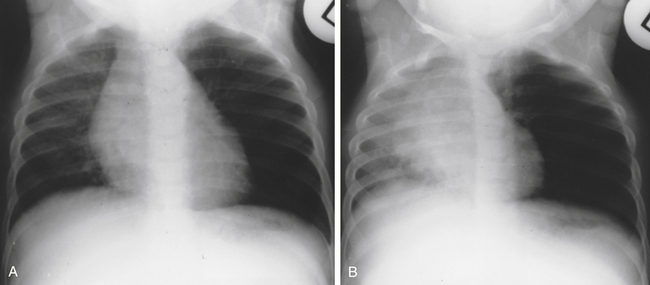
The most important diagnostic step for identifying a foreign body is a high index of suspicion. Careful auscultation of the lung fields is essential because subtle asymmetric differences may be found. Because most airway foreign bodies are radiolucent, chest radiographs can be normal, but abnormalities such as hyperinflation, atelectasis, or pneumonia can be present (Fig. 19-3). If plain radiographs are equivocal or normal and the patient is in stable condition, airway fluoroscopy can be helpful.
Epistaxis
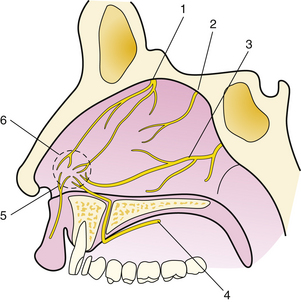
Epistaxis is classified according to its location. Bleeding from the anterior nasal cavity is most common and usually originates from a rich plexus of vessels at the anterior septum called Kiesselbach’s plexus (Fig. 19-4). Bleeding from this location, although troublesome, is less likely to be severe and is usually easier to control than posterior epistaxis. Posterior epistaxis originates from the posterior two thirds of the nasal cavity and can be quite severe and much more difficult to control.
Treatment
Effective treatment requires adequate visualization and patient cooperation. The level of intervention by the primary care physician depends on level of experience, comfort level, and availability of appropriate supplies and equipment. ENT consultation should be considered when any of these prerequisites cannot be met. The patient should be reassured and given an explanation of the planned treatment. This results in better cooperation and decreases patient anxiety, improving treatment success. A bright headlight, nasal speculum, large nasal (Frazier tip) suction, and bayonet forceps are required. If the patient is monitored and stable, a small dose of IV narcotics titrated for analgesia and anxiolytic effect may be given. Extreme caution should be taken not to oversedate the patient. Also, instrumentation of the nose can lead to a significant vasovagal response that may be accentuated in a hypovolemic patient given narcotics. It is advised to err on the side of caution with regard to narcotic medication both during and after treatment.
Other Techniques
Rarely, epistaxis cannot be controlled with packing, requiring further intervention. This can include intraoperative endoscopic cautery, endoscopic or open arterial ligation, or angiography with selective embolization of the offending vessel. There are advantages and disadvantages to each of these techniques. In general, the surgical techniques are usually favored over embolization if there are no significant contraindications to surgery. All the surgical techniques have very high success rates. Embolization is also effective when performed by an experienced invasive radiologist, but it does carry the relatively low risk of inadvertent embolization of the internal carotid artery system and subsequent ischemic cerebral injury, which can be devastating.
Head and Neck Trauma and Respiratory Embarrassment
The Ear
Otalgia
While the vast majority of patients with otalgia have an otologic cause, the clinician must recognize that otalgia may be referred. Sensory innervation of the ear includes cranial nerves V, VII, IX, and X, and therefore disorders of structures with similar innervation can cause otalgia. It is imperative that the physician not simply attribute otalgia to an ear infection unless the physical examination supports this diagnosis. Otalgia can result from dysfunction of the nose, sinuses, oral cavity, pharynx, larynx, dentition, temporomandibular joints, and salivary glands. These structures must be thoroughly assessed, especially if the examination of the ear appears normal. This is especially true in smokers, whose initial symptom of laryngopharyngeal carcinoma may be otalgia. Otolaryngologic referral for laryngoscopy may be indicated with suspected referred otalgia. (See eBox 19-1 and eBox 19-2 online at www.expertconsult.com for differential diagnosis of otalgia.)
Box 19-2 Causes of Tinnitus
From Lucente FE, Har-El G: Essentials of Otolaryngology. Philadelphia, Lippincott–Williams & Wilkins, 1999, p 110.
Subjective
Tumors of the Ear
Vertigo
Because patients use “dizzy” to describe many sensations, the actual sensation is best clarified by a detailed history (Box 19-1). The major studies on the causes of persistent dizziness, from Drachman and Hart (1972) to Davis (1994), all describe four diagnostic categories: lightheadedness, presyncope, disequilibrium, and vertigo. The investigators all conclude that the most common cause of persistent dizziness is a peripheral vestibular disorder (38%-56% of cases) followed closely by a psychogenic disorder (6%-33%). In about 25% of patients, the complaint is the result of the combined effects of multiple sensory deficits, medications, or orthostasis, leading to complaints of presyncope, lightheadedness, or disequilibrium. Finally, central vestibular etiologies are unusual and represent less than 10% of all causes.
Laboratory testing can include an audiogram if no specific cause of vertigo can be found after the medical history and physical examination. Electronystagmography (ENG) is an objective study of the vestibular system and can help localize a vestibular lesion. Electrodes placed about the eye sense the movements of nystagmus as either spontaneous or initiated by maneuvers such as caloric testing, positioning, optokinetics, and pendulum tracing. A brain MRI scan is indicated in patients with unilateral otologic symptoms and in those unresponsive to treatment. Blood tests, when necessary, can include CBC, rapid plasma reagin (RPR), vitamin B12 level, folate level, drug screens, and heavy metal testing when indicated.
Benign Paroxysmal Positional Vertigo
An expert panel convened by the American Academy of Otolaryngology–Head and Neck Surgery Foundation recommended against “routinely treating BPPV with vestibular suppressant medication such as antihistamines or benzodiazepines” (Bhattacharyya et al., 2008). Because of the variability of symptoms, the clinician must judge each case independently. Resolution occurs in a few weeks or months, and the condition is benign, although it can recur.
Tinnitus
Tinnitus is a term used to describe an internal noise perceived by the patient. It is usually, but not always, indicative of an otologic problem. Tinnitus is most often subjective, that is, heard only by the patient. However, it can be objective and heard by the patient and the examiner. In most cases, tinnitus is secondary to bilateral sensorineural hearing loss and requires no further evaluation. In rare cases, tinnitus can be a symptom of a vascular abnormality (aneurysm or arteriovenous malformation), hypermetabolic state, or intracranial mass that, if not evaluated, could result in delayed treatment. Middle ear and rarely external ear pathology can also cause tinnitus, as can numerous medications (Box 19-2). The patient’s medications should be reviewed.
In cases of pulsatile tinnitus with normal otoscopy, magnetic resonance angiography (MRA) is performed to evaluate for vascular abnormalities. If otoscopy identifies a retrotympanic mass, a temporal bone CT is obtained to evaluate for a vascular mass or abnormality. Blood tests can be performed to rule out anemia or hyperthyroidism, which can result in a hypermetabolic state and cause tinnitus secondary to increased blood flow near the cochlea. Auscultation of the neck, periauricular area, and chest may identify a bruit or murmur, indicating a need for a carotid duplex ultrasound study or echocardiogram, respectively. Most cases of arterial pulsatile tinnitus are secondary to atherosclerotic carotid artery disease. Venous pulsatile tinnitus often improves with digital pressure over the internal jugular vein. Etiologies include idiopathic venous hum, a high-riding jugular bulb, or benign intracranial hypertension.
Disorders of the External Ear
Otitis Externa
Auricular Hematoma
Although a Cochrane review could not define the best treatment for an acute auricular hematoma, a frequently successful treatment involves incision and drainage with dental rolls sutured to the anterior and posterior auricle (Fig. 19-5). Needle aspiration alone will often lead to recurrences. The bolster is usually left in place for 4 to 7 days, with the patient permitted to return to wrestling or boxing with headgear. Prophylactic antistaphylococcal antibiotics are given. For a long-standing hematoma or a cauliflower ear, debridement of fibrosis and cartilage is necessary (Jones and Mahendran, 2008).
Cerumen
In most people, cleaning the external meatus with a finger in a washcloth while bathing is sufficient to maintain the ear canals. Treatment of cerumen impaction by the clinician may involve ceruminolytic agents, irrigation, or manual removal. Ceruminolytic agents include water-based, oil-based, and non-water-, non-oil-based solutions. A Cochrane review found that any type of ear drop (including water and saline) is more effective than no treatment, but study quality was lacking. Office irrigations may be performed using a large syringe with a large angiocatheter tip. The type of irrigant solution used is probably not critical, although a tepid or warm temperature is important to prevent the patient from becoming vertiginous from a labyrinthine caloric response. Instilling a ceruminolytic 15 minutes before irrigation may improve the success rate. Irrigations should not be performed in those with tympanic membrane perforations or previous ear surgery. Of note, irrigation with tap water has been implicated as a causative factor in malignant otitis externa. Therefore, instilling an acidifying ear drop after irrigation in diabetic patients is recommended. Manual removal requires knowledge of ear anatomy and special care to avoid trauma. A handheld otoscope with a curette and other instruments may be used. Otolaryngologists will often use binocular microscopy to aid with visualization. Those patients inquiring about ear candling should be informed that it has not been shown to be effective and presents a risk of thermal injury to the ear (Burton and Doree, 2008).
Disorders of the Middle Ear
Otitis Media
Acute Otitis Media
The primary cause of bacterial colonization of the middle ear is eustachian tube dysfunction. Abnormal tubal compliance in addition to delayed innervation of the tensor veli palatini muscle leads to collapse of the eustachian tube. Aerobic and anaerobic organisms, as well as viruses, can contribute to middle ear infection (Heikkinen et al., 1999). The three most common bacteria involved in AOM are S. pneumoniae (25%-40% of cases), H. influenzae (10%-30%), and Moraxella catarrhalis (2%-15%) (Klein, 2004). Risk factors most often associated with AOM are child care outside the home and parental smoking. Box 19-3 lists the common risk factors for AOM. A viral upper respiratory infection usually precedes an episode of AOM.
Three criteria are necessary to confirm the diagnosis of AOM: acute onset, presence of middle ear effusion, and signs or symptoms of middle ear inflammation (American Academy of Pediatrics [AAP], 2004; Level of evidence [Grade] B). Middle ear effusion can be diagnosed by direct visualization of air-fluid levels behind the tympanic membrane, a bulging drum, lack of movement on pneumatic otoscopy, or a flat tympanogram readout that indicates no tympanic membrane movement and therefore the presence of middle ear effusion. Redness of the tympanic membrane, pain, and fever are the most common signs and symptoms of middle ear inflammation (see eBox 19-4 online). Erythema of the tympanic membrane without middle ear effusion is myringitis or tympanitis and is a separate diagnosis from AOM. Ear pain in the presence of a normal-appearing, flaccid tympanic membrane indicates causes other than AOM (Box 19-4).
The standard of care for the treatment of AOM in children older than 2 years is not to treat with antibiotics at the first visit, but to treat the pain and either observe the patient or prescribe an antimicrobial agent depending on certain criteria. The decision either to begin antibiotics or to observe the patient without them is based on the certainty of diagnosis, severity of symptoms, and age of the patient (AAP, 2004). (Table 19-2).
Table 19-2 Treatment of Acute Otitis Media
| Features | Treatment |
|---|---|
| Low-Risk Patients | |
| Older than 6 years, no antimicrobial therapy within past 3 months, no otorrhea, not in daycare, and temperature <38° C (<100.5° F) | Amoxicillin: 40-50 mg/kg/day in divided doses for 5 days |
| High-Risk Patients | |
| Younger than 2 years, in daycare, treated with antimicrobials within past 3 months, otorrhea, or temperature >38° C (>100.5° F) | Amoxicillin: 80-90 mg/kg/day in divided doses for 10 days |
| Treatment Failure | |
| Signs and symptoms persisting after 3 days | |
| Penicillin-Allergic Patient | |
| Any | |
TMP-SMX, Trimethoprim-sulfamethoxazole; bid, twice daily.
When all three criteria for the diagnosis of AOM are met (acute onset, middle ear effusion, and inflammation), the diagnosis is certain, and antibiotic therapy is indicated for any child 2 years old or younger (AAP, 2004; Grade A). For children older than 2 years, observation is an option if the illness is not severe and the parents can be relied on to report the patient’s status and can obtain medication if necessary. Severe illness is defined as moderate to severe otalgia and fever higher than 39° C. (102.2° F.) When two or fewer diagnostic criteria are present, diagnosis is considered uncertain, and observation is allowed for children 6 months and older with nonsevere illness.
If the initial antibiotic fails to resolve symptoms in 72 hours (pain, fever, redness and bulging of the tympanic membrane, otorrhea), high-dose amoxicillin–clavulanic acid is recommended. Alternatives in penicillin-allergic patients include the antibiotics cited earlier. Patients who do not respond to amoxicillin–clavulanic acid therapy should be treated with intramuscular ceftriaxone for 3 days. This antibiotic in a single dose can also be used initially if the child is vomiting or unable to keep down oral medication. Doses of antimicrobials are given in Table 19-2.
KEY TREATMENT
Otitis Media with Effusion
Otitis media with effusion (OME) is defined as persistent middle ear fluid without pain, fever, or redness of the tympanic membrane. It is often the result of AOM but can occur de novo. About 90% of children have OME before they reach school age. About 80% to 90% of cases resolve within 3 months and 95% within 1 year. Table 19-3 provides the Agency for Health Care Policy and Research (AHCPR) guidelines for treatment of OME.
Table 19-3 AHCPR Guidelines for Treatment of OME
| Duration of OME | Treatment |
|---|---|
| 6 weeks | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|