Chapter 51 Osteotomy and the Cruciate-Deficient Knee
Estimates report 100,000 new anterior cruciate ligament (ACL) injuries each year in the United States, with an overall incidence of 1/300,000 people.15 ACL injuries are frequently associated with dysfunction and impairment caused by knee joint instability, loss of proprioception, chondral and meniscal injuries, reduced quadriceps strength, and changes in the biomechanics of knee, with the risk of subsequent post-traumatic arthritis. Risk factors associated with ACL injury and implicated in the development of post-traumatic knee arthritis are meniscal injury, osteochondral pathology, malalignment, high levels of activity, genetic predisposition, obesity, age, and participating in high-level sports activities involving cutting, pivoting, and twisting.9,26 No previous studies have demonstrated that ACL reconstruction prevents the development of post-traumatic arthritis.11,25
Cruciate Injury and Arthrosis
In general, instability of the knee is not well tolerated and eventually post-traumatic arthritis develops. There is a significant amount of literature regarding ACL deficiency and post-traumatic arthritis. Some authors have reported the development of knee osteoarthritis (OA) after ACL injury in 50% of patients on average.9,25 Others have reported the development of OA in up to 70% of patients with combined ACL and meniscal injuries at 15 to 20 years after injury.20 Øiestad and colleagues,32 in a recent systematic review, indicated that the most accurate report of knee OA after isolated injury could be as low as 0% to 13%, and a prevalence of knee OA in combined ACL and meniscal injuries as high as 21% to 48%.
Patients with ACL and/or posterior cruciate ligament (PCL) deficiency, concomitant chondral and meniscal injuries, and preexisting malalignment of the knee are at increased risk of post-traumatic joint arthritis. In the case of ACL deficiency and underlying malalignment, with the loss of neuromuscular control, the knee is more likely to go into increased varus and overload the medial compartment. The varus knee with radiographic separation of the lateral tibiofemoral compartment and increased external rotation and hyperextension with an abnormal varus recurvatum position is referred to as a triple-varus knee.6,31 Medial joint pain, instability, and early degenerative joint disease may result in patients with this clinical scenario.
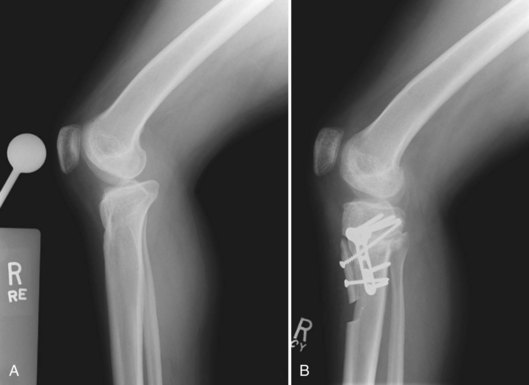
The medial compartment tends to have a posterior medial tibial plateau wear pattern in triple- varus knees (Fig. 51-1). This is thought to be caused by a chronic anterior subluxation of the tibia with respect to the femur.5 This pattern is further exacerbated by medial meniscal insufficiency. As the degenerative process progresses and the arthritic changes occur, the knee becomes less unstable. The patient begins to have arthritis-type complaints rather than instability complaints.
PCL-deficient knees are susceptible to posterior tibial subluxation and posterior instability.27 Mavrodontidis and associates30 have discussed two cases of rapid development of post-traumatic arthritis after failed PCL reconstruction. Instability of the knee joint leads to progressive knee arthritis. Much attention is devoted to soft tissue reconstruction, but surgeons may choose to ignore correctable risk factors for reconstruction failure such as joint malalignment. Frequently, joint malalignment contributes to the ligamentous injury prior to the discussion of reconstruction ever occurring. Geissler and Whipple16 found a 49% incidence of chondral defects and 36% incidence of meniscal tears in patients with chronic PCL instability. Keller and colleagues22 reviewed 40 PCL-deficient patients treated nonoperatively and found that 90% complained of knee pain with activity at 4 years from the time of injury, and only 12% of patients had normal-appearing radiographs. Clancy and associates8 found that 48% of patients with chronic PCL injuries had moderate to severe articular injury to the medial femoral condyle at the time of surgical reconstruction.
Posterior tibial slope and its relationship to instability in cruciate deficiency is also something to consider, particularly when considering osteotomy in these patients. Bonin and colleagues5 have described the relationship of pathologic tibial slope and incidence of ACL injury. The greater the slope, the greater the incidence of ACL instability. Giffin and associates,18,19 Agneskirchner and coworkers,1 and Dejour and Bonin12 have shown that increasing tibial slope alters tibial translation, and this is augmented in the cruciate-deficient knee (Fig. 51-2).
Indications for Osteotomy
Osteotomies have been used for localized medial and lateral compartment gonarthrosis with varus and valgus malalignment. The principle supporting the use of tibial osteotomy is redistribution of the mechanical force across the joint. Coventry10 initially described the indications for high tibial osteotomy to include stable knees with no subluxation or thrust, range of motion (ROM) of at least 15 to 100 degrees, localized medial compartment OA, minimal or no patellofemoral symptoms, and age younger than 65 years. Indications for high tibial osteotomies have since expanded for cases of posterior instability, ACL deficiency, and correcting tibial slope in sagittal instability.13,31 The senior author’s indications for osteotomy in the setting of instability are found in Box 51-1.
In the setting of ACL insufficiency with symptomatic instability and pathologic sagittal tibial slope, one should consider correction of the underlying malalignment issue in addition to ligamentous reconstruction. Previous observations of an increased incidence of ACL tears with increased tibial slope and biomechanical studies demonstrating increased anterior tibial translation with increasing tibial slope have suggested that decreasing the tibial slope would provide a more stable biomechanical environment.12,18,19 The PCL-deficient knee presents a contrary situation in which decreasing tibial slope causes an increase in posterior tibial translation and symptoms of instability (Fig. 51-3).
Preoperative Evaluation
Radiographic evaluation begins with assessment of the extent of knee arthrosis and lower extremity alignment with bilateral standard weight-bearing long-leg (hip to ankle) anteroposterior views, standard anteroposterior views in full extension, bilateral weight-bearing posteroanterior tunnel views in 30 degrees of flexion, and lateral and Merchant patellar views. Dugdale and coworkers14 have described the technique used to calculate the HTO correction. The mechanical axis and weight-bearing axis are determined and the correction to be made is calculated just lateral to the lateral tibial spine (Fig. 51-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree