Osteotomies of the First Metatarsal Shaft in Hallux Abducto Valgus
PART 1 Offset-V Osteotomy
Gary R. Bauer
Harold W. Vogler
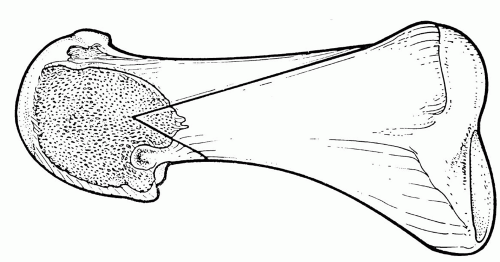
Shaft osteotomies may be employed in the repair of hallux abducto valgus deformities in some patients as an alternative to proximal procedures. The offset-V osteotomy is one type of shaft osteotomy and represents a modification of the Ludloff procedure (1). The procedure was first performed by Vogler in 1983 (2, 3, 4). The apex of the osteotomy is located at the distal metaphyseal-diaphyseal junction of the first metatarsal (Fig. 1). This zone, referred to as transitional bone, represents the junction between primarily cortical and cancellous bone (2). Compared with a base osteotomy, the procedure is performed at a more distal location with a shorter lever arm, and it allows protected weight-bearing ambulation in the immediate postoperative course. It has therefore been characterized as a “compromise osteotomy”(2). The procedure is useful in patients with cystic erosion of the metatarsal head that may make performance and stabilization of a metaphyseal type osteotomy difficult.
The intrinsic stability of the offset-V osteotomy is conferred by its geometry, with long dorsal and short plantar legs. The procedure is versatile and allows for reduction of intermetatarsal angles up to 18 degrees and proximal articular set angle deviation (PASA) in excess of 40 degrees. The reduction of the intermetatarsal angle is achieved through lateral translation of the capital fragment.
TECHNIQUE
Because of the diaphyseal location of the osteotomy and the degree of displacement of the capital fragment that is often achieved, surgical dissection is usually minimized to maintain the vascular supply to the osseous segments (5, 6, 7, 8, 9). The skin approach is through the classic dorsomedial linear incision. After incision of the superficial fascia, a limited dissection interval is developed between the superficial and deep fascia along the dorsomedial first metatarsal. The capsular and periosteal incision is curvilinear and commences over the proximal third of the metatarsal in line with the medial margin of the extensor hallucis longus tendon. It then curves medial to the level of the metatarsal insertion of the medial collateral ligamentous complex and ends in the midline dorsally on the phalangeal base. The periosteal-capsular plane is raised medially to expose the metatarsal. Care is taken to preserve the integrity of the capsular tissues for subsequent closure.
The tissues in the first intermetatarsal space may then be released, and the medial eminence of the metatarsal head is resected. We have often employed a percutaneous approach for the former maneuver. A 0.045-inch Kirschner wire is positioned at the anticipated apex of the offset-V osteotomy as an axis guide and is oriented to accomplish the desired displacement plane of the distal fragment. Factors that influence pin orientation include relative length of the first metatarsal, metatarsus primus elevatus, sub-second metatarsalgia, and PASA deviation.
The geometry of the offset-V osteotomy varies depending on the size and shape of the metatarsal and the magnitude of the deformity. The typical divergence of the wings of the osteotomy is 40 to 45 degrees. The length of the dorsal wing depends on the size of the metatarsal and the degree of PASA to be addressed, but it usually extends 50% to 75% of the length of the bone. Significant swivel of the capital fragment requires a shorter dorsal cut to prevent the juxtaposition of the proximal wing against the second metatarsal.
The legs of the offset-V osteotomy are scored onto the medial metatarsal with the saw blade directed perpendicular to the osseous surface. The dorsal cut is accomplished first and begins distally. This maneuver facilitates the saw blade orientation through the medial cortex in line with the axis guide. Stability afforded by the intact plantar leg facilitates completion of the longer proximal wing. After completion of the plantar cut, a lateral shift of the capital fragment frequently occurs spontaneously. Distal traction on the hallux creates gapping across the entire osteotomy and confirms that the osteotomy is complete.
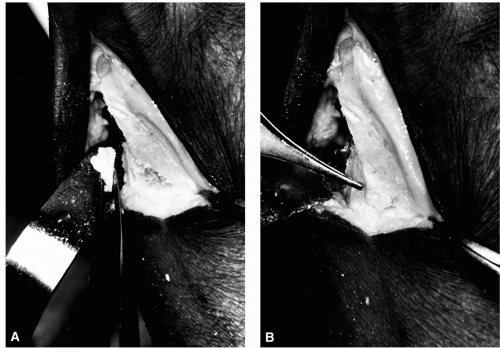
Lateral translation of the capital fragment reduces the intermetatarsal angle and is facilitated by placing a curved mosquito hemostat proximal to the apex of the osteotomy into the first metatarsal interspace just lateral to the extensor hallucis longus tendon. The tip of the instrument engages the lateral cortex of the proximal segment. The hallux is distracted, and the capital fragment is forced laterally with direct pressure while the hemostat pushes the proximal metatarsal fragment medially (Fig. 2). Resistance to shift most commonly is the result of incomplete transection of the metatarsal
at either the proximal cortex of the dorsal wing or the osteotomy apex distally. Occasionally, a significantly displaced fibular sesamoid may act as an obstacle to lateral transposition and requires blunt manipulation with the aid of the hemostat. The typical amount of lateral translation approaches 50% to 75% of the shaft width (Fig. 3).
at either the proximal cortex of the dorsal wing or the osteotomy apex distally. Occasionally, a significantly displaced fibular sesamoid may act as an obstacle to lateral transposition and requires blunt manipulation with the aid of the hemostat. The typical amount of lateral translation approaches 50% to 75% of the shaft width (Fig. 3).
 FIG. 3. A: Preoperative radiograph of a 63-year-old woman with hallux abducto valgus and metatarsus primus varus. The intermetatarsal angle is 18 degrees. B: Postoperative appearance. |
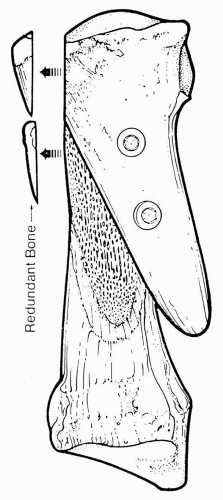
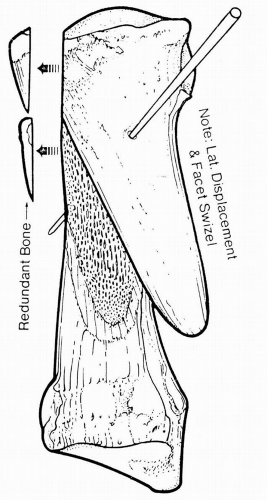 FIG. 4. After lateral transposition, one may swivel the capital fragment to achieve reduction of the proximal articular set angle. Resection of any redundant bone medially may then be accomplished. |
After lateral displacement, the distal fragment may be rotated to effect reduction of the PASA. The hemostat is repositioned medial to the proximal portion of the dorsal wing and lateral to the lateral cortical wall of the proximal fragment. This serves as a fulcrum around which the swivel maneuver may be used to correct the proximal articular set angle (Figs. 4 and 5). The cancellous substance of the metatarsal head is impacted medially into the medullary canal of the shaft as the pivot occurs around the lateral cortical apex spike of the proximal segment. “Troughing” is possible with this maneuver because of the cortical location of the procedure. The orientation of the osteotomy dictates that the capital fragment plantarflex should troughing develop. This added plantarflexion of the metatarsal may be beneficial in reducing lesser metatarsalgia. This is in contrast to iatrogenic primus elevatus that can occur with “troughing” in the Scarf Z-procedure (10,11).
The redundant medial cortical overhang is then resected. This triangular fragment may be reversed from anterior to posterior and may be inserted as a wedge into the intramedullary canal between the remaining medial cortex of the proximal fragment and the medial border of the dorsal wing of the capital fragment (Fig. 6). This serves as an autogenous bone graft to enhance healing and fills the void in the medullary canal.
 FIG. 5. Note the swivel of the capital fragment in this patient to address the deviated proximal articular set angle. |
Osteosynthesis is then accomplished. In patients with high intermetatarsal angles and PASA components, the reduced bone contact may limit the fixation to one obliquely driven Kirschner wire. When the displacement contact area is sufficient, two cortical screws are commonly used for fixation (Fig. 7). One well-positioned 0.062-inch Kirschner wire provides stable fixation for this osteotomy even in the presence of significant displacement and limited bony contact (Fig. 8). Experimental study has demonstrated the importance of the pin orientation. Enhanced stability can be achieved by delivering fixation from dorsal proximal medial to plantar distal lateral, crossing the plantar wing of the osteotomy (12,13). The pin may be left percutaneously or used as temporary fixation while screws are inserted.
Closure is accomplished in layered fashion and may be enhanced with two to three obliquely oriented “load sutures” in the capsule using 2-0 absorbable suture incorporating the thickened medial capsule and medial collateral ligament. These load sutures are directed obliquely from plantar distal to proximal dorsal. The hallux is held in corrected alignment with slight adduction and plantarflexion at metatarsophalangeal joint level.
A compression bandage is applied, and the patient is allowed to bear weight with either a surgical shoe or a slipper cast, depending on the surgeon’s preference. Immobilization varies from 4 to 6 weeks, depending on the magnitude of osseous displacement and other patient factors. Early active and passive range-of-motion exercises are encouraged, to maintain first metatarsophalangeal joint flexibility during the immediate postsurgical phase, although bandaging impedes this process to some extent. After cast or bandage removal, the patient may resume wearing closed shoes as tolerated. Most commonly, a supportive athletic style shoe is initially employed until postoperative swelling is reduced and joint mobility is restored. Serial radiographs are used to monitor consolidation and remodeling. Generally, no significant external bone callus develops other than along the proximal aspect of the dorsal wing segment. The displaced lateral wing undergoes remodeling with resorption, blunting, and new bone formation. This process is complete at about 8 months postoperatively and provides a more rectus first ray appearance radiographically.
COMPLICATIONS
The procedure has proven to be predictable and rewarding in resolving painful hallux valgus conditions associated with moderate to severe deformity. Age presents no barrier to the performance of this procedure, provided the patient’s circulatory status is sufficient. Reduced bone stock or poor quality can result in telescoping and additional shortening of the first ray segment. As with all reconstructive procedures for hallux abducto valgus, patients may experience some reduction in the total range of motion of the first metatarsophalangeal joint.
Significant PASA correction accomplished with the swivel maneuver performed along a plantar laterally declinated axis guide plane produces apparent elevatus of the metatarsal head with plantar migration of the dorsal wing. Although this condition presents more of an adverse radiographic appearance than a functional detriment, this situation is generally avoided. Infrequently, a synostosis may develop between the second metatarsal and the dorsal wing, without causing subjective complaints or any untoward clinical consequences (Fig. 9).
REFERENCES
1. Ludloff K. Die Beseitigung des hallux valgus durch die schraege plantodorsale Osteotomie des Metatarsus. I. Arch Klin Chir 1918;110: 364-387.
2. Vogler HW. Shaft osteotomy in hallux valgus reduction. Clin Podiatr Med Surg 1989;6:47-69.
3. Vogler HW. The “off-set V” osteotomy in hallux valgus reduction. In: Six schools of surgical thought (syllabus). Cleveland: Ohio College of Podiatric Medicine, 1985.
4. Vogler HW. The “off-set V” osteotomy in hallux valgus reduction. In: Jay R, ed. Current therapy in podiatric surgery. Toronto: BC Decker, 1988:158-161.
5. Rhinelander FW. Vascular proliferation and blood supply during fracture healing. In: Uhthoff H, Stahl E, eds. Current concepts of internal fixation of fractures. Berlin: Springer-Verlag, 1980:9.
6. Rhinelander FW, Stewart CL, Wilson JW, et al. Blood supply to developing, mature and healing bone. Clin Orthop 1982;164:293-305.
7. Shereff MJ, Yang OM, Kummer FJ. Extraosseous and intraosseous arterial supply to the first metatarsophalangeal joint. Foot Ankle 1987; 8:81-93.
8. Resch S, Stenstrom A, Gustafson T. Circulatory disturbance of the first metatarsal head after chevron osteotomy as shown by scintigraphy. Foot Ankle 1992;13:137-142.
9. Johnston K, Feiwell LA, Freedman EL, et al. The effect of chevron osteotomy with lateral capsular release on the blood supply to the first metatarsal head. J Bone Joint Surg Am 1995;77:197-204.
10. Zygmunt KH, Gudas CJ, Laros GS. Z-bunionectomy with internal screw fixation. J Am Podiatr Med Assoc 1989;79:322-329.
11. Meyer M. Eine neue Modifikation der hallux valgus Operation. Zentralbl Chir 1926;53:3215-3268.
12. Gonda E, Bauer GR, Hillstrom HJ, et al. Stability of the offset V osteotomy: test jig development and saw bone model assessment. J Am Podiatr Med Assoc (submitted).
13. Dalton SK, Bauer GR, Lamm BM, et al. Stability of the offset V osteotomy: effects of fixation and surgical translocation in saw bone and preserved cadaver specimens. Presented at the 57th American College of Foot and Ankle Surgeons symposium, 1999.
PART 2 Scarf Z-Osteotomy
Charles J. Gudas
HISTORICAL REVIEW
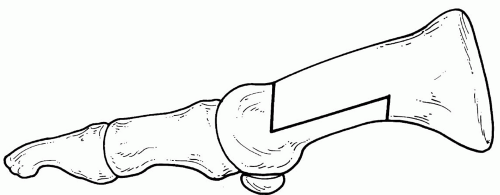
As surgeons became interested in reevaluating osteotomies of the first metatarsal shaft for the repair of hallux abducto valgus deformity, Zygmunt and Gudas devised a procedure that become known as the Scarf osteotomy. A similarly configured osteotomy had been previously described by Meyer, but with the bone cuts performed in the sagittal versus the transverse plane (1). Like the Mau procedure, the Scarf osteotomy, which is also known as the Zosteotomy, is performed in the midshaft of the first metatarsal. However, the Scarf procedure is inherently more stable than the Mau procedure because of the interlocking segments at each end of the osteotomy that allow for early postoperative weight bearing (Fig. 10). Various modifications of the Scarf osteotomy were offered shortly after the procedure became popular, so some form of this procedure is commonly employed for the repair of hallux abducto valgus.
INDICATIONS
Initially, investigators believed that the Z-osteotomy would be well suited for the repair of hallux abducto valgus deformities with mild to moderate intermetatarsal angles. Some authors noted that this would offer the surgeon the opportunity for an “in between” procedure for those patients whose metatarsus primus adductus deformities were believed to be too great for an Austin or capital osteotomy, yet one desired to avoid the non-weight-bearing protocol required with a base wedge procedure (2). However, as with the capital osteotomies, time and experience have demonstrated that the Scarf procedure may be employed for patients with larger intermetatarsal angles than had initially been appreciated (3). One may also obtain simultaneous correction of a deviated proximal articular set angle by derotating the capital fragment. However, this maneuver tends to counteract and limit the reduction of the intermetatarsal angle that is attained (4). Patients who have a first metatarsal of average or greater width also seem to derive greater potential benefit from this procedure, especially when larger intermetatarsal angles are encountered.
The Scarf procedure has also been advocated for patients with a short first metatarsal based on the premise that little if any shortening occurs with the osteotomy (5). However, shortening occurs with most any procedure that transects the bone, so preservation of metatarsal length should not be considered a unique property of the procedure. However, as with the capital osteotomies, the axis of the Z-osteotomy can be modified to lengthen or shorten the first metatarsal when required.
CONTRAINDICATIONS
Because of the complexity and length of the osteotomy, these procedures are best employed in patients with good bone quality and without significant osteopenia (4). In patients with reduced bone quality, the ability to stabilize the osteotomy adequately after rotation or transposition is limited. Surgeons may also want to exercise care when they contemplate performing the procedure in obese patients if these patients are to be fully weight bearing postoperatively.
SURGICAL CONSIDERATIONS
Surgical Technique
The incision is generally placed over the medial or dorsomedial aspect of the first ray, and it extends from the midshaft or proximal region of the first metatarsal to the base of the proximal phalanx of the hallux. Dissection within the interspace and the medial exposure of the metatarsal head is conducted as preferred by the surgeon. The periosteum needs to be incised along the course of the incision, with a greater length usually required for reduction of larger intermetatarsal angles. The periosteum needs to be freed from the metatarsal to execute the osteotomy and to provide adequate visualization for the fixation process. The medial eminence may be removed before or after the osteotomy, and this segment of bone may be used as a subsequent graft for a variety of purposes.
The osteotomy consists of a longitudinal cut through the midshaft of the first metatarsal with additional cuts proximally and distally to transect the plantar and dorsal cortices, respectively. The horizontal portion of the osteotomy typically measures 3 to 4 cm. This cut is placed at the junction of the upper two-thirds of the first metatarsal and the lower one-third of the first metatarsal to provide a stronger dorsal wing to resist weight-bearing forces. A sharp, thin, broad saw blade is preferred for the horizontal cut, which is initiated
from medially to laterally, and it may be directed slightly plantarward to enhance the weight-bearing position of the metatarsal postoperatively. The distal and proximal cuts of the Z-osteotomy are made 60 to 80 degrees from the perpendicular (Fig. 11). Care should be taken so the distal and proximal cuts do not extend beyond the longitudinal osteotomy of the metatarsal shaft; otherwise, the bone will be weakened, possibly leading to later stress fracture. One way to help prevent this overcutting of the bone is to use a small osteotome to perform the final portion of the transection.
from medially to laterally, and it may be directed slightly plantarward to enhance the weight-bearing position of the metatarsal postoperatively. The distal and proximal cuts of the Z-osteotomy are made 60 to 80 degrees from the perpendicular (Fig. 11). Care should be taken so the distal and proximal cuts do not extend beyond the longitudinal osteotomy of the metatarsal shaft; otherwise, the bone will be weakened, possibly leading to later stress fracture. One way to help prevent this overcutting of the bone is to use a small osteotome to perform the final portion of the transection.
Although not required, axis guides, which are typically smooth Kirschner wires (K-wires), may help the surgeon to perform this procedure with greater precision (5,6) (Fig. 12). This may be particularly helpful when attempting to alter either the sagittal plane alignment or length of the first metatarsal with transposition of the osteotomy. As with other procedures, altering the plane of the osteotomy may help the surgeon to accomplish the change in position of the first metatarsal that is desired. However, transposition will be more difficult if the proximal and distal cuts are oriented perpendicular to the first metatarsal or if lengthening is attempted.
Translocation of the osteotomy may be facilitated by distracting the hallux and employing a small osteotome to free up any remaining osseous attachments plantar laterally. The capital fragment is displaced approximately one-third of the width of the metatarsal shaft and is initially stabilized with a bone clamp. Intraoperative radiographs may be used at this point to assess the osteotomy and the degree of correction. Furthermore, one should note whether the distal aspect of the osteotomy is approximated, because the juxtaposition at this level enhances overall stability. The osteotomy may also be pivoted to reduce deviation of the proximal articular set angle (Fig. 13). The medial corticocancellous overhang is removed with a sharp bone saw and may be used as a graft.
Fixation
Satisfactory stabilization of the osteotomy may be performed with various devices including screws (2,4,5,7,8), threaded K-wires (6,9), smooth K-wires (10), and absorbable pins (11). Two fixation devices are preferred to provide the best stability with the longer form of the osteotomy (Fig. 14). However, shorter forms of the Z-osteotomy may be adequately stabilized with only one fixation device (10,12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree