Osteochondritis Dissecans of The Knee and Articular Cartilage Fractures
Alberto Gobbi
Massimo Berruto
Giuseppe Filardo
Elizaveta Kon
Georgios Karnatzikos
Osteochondritis dissecans (OCD) is a disorder of one or more ossification centers, characterized by sequential degeneration or aseptic necrosis and recalcification. An OCD lesion involves both bone and cartilage but appears to affect the subchondral bone primarily and the articular cartilage secondarily.
The condition was first described by Ambrosio Pare’ and was named by Franz König (1) in 1888 describing it as a knee subchondral inflammatory process, resulting in a loose fragment of cartilage from the femoral condyle. Incidence of OCD has been stated to be between 0.02% and 0.03% on radiographs and 1.2% on arthroscopy (2). Linden (3) stated the incidence of OCD in Sweden, between 15 and 21 cases per 100,000. It most commonly occurs in patients aged 10 to 15 years, with a male-to-female ratio of 2:1 and occurs bilaterally (4) in 15% to 30%.
ETIOLOGY
The pathogenesis of OCD is still controversial: various theories have been proposed throughout the years but no theory is markedly superior over the other.
Theories can be divided into three major groups: genetic, vascular, and traumatic.
Genetic theory shows variation or subgroup of epiphyseal dysplasia and thus may display a similar inheritance pattern.
OCD has been found with a variety of inherited conditions, including dwarfism, tibia vara, Legg-Calvé-Perthes disease, Stickler syndrome (5, 6, 7, 8 and 9) and that there is a familial predisposition to the occurrence of OCD in other joints.
Other authors (10, 11 and 12) have suggested a vascular etiology with the occurrence of a vascular event such as embolism, thrombosis, or venous stasis, which can cause a secondary osteonecrosis; however, others (13) have demonstrated that the presence of an abundant vascularization does not end at the femoral epiphysis, which refuted the vascular etiology.
The traumatic etiology (14, 15 and 16) is by far the oldest and the most well established and is based on clinical history of previous trauma, predominantly affecting men, and the probability of reproducing similar lesions in other parts of the body.
According to the theory of repeated microtrauma, as described by Fairbank (17) and validated by Smillie (18) in the 1960s, the OCD is caused by contact of a hypertrophied tibial spine on the medial femoral condyle. This theory, despite being the most credited, does not allow an explanation of the localization of the disease in different locations of the knee. Nowadays, repetitive microtrauma correlated with a possible vascular insufficiency and other inherited factors are still under investigation.
OCD CLASSIFICATION
There are several types of classifications of OCD that is based on the following:
Age of onset of the disease
Radiographic localization
Patho-anatomy
Arthroscopic evaluation
Age of Onset
Smillie (18) distinguished two forms of OCD, juvenile and adult, and suggested unique etiologies.
The juvenile form OCD was supposed to be related to a disturbance of the epiphyseal development, whereas in the adult a more direct traumatic causation was supposed. Other authors (19) suggested a distinction based on the osseous age of the patient at the time of symptom onset: juvenile OCD, which affects patients with open growth of cartilage in a general age group of between 10 and 16 years, and OCD in adults, when the cartilage physis is closed.
Radiographic Localization
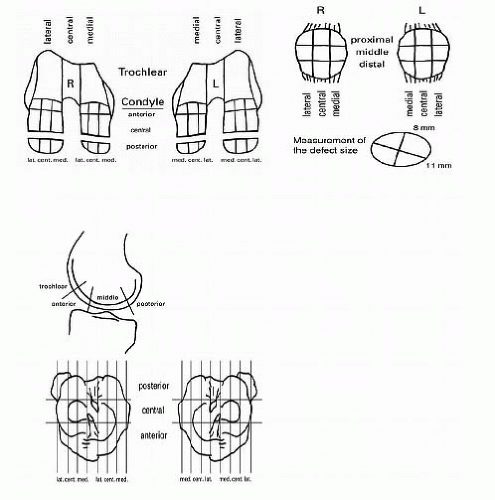
The location of OCD can be defined topographically on standard radiographic projections of the knee (19). In the anteroposterior view, it is typically located centrally on the medial condyle, whereas on the lateral view, it is most commonly in the anterior or middle segments (Fig. 64.1).
Anatomo-pathologic Classification
Proposed by Conway and subsequently amended by Guhl (20), this classification, which was useful in the past to address the type of treatment, taking into account the anatomical characteristics of the lesion and subdivided into five stages:
Stage I: Lesion evident at radiography, the CT or the MRI, with the presence of a sclerotic line, cartilage intact, and, only in some cases, slightly softened but only in some points.
Stages II and III: Cartilage not intact, with the presence of fissures and fragments in situ or partially detached.
Stage IV: Complete detachment but normal joint.
Stage V: The fragment is displaced and there are findings of degenerative cartilage damage.
Classification by Arthroscopy
Recently, the board of the International Cartilage Repair Society (ICRS) (21) defined a classification of OCD arthroscopy in four stages:
Stage I: Stable lesion with a continuous but softened area covered by intact articular cartilage.
Stage II: Lesion with partial articular cartilage discontinuity but stable when probed.
Stage III: Lesion with an unstable but not dislocated fragment “dead in situ.”
Stage IV: Empty defect with a dislocated fragment (loose body).
CLINICAL EVALUATION
Juveniles and adolescents will complain of vague, nonspecific, poorly localized anterior knee pain with variable intermittent amount of swelling, locking of the knee, grinding, or catching; pain is aggravated by activity and relieved by rest (22). While others may be asymptomatic, a high level of suspicion should be exhibited with these type of symptoms. Symptoms are usually preceded by trauma in 40% to 60% of the cases (15, 23). Others may present with Wilsons (24) sign, which is performed by flexing the knee to 90° then slowly internally rotating the leg and extending it. Patients will complain of pain at 30° of flexion, and the pain is relieved by external rotation. Pain is exhibited because the tibial spine impinges on the medial femoral condyle. This test, albeit unreliable, has been shown to have an accuracy of only 70% (2, 25).
Radiographic Evaluation
The radiographic examination of a patient suspected to have OCD should always begins with plain radiographs. Standard request should be an anteroposterior, lateral, notch, and Merchant view of the knee. Notch view is specifically recommended because it demonstrates the most common areas for the occurrence of OCD, and it increases the percentage of detection. Classic findings of OCD on plain film are a well-circumscribed area of subchondral bone, separated by a crescent shaped sclerotic radiolucent outline of the OCD fragment (14, 25). In pediatric patients and adolescents, contralateral views should be requested to avoid confusion with the growth plates. Plain radiographs, however, cannot visualize for us the stability and status of the overlying cartilage; hence, additional diagnostic procedures may be necessary for us to treat these lesions.
CT Scan
The use of the CT scan has fallen out of favor with the advent of the MRI because the MRI gives a more detailed picture of the disease entity. CT scanning is helpful in determining lesion size and loose bodies but is rarely used nowadays as part of the treatment strategy.
Scintigraphy
Technetium bone scans have been previously used to localize the lesion of a specific joint and follow the progression of healing in juvenile patients. This imaging modality provides no information on the status of the cartilage and has been replaced by MRI. Some authors have proposed serial bone scanning of juvenile patients (but have not been widely adopted due to the time required for the study, invasive venous access, and the risk of introducing a radioactive isotope).
Magnetic Resonance Imaging
MRI has proven superior in providing valuable information as compared with other diagnostic modalities.
It generally gives us the dimensions of the lesion, as well as the status of the cartilage and subchondral bone. The most appropriate MRI protocol for evaluating OCD lesions is fast spin echo, proton density, and T2-weighted image (25). MRI-arthrography with gadolinium has been shown to have 100% accuracy, determining the status of articular cartilage using gradient echo techniques (26).
It generally gives us the dimensions of the lesion, as well as the status of the cartilage and subchondral bone. The most appropriate MRI protocol for evaluating OCD lesions is fast spin echo, proton density, and T2-weighted image (25). MRI-arthrography with gadolinium has been shown to have 100% accuracy, determining the status of articular cartilage using gradient echo techniques (26).
TREATMENT
The advent of arthroscopy has outright revolutionized the treatment of OCD. Using standard arthroscopic portals and techniques, surgeons are now visualizing lesions previously missed on standard diagnostic procedures. Open techniques have not fallen out of favor and are still utilized for lesions requiring greater exposure and visualization. Treatment options largely depend on age of the patient, lesion size, and stability. Unstable lesions must be treated surgically.
Nonoperative Treatment
Nonoperative treatment is still used in a select group of patients with OCD. The goal of nonsurgical treatment is to promote healing of lesions in situ and prevent lesion displacement. Skeletally, immature patients usually have a better prognosis. Lesions on weight-bearing surfaces and those that are greater than 1 cm in size have shown to have an unsuccessful outcome (15, 20, 27, 28). The mainstay of nonsurgical treatment has been cessation of athletic activity and lifestyle modification. This is done for a period of 3 to 6 months with an initial 6 to 8 weeks of nonweight bearing and daily range-of-motion exercises. If at the 6th month there are no signs of radiographic healing, then operative treatment should be considered (29, 30). A healing rate of 50% to 94% has been noted with nonoperative treatment (4, 19, 29).
Operative Treatment
Excision of Fragments
Previously considered the most common treatment for these lesions have fallen out of favor due to the dismal long-term results in juvenile and adult patients (31, 32, 33 and 34). The addition of a debridement and curettage of the lesion bed has shown to improve the results in juvenile patients (31, 35).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree