Chapter 14 Osteochondritis Dissecans
Background/aetiology
The most common ‘little leaguer elbow’ symptoms are on the medial side of the joint and are related to traction injury and inflammation of the medial collateral structures, especially the vulnerable medial epicondyle. Less frequently, symptoms are lateral and related to compressive overloading of the lateral bony structures, including the radial head and especially the capitellum. OCD and Panner’s disease are both seen in the capitellum and it is therefore important to define and distinguish these conditions (Table 14.1).
Table 14.1 Panner’s disease and osteochondritis dissecans
| Feature | Panner’s disease | Osteochondritis dissecans |
|---|---|---|
| Usual age | 10 years or less | Adolescent |
| Radiology | Capitellar sclerosis and fragmentation | Discreet capitellar change |
| Management | Usually non-operative | Non-operative and operative depending on grade |
| Prognosis | Relatively good | Variable |
Panner’s disease is considered to be an avascular necrosis of the developing capitellar ossification centre. It is characterized initially by radiological sclerosis and then fragmentation of the capitellum (Fig. 14.1), followed by gradual restoration. It is not necessarily associated with trauma.1,2 The process is very similar to the series of changes seen in the femoral epiphysis in Perthes’ disease. Panner’s disease occurs in the relatively young (under 10 years). Management is usually non-operative and primarily involves avoidance of the causative stress together with range-of-movement therapy to maintain extension. Although it may take some time for the radiological lesion to resolve, the prognosis is relatively good. As in Perthes’ disease, the capitellar cartilaginous anlagen, devoid of its supporting bony nucleus, can deform and sometimes reossifies into a flattened oval in the sagittal plane, ultimately limiting full extension.
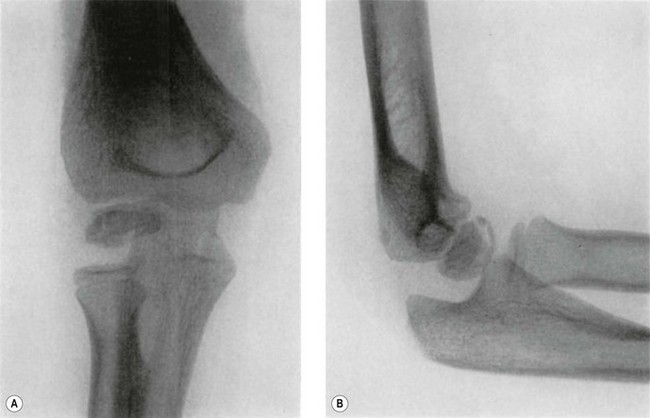
Figure 14.1 Panner’s disease. Sclerosis and fragmentation of the entire ossific nucleus of the capitellum.
From J Bone Joint Surg Am, April 1960; 42:513–516. Avascular necrosis of the capitellum humeri (Panner’s disease): a report of a case. Charles J. Heller and Leon L. Wiltse.
By contrast, OCD occurs most commonly in the adolescent age range. It is usually a more discreet condition, affecting a section of the subchondral bone and the overlying articular cartilage (Fig. 14.2). The pathology and radiology are similar to OCD seen in other joints such as the knee and ankle and there is potential for loose body formation. Management is sometimes operative and depends on the stability of the OCD lesion. Prognosis is accordingly variable and generally worse than Panner’s disease. Early recognition is important because appropriate early management can influence the prognosis.
The capitellum of the immature elbow has a tenuous vascular supply consisting of one or two posterior vessels that traverse the capitellar cartilage before entering the epiphysis. There is no metaphyseal blood supply until the physis closes at maturity.3 This tenuous circulation makes the capitellum vulnerable to avascular necrosis following lateral condyle fractures and it is postulated that it may also play a role in the genesis of Panner’s disease and OCD. Some reports suggest a genetic predisposition in some families but most evidence supports the hypothesis of repeated shear and compressive trauma, particularly in relation to OCD.
Investigation and classification
Evaluation should not overlook other potential explanations for pain. Investigation usually commences with standard anteroposterior and lateral plain radiography. The typical early appearance of OCD is anterolateral radiolucency within the capitellum, with flattening progressing to irregularity of the central or anterolateral articular surface. A separated fragment can subsequently form and either remain in its bed or become detached, forming a loose body. Radiographic findings can be classified into three grades (Fig. 14.2).4 Grade I is localized flattening or radiolucency. Grade II is an undisplaced fragment and grade III a displaced or detached fragment. Reliable grading is, however, difficult and subject to inter-observer variation.
Furthermore, plain radiography lacks sensitivity. Early grade I changes are difficult to visualize and early lesions can be easily overlooked. One study has shown that only 7 of 15 known cases of early OCD were identified with plain radiographs.5 As a result, some authors recommend supplementing the standard films with an anteroposterior view of the elbow when it is flexed to 45° to give a tangential view of the anterolateral capitellum, where the lesion is most typically located.6 Magnetic resonance imaging (MRI) is more sensitive than plain radiography and should therefore be utilized if the history and examination suggest OCD as a possible differential diagnosis.
Classification of the lesion is critical because current management guidelines are dependent on the type of lesion present and particularly on its stability. In an effort to standardize the classification of OCD lesions, the International Cartilage Repair Society (ICRS) has published a system for clinical cartilage evaluation and imaging assessment (Table 14.2).7 Prognosis deteriorates from OCD I to OCD IV. Determining the stability of the lesion is the critical issue. More stable lesions have a better prognosis and can sometimes heal completely with non-operative treatment. Unstable lesions have little or no chance of healing with non-operative management and require surgical treatment.
Table 14.2 ICRS classification of OCD
| International Cartilage Repair Society (ICRS) | Arthroscopic OCD lesion classification |
|---|---|
| OCD I | Lesion with a continuous but softened area covered by intact cartilage. Stable when probed |
| OCD II | Lesion with partial discontinuity of articular surface but stable when probed |
| OCD III | Complete discontinuity of articular surface but fragment not yet dislocated (‘dead in situ’) |
| OCD IV | Empty defect with loose fragment in joint or loose within bed |
| Subgroups I–IVa <10 mm in depth Subgroups I–IVb >10 mm in depth |
From Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am April 2003; 85:58–69.
By comparison with plain radiography MRI is sensitive and can accurately define the site and extent of OCD lesions. MRI assessment of stability is, however, more difficult and controversial. Some authors have suggested that unstable lesions are surrounded by a rim of high signal intensity or a fluid-filled cyst on T2-weighted images.5 Other studies have demonstrated that such high signal deep to the OCD fragment merely represents granulation tissue and the determination of instability can only be certain if a break in the articular surface is also demonstrated.8 MR arthrography, which can identify an articular surface breach more precisely, is therefore sometimes used to improve the accuracy of MR assessment.9 There is also emerging evidence that ultrasonography is a potentially useful imaging modality to evaluate OCD lesions and their stability, but interpretation requires considerable operator experience.10 Currently therefore surgical visualization and probing of the lesion, either by arthroscopy or arthrotomy, remains the gold standard for the assessment of OCD lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









