Chapter 14 Osteochondral Lesions of the Talus and Occult Fractures of the Foot and Ankle
Occult Fractures of the Hindfoot
Pertinent anatomy
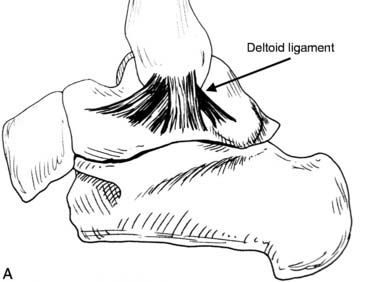
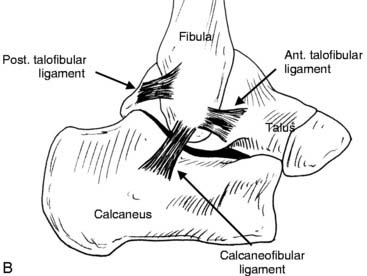
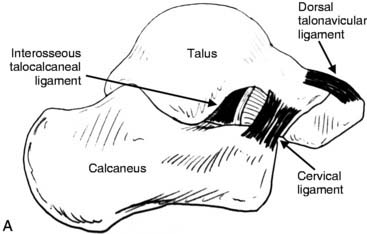
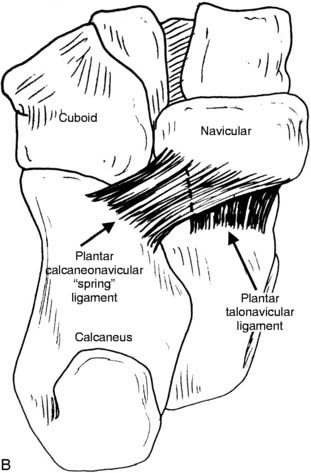
With 28 bones, multiple joints, and connecting ligaments, the foot and ankle are vulnerable to compression and avulsion injuries with many complex movements during competitive sports. The bones comprising the hindfoot are the tibia, fibula, talus, calcaneus, navicular, and cuboid. The talus is especially prone to injury because it is involved in both dorsiflexion/plantarflexion and inversion/eversion motions. The talus is connected at the ankle joint to the tibia medially through the deltoid ligament (Fig. 14-1, A) and to the fibula laterally through the anterior talofibular ligament and posterior talofibular ligament (Fig. 14-1, B). The talus is connected to the calcaneus by the talocalcaneal interosseous ligament and the cervical ligament (Fig. 14-2, A). Thedorsal (see Fig. 14-2, A) and plantar (Fig. 14-2, B) talonavicular ligaments connect the talus and navicular.
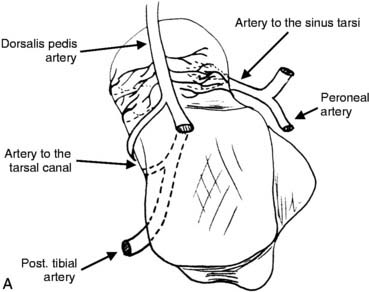
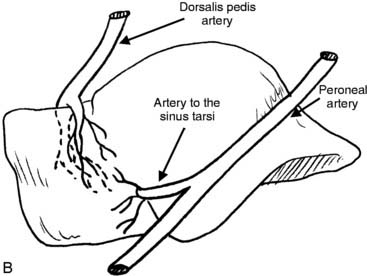
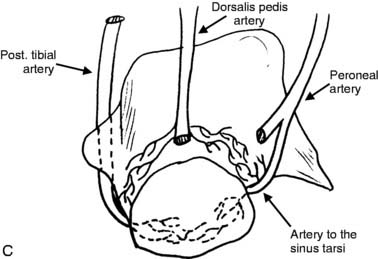
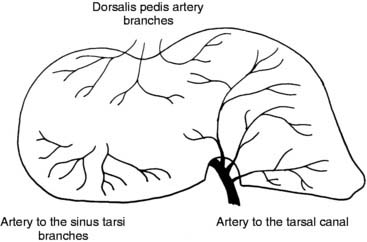
The talus is unique in that it has no direct muscular attachments. Approximately 60% to 70% of the talar surface is articular1,2 with the ankle joint superiorly, the talonavicular joint anteriorly, and the subtalar joint inferiorly. Blood supply to the talus therefore is limited,1,3 coming from its ligamentous attachments and a leash of vessels surrounding the talar neck that receive contributions from the artery to the tarsal canal medially, the dorsalis pedis artery anteriorly, and the artery to the sinus tarsi laterally (Fig. 14-3, A through C). The internal vasculature of the talus varies considerably4 (Fig. 14-4). External athletic injuries to the talus that involve disruption of the vascular leash or the ligamentous attachments often produce vascular insult to the talar body or talar neck and may produce talar fractures or compression injuries that heal slowly or do not heal.
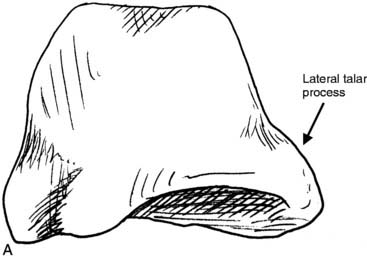
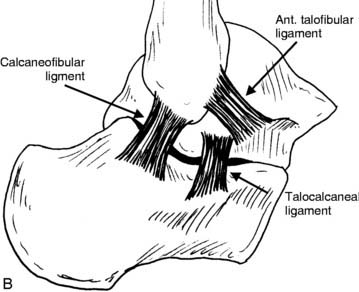
The lateral process of the talus is a wide, triangular-shaped process that slopes down to meet the lateral calcaneus (see Fig. 14-5, A). On the lateral view it is wedge-shaped and articulates superiorly with the fibular surface and inferiorly with the calcaneus (see Fig. 14-5, A). The lateral talocalcaneal ligament attaches to the lateral process (Fig. 14-5, B).
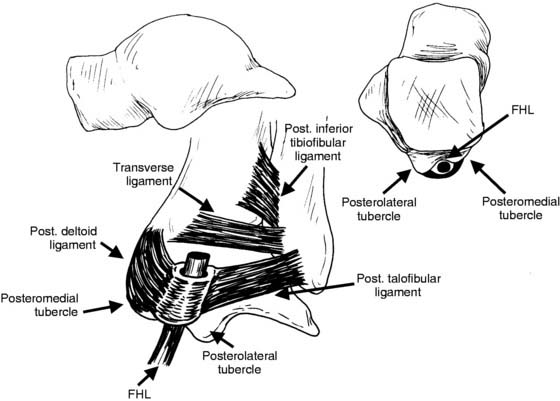
The posterior process of the talus originates from the convex-curved posterior half of the talar dome and slopes down and back to form the posterior talar “beak.” Inferiorly, it is concave and articulates with the posterior subtalar facet of the calcaneus. The posterior process has both a posteromedial tubercle and posterolateral tubercle. In between lies the flexor hallucis longus, which is commonly involved in posterior talar injuries (Fig. 14-6). This posterior process is widely variable in shape, from a short, rounded end to a long “beak” that is prone to injury.
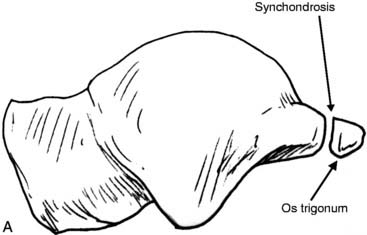
The posterolateral tubercle (Stieda’s process) is larger than the posteromedial tubercle. In approximately 7% to 10% of humans a separate os trigonum may exist—connected to the posterolateral tubercle by a fibrous cartilaginous synchondrosis (Fig. 14-7, A and B). The posterior talofibular ligament attaches the fibula to the posterolateral tubercle or the os trigonum (see Fig. 14-7, B). The posterior deltoid or posterior talotibial ligament attaches the posterior tibia to the posteromedial tubercle of the talus. The Y-shaped transverse or bifurcate ligament is a thickening in the posterior ankle capsule that holds the two tubercles together and restrains the flexor hallucis longus. A meniscus-like “marsupial meniscus” also often exists in the posterior ankle superior to the posterior process of the talus (Fig. 14-8).
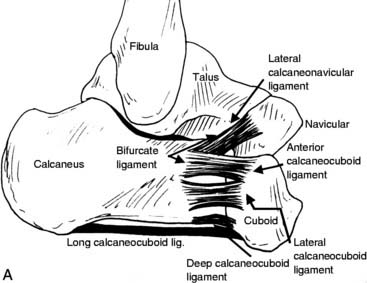
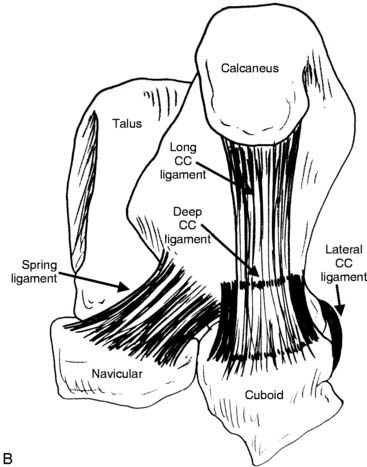
The blood supply to the calcaneus is quite robust, and fractures of the calcaneus tend to heal more easily. The ligamentous attachments at the calcaneus are the talocalcaneal interosseous ligament, lateral talocalcaneal ligament and cervical ligament to the talus and the calcaneofibular ligament laterally (Fig. 14-9). The posterior, lateral, and anterior calcaneocuboid ligaments and the plantar calcaneonavicular (spring ligament) and lateral calcaneonavicular ligaments connect the calcaneus anteriorly to the cuboid and navicular, respectively.
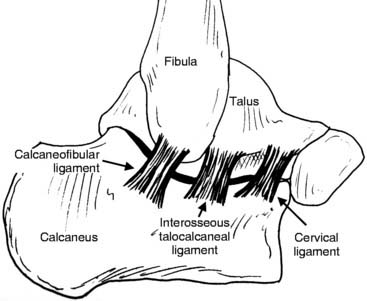
Figure 14-9 Calcaneal ligaments. Note laterally the calcaneofibular, cervical, and lateral talocalcaneal ligaments.
The strong plantar calcaneonavicular or “spring” ligaments acts as a “sling” to hold the talar head in place. The bifurcate ligament (Y-ligament) is composed of the anterior and lateral calcaneocuboid ligament (Fig. 14-10, A and B) and is commonly injured during “sprain-type” inversion injuries, producing an avulsion fracture at the anterolateral process of the calcaneus. Inversion/adduction injuries of the midfoot also may produce avulsion fractures at the base of the cuboid.
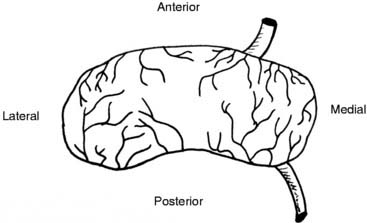
The saddle-shaped cuboid articulates with the anterior process of the calcaneus and may be involved in either compression or avulsion tension-type injuries. The tarsal navicular is a “C” or saucer-shaped bone articulating with the talus posteriorly and the cuboid laterally. The dorsal talonavicular ligament and capsule may produce avulsion injuries of the navicular from plantarflexion-type injuries. Compression-type injuries also may be produced by the impact of the talar head on the navicular. The blood supply to the midportion of the navicular is poor (Fig. 14-11) and may contribute to delayed healing or nonunion of such fractures. The articulation between the cuboid and the navicular varies from a true articulating joint to a fibrous connection to a bony bridge (tarsal coalition).
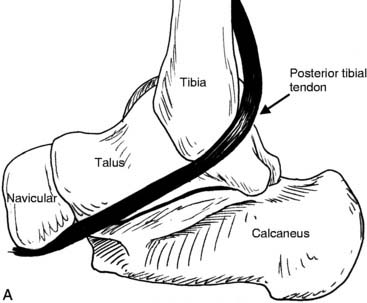
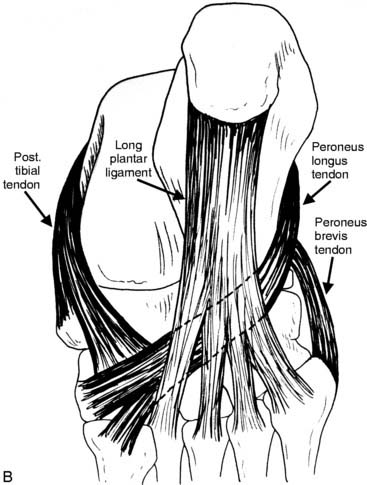
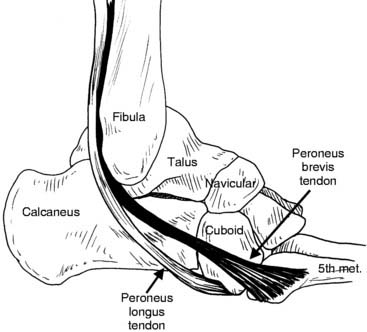
Various important and powerful tendons attach to the hindfoot; these produce considerable forces during athletic activities and can create injuries. The posterior tibial tendon attaches to the navicular (Fig. 14-12, A and B), producing inversion/supination and adduction while elevating the arch. It fires twice during each gait cycle or step—both eccentrically as a shock absorber and concentrically during push-off. The anterior tibial tendon, with attachments to the cuneiform and first metatarsal, is the primary dorsiflexor for the ankle and also inverts the foot. It also fires eccentrically during heel strike to decelerate and cushion the landing foot. The peroneus brevis and longus tendons (Fig. 14-13) both evert the foot and ankle and resist inversion injuries. The peroneus brevis attaches to the base of the fifth metatarsal. The peroneus longus wraps around the cuboid at the trochlea to insert broadly underneath the foot near the base of the first metatarsal, which allows the longus also to help plantarflex and stabilize the medial foot.
Talonavicular Avulsion Injuries
Incidence and mechanism
Avulsion fractures involving the tarsal navicular or talar head are not unusual after a plantarflexion injury of the ankle (Fig. 14-14). The dorsal talonavicular capsule or ligament pulls off a small fragment with this injury (see Fig. 14-14). This injury is more common than thought, because many occur and are not treated immediately. They are seen in practices such as mine years later, asymptomatic with x-ray findings on films taken for an unrelated injury. Many of these minor fractures heal untreated by either painless bony or fibrous nonunion. However, a painful nonunion also may occur. Bony union of the fracture can result in the athlete’s having pain from a bony prominence over the joint (Fig. 14-15) or painful arthritis of the talonavicular joint.

Figure 14-14 Fracture of navicular caused by plantarflexion of foot and ankle with avulsion of dorsal fragment.

Figure 14-15 Nonunion of dorsal navicular avulsion fracture. This can cause a dorsal prominence and pain in the athlete.
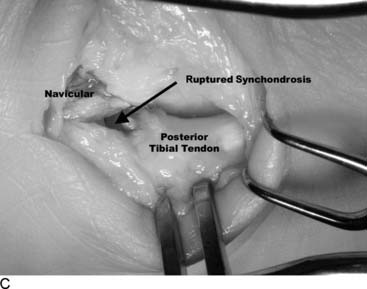
An avulsion fracture from the medial or proximal end of the tarsal navicular at the distal insertion of the posterior tibial tendon is less common in athletics. This injury occurs in running sports in which a sudden change of direction is common. The athlete plants the foot, decelerates, and twists a plantarflexed foot to reaccelerate and push off. The force of the posterior tibial tendon on the navicular may produce an avulsion at its insertion. In cases in which the athlete has a congenital accessory navicular, the injury may occur through the cartilaginous synchondrosis between the main and “extra” (or accessory) bone (Fig. 14-16).
Diagnosis
With dorsal navicular avulsion fractures, the athlete complains of anterior “ankle” pain after a sprain-type injury. In acute cases, ecchymosis may exist over the anterior ankle. Point tenderness will be noted over the dorsum of the navicular (Fig. 14-17) or the talar head. Inversion or eversion may produce pain and plantarflexion of the foot. In chronic cases, a firm, bony “lump” (tender or nontender) will be noted over the dorsal navicular or talar head.
Imaging
X-rays usually will show a wafer-like avulsion fracture on the dorsum of the navicular or talar head (Fig. 14-18). In chronic cases, x-ray may show a rounded-off nonunion of the fragment or a healed, bony, beak-like projection, often with some arthritic changes in the dorsal talonavicular joint (Fig. 14-19). More involved navicular body fractures also occur in the athlete but are not common. These larger body fractures require a computed tomography (CT) scan with axial and lateral views (Figs. 14-20 and 14-21) to assess joint alignment and fracture orientation for surgical decision making. A CT scan also is helpful in chronic cases for assessment of joint irregularities and arthritis and to rule out a navicular stress fracture. In medial navicular avulsion fractures, x-rays will show calcified flecks or fragments on the medial navicular (Fig. 14-22). Additional supination oblique views (Fig. 14-23) sometimes are helpful, especially when an accessory navicular is present. Widening of the synchondrosis may or may not be seen.

Figure 14-19 Radiographic findings of chronic, dorsal, navicular nonunion. Note rounded edges and smooth contour in distinction from acute fracture in Fig 14-18.
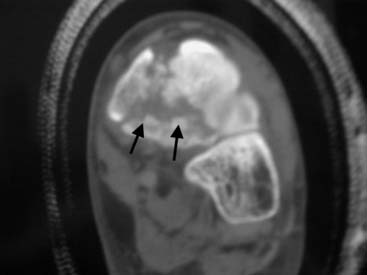
Figure 14-20 Computed tomography (coronal view) demonstrating more involved navicular body fracture with comminution.
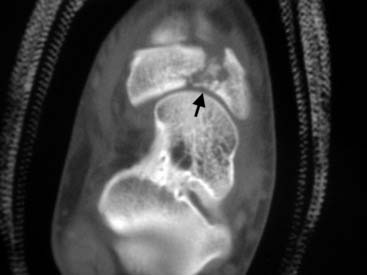
Figure 14-21 Computed tomography (axial view) demonstrating navicular body fracture with displacement.

Figure 14-22 Anterior-posterior radiograph of foot demonstrating comminute medial navicular avulsion fracture.
Treatment
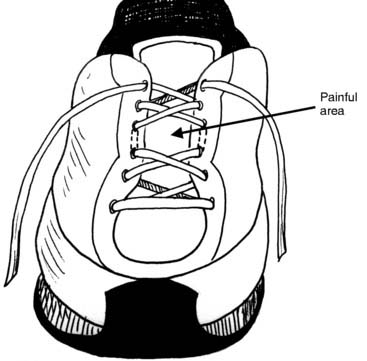
When a painful nonunion develops, an injection of corticosteroid sometimes will relieve the symptoms. Alternative shoe lacing (Fig. 14-24), or a donut-type pad may reduce pressure in the area. If conservative treatment fails, the usual surgical treatment is excision of the fragment through a small dorsal longitudinal incision. Postoperatively the patient is nonweight bearing in a boot for approximately 2 weeks, followed by progressive weight bearing and active range of motion (AROM).
In chronic cases in which a bony union has resulted in a painful bony prominence or dorsal talonavicular joint arthritis, conservative treatment is nonsteroidal anti-inflammatory drugs (NSAIDs), alternative shoe lacing or a donut-type pad dorsally, and molded foot orthoses with good arch support. A cortisone injection also may be helpful. If nonsurgical care is unsuccessful, the prominent and arthritic portion of the talus or navicular may be resected in a V-shaped fashion (Fig. 14-25), leaving healthy joint behind. In severe cases of posttraumatic talonavicular arthritis, fusion may be needed.
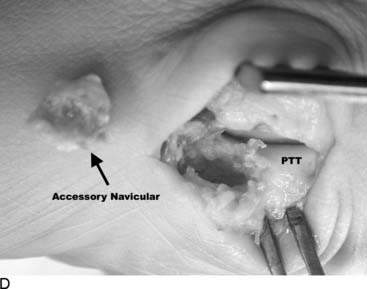
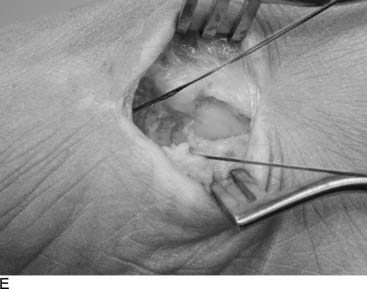
Treatment of acute medial navicular fractures usually is conservative. Protection in a nonweight-bearing boot for 6 weeks until nontender followed by appropriate therapy for the posterior tibial tendon, usually will produce good results. The avulsion fragments may or may not demonstrate bony union on follow-up x-rays in successful cases. The rare large displaced fragment may require open reduction internal fixation (ORIF) (Fig. 14-26, A and B). The conservative treatment may be tried for nondisplaced accessory navicular injuries but in my experience is less successful. Excision of the accessory navicular and repair of the posterior tibial tendon to the navicular with bony anchors (Fig. 14-27, A through G, followed by protection in a nonweight-bearing boot for 6 weeks, may be needed.
Cuboid Fractures
Incidence and mechanism
Cuboid fractures are much more rare in an athletic foot and ankle practice but tend to be overlooked and dismissed as a foot sprain. Two basic types are seen as athletic injuries: (1) an avulsion injury, caused by an inversion/adduction injury while landing (basketball, volleyball, and so forth) or rapid direction change (soccer, rugby, football) and (2) a compression injury, caused by forced eversion while plantarflexed or dorsiflexed in a pileup (e.g., football, rugby). In the avulsion cuboid injury, the calcaneocuboid capsule and plantar C-C ligament are torn, producing a usually small avulsion fragment off the plantar posterior cuboid. In the compression injury, the cuboid is crushed between the calcaneus and fifth metatarsal.
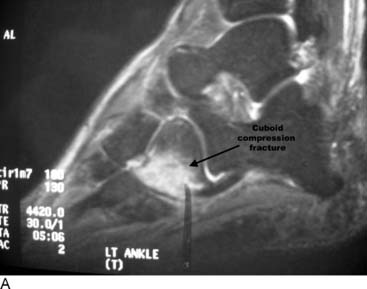
Imaging
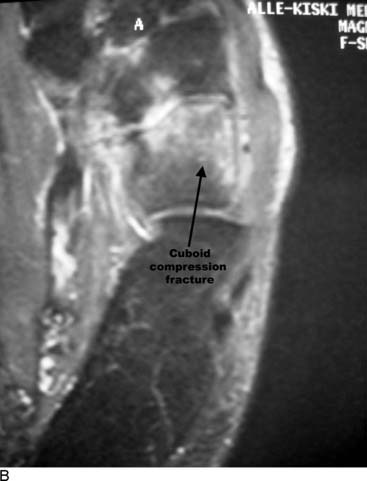
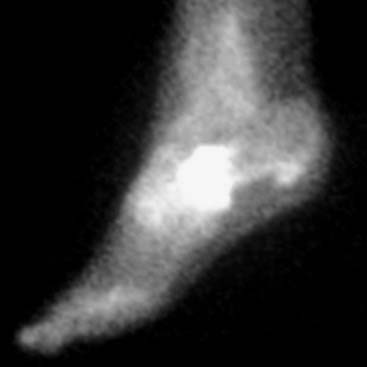
The small avulsion fractures may be seen with careful inspection of lateral or oblique x-rays (Fig. 14-28). Compression injuries of the cuboid often do not show on standard x-rays. Posthealing x-rays may show increased radiodensity (Fig. 14-29). A magnetic resonance imaging (MRI) (Fig. 14-30, A and B) or bone scan (Fig. 14-31) can be used to confirm the fracture. Healing then must be followed by either routine radiographs or CT.

Figure 14-29 Lateral radiograph of foot depicting increased density of cuboid indicating healing of prior occult cuboid fracture.
Fractures of the Anterolateral Process of the Calcaneus
Incidence and mechanism
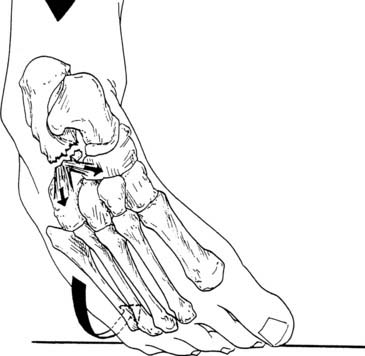
The anterolateral process fracture represents up to 23% of all calcaneus fractures.5 Two mechanisms of injury to the anterolateral process of the calcaneus have been noted.6,7 An inversion injury to a plantarflexed foot (much like the mechanism for a common ankle sprain) will produce an avulsion fracture of the tip of the anterolateral process through tension on the bifurcate ligament (Fig. 14-32).
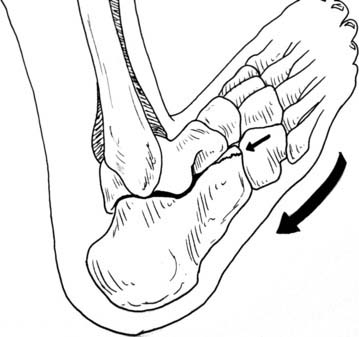
The second mechanism of injury to the anterolateral process is an eversion abduction injury (Fig. 14-33) that produces a compression-type horizontal fracture through the calcaneus.5,7 Degan et al.7 proposed the following classification for fractures of the anterior lateral process of the calcaneus: type I—nondisplaced tip avulsion, type 2—displaced avulsion fracture not involving the calcaneocuboid joint, and type 3—displaced larger fragments involving the calcaneocuboid joint.
Diagnosis
Examination will show point tenderness over the bifurcate ligament and the anterolateral process of the calcaneus (Fig. 14-34). Lateral ankle instability tests (drawer test, talar tilt test, and flexion rotation drawer test) often are negative. Often pain may be produced by inversion stress through the subtalar joint (distracting the fragment). There may be instability of the transverse tarsal joint, which is tested by holding the heel stable with one hand and pronating and supinating the midfoot with the other hand (Fig. 14-35, A and B).
Imaging
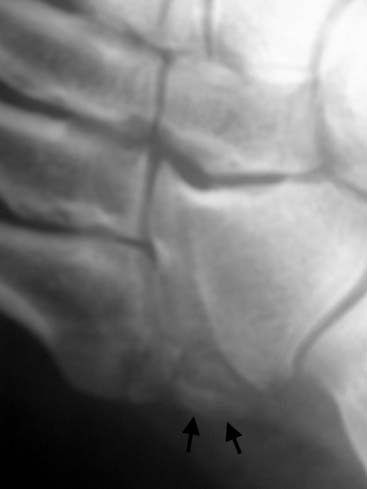
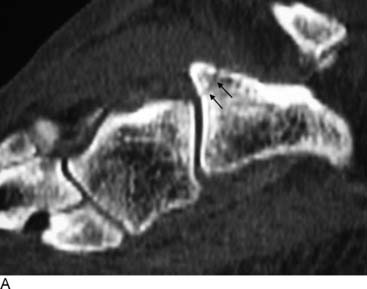
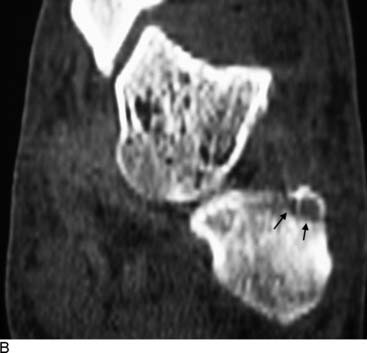
As stated previously, initial x-rays may be interpreted as negative if the fracture is nondisplaced. However, review of the old x-rays or new anterior-posterior (AP), lateral, and oblique x-rays of the foot may show a displaced fracture through the tip of the anterolateral process of the calcaneus (Fig. 14-36). Alternatively, a large, blunted, irregular and indistinct process may be visualized (Fig. 14-37). In cases in which point tenderness exists over the anterolateral process but x-rays are not conclusive, a CT scan (Fig. 14-38, A through C) often will show the fracture and help in assessing the amount of healing. The CT also is helpful in surgical planning (ORIF vs. excision). A bone scan is used as a screening tool to distinguish this injury from other soft-tissue types of lateral ankle injuries.

Figure 14-36 Lateral radiograph of hindfoot demonstrating small anterior process fracture (arrows) of calcaneus.

Figure 14-37 Lateral radiograph of hindfoot demonstrating healed fracture of anterior lateral process (ALP) of calcaneus.
Treatment
For cases of malunited fractures of the anterolateral process of the calcaneus, arthritic changes in the superior portion of the calcaneocuboid joint and/or the junction between the process of the calcaneus and navicular may exist. In these cases, a trial injection of cortisone in the calcaneocuboid joint and calcaneonavicular space may provide relief or help to establish the diagnosis of arthritic changes. A CT scan or MRI with magnified views will help to provide information about the joints. Surgical treatment involves open resection of a portion of the anterolateral process of the calcaneus, trimming it back to a point at which a healthy calcaneocuboid joint is present. Recently, arthroscopic resection through a subtalar approach has been described.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree