Os Trigonum Surgery
Molly A. Judge
Surgery for recalcitrant pain and dysfunction associated with the os trigonum is described as primarily an arthroscopic technique in the current literature. Specifics in designing arthroscopic portals and technical pearls for this type of exploration are discussed extensively in the most modern literature. There are reasons to gravitate to an open procedure when addressing this pathology, and those conditions generally involve compound deformity: symptomatic os trigonum in the presence of chronic lateral ankle instability, flexor hallucis longus (FHL) tenosynovitis, peroneal tendon dysfunction or osteoarthritis of the rear foot, and/or midfoot complexes. Consequently, the postoperative course for excision of an os trigonum can vary dramatically depending upon the technique employed (arthroscopic vs. open surgery) and the adjunctive procedures performed. As with any pathology of the lower extremity, the differential diagnosis for chronic ankle pain is extensive and misdiagnoses do occur. For these reasons, the clinical evaluation and in some cases ancillary imaging techniques are important to support the working diagnosis and identify occult injury or deformity when it exists.
FUNCTIONAL ANATOMY
Prevalence of this accessory ossicle has been reported from 3.0% to 13.0% (1,2) and its presence has been identified in the 12-week embryo (3) and the 2-month-old fetus (4). At birth, this ossification centroid is cartilaginous (5). By the age of 8 to 11, the ossification center appears radiographically, and within a year, it will unite and become the posterior process of the talus. McDougall suggests that it is the separation of this ossification center that yields the os trigonum (6). After repetitive plantar flexion over time, this process will ultimately separate due to impingement from the tibia. This secondary ossification center may begin as separate and distinct from the talus or results as a separate entity due to repetitive trauma as experienced by soccer players, ballet dancers, or the paralytic dropfoot patient, just to name a few.
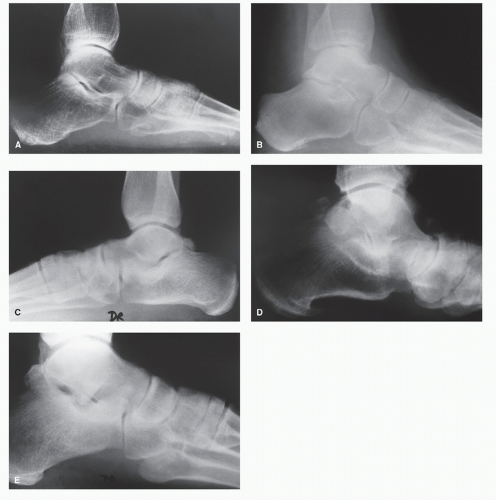
To fully understand os trigonum syndrome, the os should be differentiated from the posterior lateral tubercle of the talus. This posterior lateral prominence is much larger than its medial counterpart and can range from barely prominent to a large protuberance emanating from the posterior lateral aspect of the talus (Fig. 49.1). The inferior aspect of the lateral process articulates with the proximal rim of the posterior calcaneal facet forming a hook-like projection across the posterior subtalar joint. When this process is degenerated or injured, a partial fusion of the posterior facet of the subtalar joint may result. When fractured, this triangular- to rhomboid-shaped fragment may appear as separate and distinct from the talus, a Shepherd fracture, and can be confused with the os trigonum. When the os trigonum is fused to the lateral process, it is referred to as a “trigonal process” and then a zone of fibrous, cartilaginous, or fibrocartilaginous junction is often present (7). Prevalence of this accessory ossicle has been reported from 3% to 13% when taking into account clinical case reports found within the literature (1,2). Based upon strictly anatomical studies, the frequency of occurrence of the os trigonum is reported from 2.7% to 7.7% based upon four separate studies reviewing 2,142 tali in adult specimens (8,9,10 and 11). In one sports medicine clinic, 100 consecutive ankle radiographs revealed a 14% occurrence of the os trigonum, suggesting this ossicle may be even more prevalent than previously reported in an athletic population (12).
Children and adolescents are generally spared of injury to the ossicle as the os trigonum does not ossify until the second decade of life and usually fuses within 1 year of its radiographic appearance (between the ages of 8 and 10 years in females and 11 and 13 years in males). In this age group, the ossicle is rarely symptomatic as its attachment to the talus is cartilaginous until the time of ossification. Its incidence of appearance is found unilaterally twice as often as bilaterally (13).
The os trigonum syndrome has been associated with an age group beginning with the younger adult population, often ranging from 20 to 35 years of age (14). Traditional classification schemes focus upon the morphology of the posterior process and the ossicle when it is present. A staging system suggested by Watson and Dobas includes type I, considered a normal posterior tubercle without clinical consequence. Type II, Steida process, is an enlarged tubercle prone to injury during extreme plantar flexion of the ankle. Type III is an accessory bone, the os trigonum, which can be the source of discomfort due to repetitive micro- or macrotrauma often seen in athletes. Type IV is a coalition or fused os trigonum, which forms a synchondrosis or syndesmosis with the posterior talus (15).
The mechanism of injury in the os trigonum syndrome is that of a “nut cracker”-type compression or fracture within the posterior aspect of the rear foot and ankle, an impingement between the superior aspect of the calcaneus and the posterior malleolus of the tibia. A hypertrophic prominence may be found at the most superior pole of the posterior calcaneal tuber that may contribute to the incidence of injury to the ossicle (16).
Ligamentous attachments of the posterior lateral tubercle of the talus include the posterior talofibular ligament laterally, the deep layer of the flexor retinaculum and the posterior tibiotalar portion of the deltoid ligament medially and the posterior talocalcaneal ligament attaching upon its inferior aspect. All of these ligaments contribute to the functional stability of the posterior subtalar joint. When the posterior lateral tubercle of the talus is fractured, rear foot stability is reduced. In contrast, if the os trigonum is fractured, pain and dysfunction associated with impingement of the os between the long flexor of the hallux and the posterior subtalar joint may exist, but the stability and integrity of the posterior subtalar joint remains
unchanged. Therefore, determining the proper technique and execution for the excision of a symptomatic os trigonum is critical to maintaining that stability. Iatrogenic disruption of one or a combination of ligaments about the posterior subtalar joint can destabilize a previously sound joint. Paulos described a bifurcate ligament traversing the posterior subtalar joint consistently present in his dissections. This ligament tethers the posterior process of the talus both medially and laterally. Once the posterior process was osteotomized, it became evident that the ligament would distract the posterior fragment as the ankle was put through sagittal plane range of motion. This ligament attaches to the lateral process along with the posterior talofibular ligament, while the medial attachment is the posterior talocalcaneal ligament (17). The FHL runs through this bifurcate ligament, and it is within this tethered arrangement that that the FHL comes into contact with the os trigonum. In viewing this arrangement from the posterior subtalar and ankle joints, it is easy to appreciate how FHL tendonopathy may develop in conjunction with a hypertrophic tubercle or an irritated and inflamed os trigonum. It is suspected that the distraction effect of the bifurcate ligament is the culprit for the nonunion of a fractured os trigonum or posterior process of the talus. In Sheperd’s dissections, he noted that the deeper the groove for the FHL tendon, the larger the process of the talus (18). That observation is consistent with the current philosophy that the hypertrophic posterior process and or irritated ossicle are often associated with the repetitive mechanical stress from the FHL tendon seen in dancers with os trigonum syndrome.
unchanged. Therefore, determining the proper technique and execution for the excision of a symptomatic os trigonum is critical to maintaining that stability. Iatrogenic disruption of one or a combination of ligaments about the posterior subtalar joint can destabilize a previously sound joint. Paulos described a bifurcate ligament traversing the posterior subtalar joint consistently present in his dissections. This ligament tethers the posterior process of the talus both medially and laterally. Once the posterior process was osteotomized, it became evident that the ligament would distract the posterior fragment as the ankle was put through sagittal plane range of motion. This ligament attaches to the lateral process along with the posterior talofibular ligament, while the medial attachment is the posterior talocalcaneal ligament (17). The FHL runs through this bifurcate ligament, and it is within this tethered arrangement that that the FHL comes into contact with the os trigonum. In viewing this arrangement from the posterior subtalar and ankle joints, it is easy to appreciate how FHL tendonopathy may develop in conjunction with a hypertrophic tubercle or an irritated and inflamed os trigonum. It is suspected that the distraction effect of the bifurcate ligament is the culprit for the nonunion of a fractured os trigonum or posterior process of the talus. In Sheperd’s dissections, he noted that the deeper the groove for the FHL tendon, the larger the process of the talus (18). That observation is consistent with the current philosophy that the hypertrophic posterior process and or irritated ossicle are often associated with the repetitive mechanical stress from the FHL tendon seen in dancers with os trigonum syndrome.
HISTORY AND CLINICAL EVALUATION
There is often a history of repeated injury or routine activity requiring repetitive sagittal plane ankle motion in heavy weightbearing sports such as ballet, soccer, and gymnastics (12,19). Pain may manifest after a significant ankle sprain in which symptoms are recalcitrant despite usual conservative efforts such as relative rest, ankle compression devices, cryotherapy, and oral or topical anti-inflammatory medications. A sense of giving way or weakness may be an associated complaint that fails to respond to conservative care. Although the incidence of os trigonum syndrome after an ankle sprain is small, the coincidence of this condition is likely underreported. In the world of medicine, this condition is considered relatively obscure and as such may be misdiagnosed in favor of more a more common and better understood diagnosis such as tendonitis (12). In Fallat’s report of 639 ankle sprains, only 0.2% suffered from os trigonum syndrome (20).
After a significant ankle sprain, one that does not spontaneously resolve within a few days, many will suffer from prolonged pain and disability due to improper diagnosis and treatment. In Gerber’s prospective study of 104 ankle injuries, all patients had returned to work by the 6-month follow-up; however, 40% continued to suffer from residual pain and dysfunction. This chronic pain and dysfunction is often the result of a failure to identify significant pathology associated with ankle sprains. In 104 ankle injuries, 96 were ankle sprains, including 16 syndesmotic injuries (21).
Subjective complaints associated with an os trigonum include poststatic dyskinesia aggravated by heavy and or prolonged weight-bearing activities. Often described as a vague aching within the posterior ankle, concomitant complaints of lateral ankle pain and stiffness within the peroneal group are common. At times, patients may relate the pain stems from the back of their heel, yet they indicate a region within the Kager triangle rather that the posterior or inferior calcaneal tubercle. The pain is often aggravated in weight-bearing conditions such as when walking on uneven terrain, descending the stairs, or walking on declinated surfaces such as driveways or ramps. Athletes will complain of pain specifically when they are pushing off on the ball of the foot but not when standing or walking. At times, the sense of giving way may be an additional complaint. Due to the plantarflexed position of the ankle when off weight-bearing (sitting or lying down), discomfort may be present even when the ankle is off-loaded. The literature reports this condition among specific athletes; those requiring repetitive forceful plantarflexion and ballet dancers seem to fit the patient profile best (19,22,23,24,25,26,27,28,29,30,31 and 32). While other categories of athletes may develop this condition, even nonathletes can be affected as there are a number of case reports involving nonathletic patients (23,24,33,34,35,36 and 37). Ultimately and ironically, the ankle will be restricted in the direction of dorsiflexion despite the fact that a plantarflexory force produced the dysfunction.
The pain is typically described as a dull aching sensation deep within the posterior ankle. During the initial interview, it is important to have the patient point to the target area of tenderness with one finger. This basic exercise will eliminate a host of confusion that can interfere with a focused clinical examination such as the patient’s inability to differentiate the ankle joint from the rear foot or midfoot complexes. It is all too common that patients report ankle pain when in fact they actually point to the sinus tarsi or even the talonavicular joint as their target of tenderness. Worse yet, the patient may simply wave his or her hand down at the foot and ankle reporting “… the pain is just all through there.” This is an unacceptable description of the region of the chief compliant, and the patients must be coached to clearly define their principle region of tenderness. When the patient is poorly compliant with this exercise, ancillary imaging may be helpful.
The clinical evaluation of a symptomatic os trigonum is no different than that of any other chronic ankle condition in that a stepwise approach is taken in assessing ankle motion, ligamentous integrity about the foot and ankle, and isolation of the point of maximum tenderness. Point tenderness upon deep palpation within the most distal extent of the Kager triangle is a telling feature. The range of motion of the ankle, rear foot, and midfoot complexes are assessed individually, and any evidence of crepitation, restriction of motion, or tenderness is specifically located. Rear foot motion may be restricted with associated peroneal spasm when the os trigonum presents as a malunion at the posterior subtalar joint facet (36). Manual muscle testing may reveal an impingement syndrome, crepitation, or triggering within the FHL tendon (19,25,26,38).
Generally, the clinical exam fails to elucidate edema, erythema, or calor unless associated with acute trauma. Given the fact that os trigonum syndrome is most often due to a chronic ankle injury, it is a cool process in which the temperature gradient is within normal limits and there are no outward physical signs of injury or inflammation. The hyperplantarflexion test as described by Van Dijk is the most important clinical test specifically for os trigonum syndrome. With the patient supine or in the sitting position, the foot may be held in one of three positions: neutral, slightly internally rotated, or slightly externally rotated with respect to the tibia; depending on the location of the os, the actual target of tenderness may vary. To perform the test, the right distal tibia is stabilized with the examiner’s left hand, and the examiner uses the right hand to forcefully plantar flex the foot. This quick passive force reproduces the posterior impingement of the os between the posterior inferior aspect of the tibial malleolus and the superior aspect of the calcaneus. A negative test will not reproduce the pain, and the os trigonum syndrome is ruled out. A positive examination will reproduce the pain and/or crepitation associated with the chief complaint and should be supplemented then by a diagnostic block (39). It is strongly suggested to perform a diagnostic block as final confirmation and support of the principle diagnosis. When a positive result is obtained, the discomfort of the chief complaint will be temporarily eliminated, while the ankle, FHL tendon, and subtalar joint are manipulated. A diagnostic block using 1 mL of 1% lidocaine plain solution can be applied with or without the benefit of fluoroscopic guidance using a lateral approach (40). The injection is placed in the target area of tenderness as determined by deep palpation and manipulation of the rear foot and ankle. Injecting posterior to the peroneal tendons a small amount of anesthetic can be expected to produce a positive response when the diagnosis is an irritated or painful os trigonum. Once confirmed, it has been suggested to place a long-acting corticosteroid injection in this region in an attempt to achieve longer-lasting pain relief. Thus, injection therapy with a short-acting agent can be used first as a diagnostic block, and then later with a long-lasting steroid it can be used as a therapeutic modality (1,41).
The differential diagnosis for chronic posterior-lateral ankle pain is extensive and includes (in no particular order) sinus
tarsi syndrome, adhesive ankle or rear foot capsulitis, tibiofibular diastasis or syndesmotic injury, peroneal tendinopathy, peroneal subluxation, lateral ankle ligament disruption, chronic lateral ankle instability, osteochondral lesions of the ankle or rear foot joint, ankle impingement or exostosis, posttraumatic ligamentous calcifications, lateral Achilles tendon tear or lateral Achilles enthesitis, peritendinitis crepitans, gout, seropositive or seronegative arthropathies, and os trigonum syndrome. Goals in the preoperative examination are to determine the principle diagnosis and identify associated pathology including both dynamic and structural culprits for dysfunction and pain.
tarsi syndrome, adhesive ankle or rear foot capsulitis, tibiofibular diastasis or syndesmotic injury, peroneal tendinopathy, peroneal subluxation, lateral ankle ligament disruption, chronic lateral ankle instability, osteochondral lesions of the ankle or rear foot joint, ankle impingement or exostosis, posttraumatic ligamentous calcifications, lateral Achilles tendon tear or lateral Achilles enthesitis, peritendinitis crepitans, gout, seropositive or seronegative arthropathies, and os trigonum syndrome. Goals in the preoperative examination are to determine the principle diagnosis and identify associated pathology including both dynamic and structural culprits for dysfunction and pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree