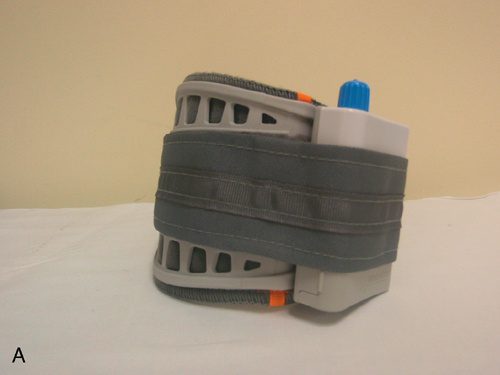
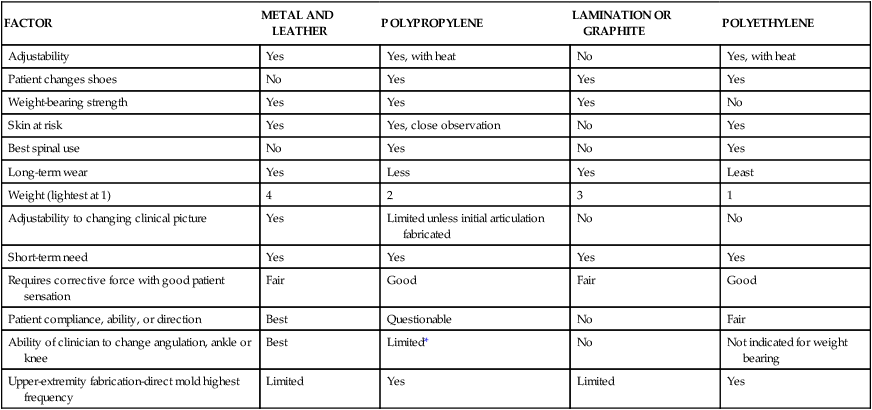
HEIDI TRUMAN, CPO and WALTER RACETTE, CPO After reading this chapter the student or therapist will be able to: 1. Identify and analyze the force systems produced by the use of an orthosis. 2. Comprehend the prescription rationale gained from an orthotic evaluation for individuals with neuromuscular dysfunctions. 3. Identify and differentiate the variables considered by the orthotist to optimize outcomes during orthotic intervention. An orthosis is an external device that produces a force that biomechanically affects the body to correct, support, or stabilize the trunk, the head, and/or an extremity. The goals in patient care with orthotic use vary from temporary application to permanent usage to maintain improvement. Orthoses are named by the sections of the body to which they are applied. For example, an orthosis that controls and covers the ankle and foot is called an ankle-foot orthosis (AFO). The abbreviations for the device are used by professionals in clinical documentation. Many factors enter into the decision regarding use and type of orthosis, and these will be discussed later. It is essential that the least complicated and most cost-effective orthosis be applied to the patient. The rehabilitation team must build a priority list of desired outcomes and accept that sometimes all of the items on the list may not be achieved by either the orthosis or the patient-team combination. At the very least, care must be attempted in stages because the patient’s condition changes or other medical concerns may arise. For example, an excessive number of custom-made and custom-fit plastic AFOs have been issued because they are “more cosmetic and lighter” than AFOs made of metal and leather material. There are times when all higher-priority goals can be achieved so that down the list the goals of cosmesis and light weight can be considered (Table 34-1). However, in the case of neuropathy of the foot, significant risk would be incurred by providing a total contact AFO made of plastic to keep it lightweight. A double-upright metal AFO with a well-fitting extra-depth shoe with a custom accommodative insert would fit the patient’s needs and take into consideration the sensory and motor changes within the lower extremity. Effective coordination and communication between health professionals in development of patient goals is essential during the evaluation process. For example, a design criteria omission as simple as placing a loop closure on the side that the patient cannot reach will prohibit the use of the orthotic device. A sound understanding of biomechanical and orthotic principles as well as skilled patient management techniques must be used to be successful with patients who require orthoses. TABLE 34-1 COMPARISON OF METAL AND PLASTIC ORTHOSES *Use in combination with metal joints produces best results. The advancements in and access to medical technology have had a profound effect in the field of orthotics. The evolution of plastic, composite, and metals fabrication technology has dramatically improved the ability to control, support, and protect all areas of the human body. Today, patients are fit for custom and prefabricated orthotic devices that provide a variety of functions in both a timely and cost-effective manner. These factors have led physicians to routinely prescribe orthoses for a wide range of medical conditions, whereas in prior decades lack of availability and shortage of experienced orthotists restricted patient access and narrowed the use of orthoses.1 Orthoses are important options for postoperative management, acute fracture management, and adjunct treatment, in addition to more traditional uses. For many, the proliferation of the prefabricated orthosis signaled a dilution of quality orthotic care, but in reality it has had the opposite effect. These readily available, cost-effective orthoses have not taken orthoses out of the hands of the orthotist but rather have moved them into the minds of treating professionals. There has been continued growth of new and improved orthoses and expansion into other areas of treatment previously lacking in orthotic management. For example, positional and corrective orthoses can be used for premature and newborn infants, and a wide range of sizes of orthoses that previously were made only in adult sizes have become available for pediatric patients. As with any new technological advancement, there has been incorrect application and use. It is not that many of these prefabricated orthoses are difficult to apply; rather, there has been lack of a clear understanding of the indications, contraindications, and limitations these devices present to the orthotist and other health professionals such as occupational and physical therapists. Advancements in technology have allowed the use of lighter, stronger materials in the fabrication of lower-extremity orthotics. Specifically, the substance called preimpregnated carbon is a graphite fabric with an exact amount of resin and catalyst already incorporated into the material. With the fibers properly directed over a model, it can be formed with heat. Graphite in other forms has been used in both prosthetics and orthotics for years. However, it had limited acceptance in orthotics because it did not significantly reduce the weight of the orthosis compared with other materials. It also lacked the properties to enable modification of the orthosis after the lamination process. The preimpregnated graphite has a dramatically reduced weight, still maintains its strength, and gives the orthotist the opportunity to use the dynamics of loading and response during the gait cycle. This allows for assistance in both the swing and stance phases of gait (Figure 34-1). A clinical example at the end of this chapter demonstrates this need in patient management. Another significant advancement in component technology has been the introduction of weight-activated orthotic knee joints. Although available in prosthetics for decades, the development of a lightweight, compact knee joint that would allow a patient to have knee stability during stance2 and clearance during swing phase has been elusive until recently. Before this, the available knee joints for knee-ankle-foot orthoses (KAFOs) involved some type of locking mechanism that remained locked throughout the gait cycle. The joint provided stabilization of the weak quadriceps musculature during stance but kept the knee in a fully extended position, making advancement of the limb in swing more difficult for the patient. There are specific indications and contraindications for stance control KAFOs, but early results are promising. This feature can significantly reduce energy output,3 as it is not necessary to raise the center of gravity to clear the locked knee during swing phase. This improves patient safety when walking on uneven surfaces. New technology for externally powered knee orthoses has just entered the market. These “bionic legs” are robotic aids worn during therapy sessions for gait training. They assist and augment the strength of the patient’s muscle and are most typically used in post–cerebrovascular accident (CVA) rehabilitation. Once the patient has achieved functional improvements, the use of the orthosis is discontinued. Other advancements in orthotic technology include the development of neuroprosthetic devices. These devices act through circuitry and programming to substitute for a deficit in the neural system. Functional electrical stimulation (FES) is a method of applying low-level electrical currents to motor nerves to restore function. In the 1960s the application of FES for foot drop was demonstrated by using a simple single channel to stimulate the common peroneal nerve to activate the ankle dorsiflexors. FES has widespread applications in many other neuroprosthetic devices such as cardiac pacemakers, cochlear stimulators, bladder stimulators, and phrenic nerve stimulators. Until recently, FES devices to provide ambulation assistance were large, unreliable, complex, and restricted to use in a therapy setting. The FES used in neurological rehabilitation attempts to unmask existing voluntary control (if any) and/or initiate dormant activity of the nerves and muscles. For FES to be used, the patient must have an upper motor neuron lesion. This means the nerve-to-muscle pathway is intact and the reflex arc is undamaged. Goals of FES address many rehabilitative outcomes. FES can reduce spasticity, synergy patterns, swelling, and blood clot formation as well as maintaining range of motion (ROM). FES used in gait can improve overall walking abilities by dorsiflexing the foot during swing to provide foot clearance, control initial contact, increase safety, decrease energy expenditure, and retrain muscles. FES has some application in the upper extremity as well, although at this time it is purely in a therapeutic setting. Currently, there are several FES units for foot drop on the market. These devices are used by patients in their daily lives and are not limited to the rehabilitation setting. The WalkAide from Innovative Neurotronics (Figure 34-2) and NESS L300 from Bioness (Figure 34-3) both function to provide dorsiflexion during the swing phase by stimulating the peroneal nerve. An ideal candidate for these devices must have an upper motor neuron lesion, good control of the knee joint, and drop foot. Common neurological conditions in which these devices are used are CVA and multiple sclerosis (MS). Both devices involve some sort of sensor to determine when the patient is initializing the swing phase of the gait cycle and send an electrical stimulus to the nerve to dorsiflex the foot. Advantages of functional FES over traditional orthotic management for foot drop are that it shifts an orthotic device from being a passive support to providing active assistance. FES stimulates the patient’s muscles to lift the foot, rather than acting as a passive splint to hold the foot. Alignment of the extremities and spine is a common function in orthotic prescription. The orthosis can provide either temporary or permanent function. A TLSO may be prescribed for stabilizing alignment after spinal fusion in the case of an unstable spinal cord injury (refer to Chapter 16). A supramalleolar orthosis (SMO) is commonly prescribed to hold the foot in proper alignment. When the goal of orthotic intervention is to correct alignment to a position well tolerated by the overlying soft tissue and/or the malalignment is a result of a muscle weakness, the new position should stabilize the joint. Clinicians need to remember that aligning one joint may result in the proximal or distal joint being placed in malalignment. An example of this is a genu valgum knee, which may seem easily corrected. However, changes in alignment result in adjustments by the other joints up and down the kinetic chain. Questions such as “Does the subtalar joint have the mobility to pronate?” must be asked and answered. During evaluation, review of the diagnosis and gathering of patient history are extremely valuable. A complete medical diagnosis will indicate important information to the team. For example, if a patient with poliomyelitis is to be seen, the orthotist is aware that it is a lower motor neuron lesion and that proprioception is intact (see Chapters 17 and 35). These patients have the benefit of skeletal balance in standing and ambulation and therefore require durable orthotic construction. Compare this with a similar result in muscle testing and ROM assessment for an individual with T12 level paraplegia. Assuming this is a complete lesion, patients with this upper motor neuron lesion lack proprioception. They require other means to get feedback about standing balance and require a lightweight orthosis, as they rarely use orthoses as a major means of locomotion. Although gathering patient history is a vital part of the evaluation, it is, more importantly, an opportunity to establish a productive patient management environment. Patients and family members have important information regarding the initial injury, previous medical care, reasons they sought additional care, and desired outcomes of new treatment. Most of this information can be gathered efficiently as either the therapist or the orthotist begins other professional evaluations. These are important patient and family management skills. One must hear from the patient or family why they came to see the health care professional and their expectations of care. The therapist should not assume the family’s goals without asking, as often patient and family goals are higher than the clinicians’ expectations. Communicating at a level that is understandable both is vital and demonstrates to the patient and family that the therapist is a concerned professional, thereby engendering trust and confidence. Complete and timely documentation of these findings is becoming increasingly vital to the evaluation and treatment plan. Whether communicating with others on the rehabilitation team, insurance carriers, or legal professionals, documentation and building medical justification are essential in treating all patients.
Orthotics: evaluation, intervention, and prescription
Overview

FACTOR
METAL AND LEATHER
POLYPROPYLENE
LAMINATION OR GRAPHITE
POLYETHYLENE
Adjustability
Yes
Yes, with heat
No
Yes, with heat
Patient changes shoes
No
Yes
Yes
Yes
Weight-bearing strength
Yes
Yes
Yes
No
Skin at risk
Yes
Yes, close observation
No
Yes
Best spinal use
No
Yes
No
Yes
Long-term wear
Yes
Less
Yes
Least
Weight (lightest at 1)
4
2
3
1
Adjustability to changing clinical picture
Yes
Limited unless initial articulation fabricated
No
No
Short-term need
Yes
Yes
Yes
Yes
Requires corrective force with good patient sensation
Fair
Good
Fair
Good
Patient compliance, ability, or direction
Best
Questionable
No
Fair
Ability of clinician to change angulation, ankle or knee
Best
Limited*
No
Not indicated for weight bearing
Upper-extremity fabrication-direct mold highest frequency
Limited
Yes
Limited
Yes

 The NESS L300 Foot Drop System.
The NESS L300 Foot Drop System.
Basic orthotic functions
Alignment
Evaluation
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree