Chapter 10 Orthoses for spinal trauma and postoperative care
Pathophysiology
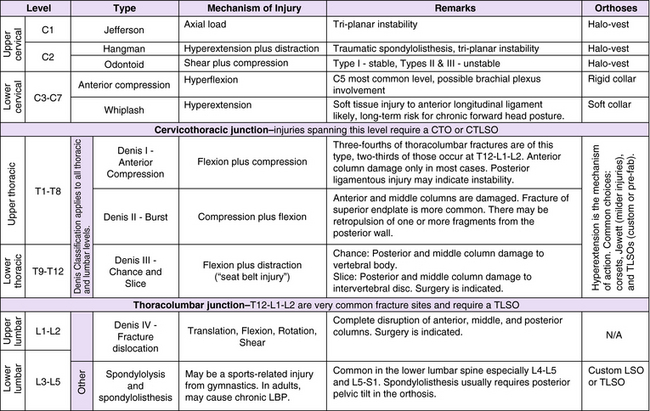
Before proceeding with orthotic treatment procedures, it is incumbent on the orthotist to independently verify the stability of the injury to the spine. The mechanism of injury, results of clinical examination, and radiologic evidence should be considered. In general, if the integrity of the anterior and/or posterior ligamentous complex is compromised, the injury should be considered unstable (Table 10-1).
Table 10-1 Criteria for stability of spine
| History of Mechanism of Injury | Physical and Neurologic Examinations | X-ray Examination Specific Criteria |
|---|---|---|
| Disruption of posterior ligamentous complex | Disruption of posterior ligamentous complex | Disruption of posterior ligamentous complex |
Hoppenfeld S: Orthopedic neurology: a diagnostic guide to neurologic levels, Philadephia, Lippincott Williams & Wilkins, 1977
Cervical spine fractures
A hangman fracture is a fracture through the pedicles of C2 that separates the posterior neural arch from the vertebral body. The mechanism of injury, which consists of hyperextension followed by distraction, is called traumatic spondylolisthesis. The spinal cord may be compressed, with possible transient neurologic findings. This injury also is unstable in all three anatomical planes, and the risk of neurologic damage is high in the absence of external support.
Compression fractures in the region C3–7 are hyperflexion injuries where the endplates of the vertebra may be damaged and the vertebral body fractured. The most common level of injury is C5, and the brachial plexus may be involved.14 Hyperextension injuries (e.g., from whiplash) are mostly soft-tissue injuries, and the anterior longitudinal ligament may be ruptured. A full clinical assessment must be performed to determine whether the injury is stable.25
Thoracic and thoracolumbar spine fractures
Normal thoracic kyphosis ranges from 20 to 50 degrees.2 Because of the kyphotic posture, the thoracic spine is especially vulnerable to flexion injuries. On the other hand, the ribs and their articulations provide considerable additional stability by restricting the mobility of the vertebrae. The lower thoracic vertebrae from T9–12 are considered transitional vertebrae and have more mobility.
Spinal trauma can be categorized with the Denis classification7 of acute thoracolumbar spinal injuries using a three-column theory (Fig. 10-1). If the anterior column of the spine alone is injured (Denis type I), the mechanism of injury is flexion followed by compression. If the anterior and middle columns are injured, causing a burst fracture (Denis type II), the mechanism of injury is compression followed by flexion. The posterior and middle columns can be injured through the mechanism of flexion followed by distraction (Denis type III). They can be through bone (Chance fracture), soft tissue (slice fracture), or a combination of the two. Fractures through soft tissue usually are treated surgically.
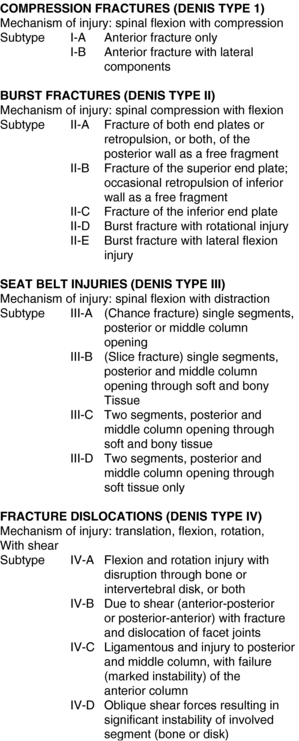
Fig. 10-1 Classification system for traumatic fractures of the thoracolumbar spine.
From Lusardi MM, Nielsen CC: Orthotics and prosthetics in rehabilitation. Philadelphia, WB Saunders, 2007.
According to Denis,7 approximately 50% of all fractures occur between T11–12 and L1–L2 levels, and almost half of thoracolumbar fractures that occur are compression fractures.
Lumbar spine fractures
Spondylolysis is the fracture of the pars interarticularis and is a stable condition. Spondylolisthesis is the anterior migration of one vertebral body over another and may or may not be stable.
Complicating factors
Obesity occurs in near epidemic proportions in the United States.34 The presence of substantial excess adipose tissue may deteriorate the performance of an orthosis by compromising its stabilizing effects.1 Because the orthotic practitioner likely will treat patients with the comorbidity of obesity, strategies should be in place to cope with this complication.14
Historical perspective
Spinal trauma
Understanding the historical traditional approaches to spinal trauma and treatment provides a foundation for learning from previous successes and decreasing the probability of future mistakes. These approaches are related specifically to the mechanism of injury (of the trauma) and the mechanism of action (orthotic treatment) addressing the injury. The mechanism of injury in the past (and frequently in the present) was routinely categorized by terms such as lateral flexion, compression, rotation, and extension injuries. Although this approach can have meaningful clinical application, it also runs the risk of oversimplifying complex injury mechanisms that then are managed orthotically in an inappropriate manner (Fig. 10-2).37
For example, a patient may present with an anterior compression fracture that resulted from a small compressive load but also associated with a major forward bending moment that has simultaneously disrupted the posterior ligamentous structures. The result is a motion segment more susceptible to instability secondary to shear. This also has been liberally reported as the main factor for destabilization of a compression fracture.21,37,38 If the focus remains only on the compression fracture, then the logical orthotic treatment may result in use of a Jewett three-point hyperextension orthosis. Although the lumbar pad is an important element of this three-point hyperextension addressing the compression fracture, it also introduces the element of shear with its anteriorly directed transverse force. Ultimately the patient is at greater risk for further instability and increased discomfort. In this example, a better knowledge of the mechanism of injury may have resulted in a more logical and predictable treatment strategy and outcome.
Current issues and research
Nonsurgical treatments of spinal trauma
Cervical fractures
The primary orthotic goal is to immobilize a fracture of the cervical spine. The orthotist may be faced with the questions of which orthosis to recommend, and, in particular, whether the recommended device should be a cervical orthosis or a cervicothoracic orthosis. These devices are used for both nonoperative and postoperative care. To shed light on the issue, Gavin et al.11 analyzed two cervical orthoses (Aspen and Miami J) and two cervicothoracic orthoses (Aspen two-post and Aspen four-post) using video fluoroscopy. They concluded that cervicothoracic orthoses provided significantly more reduction of cervical intervertebral and gross range of motion in 20 normal subjects compared to cervical orthoses. The two collars performed the same.
In the elderly, half of cervical spine fractures occur at the C1-C2 level. Fractures of the odontoid are the most common cervical fractures in patients older than 70 years and account for 10% to 15% of all fractures of the cervical spine.30,33 Tashjian et al.33 studied 78 patients older than 65 years with type II or type III fractures of the odontoid, which were considered unstable. They found that the patients managed with a halo vest had a mortality rate of 21% as well as higher rates of complications such as pneumonia and cardiac arrest compared with patients managed surgically or with a rigid cervical orthosis. The study also suggested that when managing an elderly patient having an odontoid fracture with a halo vest, extreme caution and daily supervision are required.
Injuries to the cervical spine resulting from motor vehicle accidents are common. Reduction or reversal of cervical lordosis that can lead to abnormal forward head posture is associated with whiplash injuries. With the head forward of its normal position, loads on the posterior musculature and vertebral bodies can increase significantly. Cervical kyphosis is a known primary risk factor for chronic pain in whiplash-associated disorders.15 Some evidence indicates that correcting the posture can relieve the symptoms to a great extent.9 An orthosis for this purpose should use the mechanism of retraction of the head rather than extension.25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree