Chapter 8 Orthoses for spinal pain
Historical perspective
Orthoses have been used in the management of spinal pathology for hundreds of years, with the earliest reported use from ancient Egypt more than 2500 years ago.91 Most of the early orthotic devices, which were specifically designed for treatment of spinal deformities, used wood and iron frames, leather straps, paper cellulose, and glue.11 The development of new composite materials, polymer resins, and thermoplastics has led to a number of commercially available orthoses that are extremely lightweight and comfortable, almost completely replacing the heavy, cumbersome devices of the past. Use of polypropylene and other thermoplastics has allowed production of relatively inexpensive, rapidly fabricated custom-molded orthoses and a proliferation of orthotic use for a wide variety of orthopaedic conditions.
Spinal orthoses for back pain
Pathophysiology
Back pain is one of the most common disabling conditions experienced by individuals throughout the industrialized world, affecting more than half of Americans at some time during their lives. Epidemiologic studies have reported that the lifetime prevalence of experiencing low-back pain is as high as 80% in the general population.34
In 80% to 90% of patients presenting with disabling low-back pain, the precise diagnosis is unknown.92 Dillane et al.27 found that 79% of men and 89% of women who presented with a first episode of back pain to a general practice office were classified as having back pain of unknown origin. Some authors have estimated that only 15% of chronic low-back pain cases have an identifiable pathoanatomic explanation.74
The posterior longitudinal ligament, outer lamina of the posterior annulus fibrosus, and ventral dural sac and blood vessels of the vertebral body are innervated by branches of the sinuvertebral nerve, which is formed by ventral rami and autonomic roots from gray rami communicantes. Transverse and descending branches supply the posterior longitudinal ligament at the level of nerve entry, with an ascending branch to the next cranial level providing overlapping innervation at each spinal level. Segmental branches from ventral rami supply the ventral annulus fibrosus and anterior longitudinal ligament. The dorsal rami divide into multiple branches innervating the paraspinal musculature and facet joint capsules.
Treatment recommendations
The vast majority of nonspecific low-back pain is managed conservatively with rest, analgesics, antiinflammatory medications, physical therapy, manipulation, and, in many cases, orthoses. Lumbar supports continue to be one of the most common methods of handling the impairment and disability caused by low-back pain, despite the lack of knowledge regarding their true physiologic effect or their effectiveness in relieving symptoms.2,53 One study found that 99% of orthopaedic surgeons had prescribed an orthosis at some time for their patients with low-back pain.78 A survey of patients indicated that 27% of patients with back pain for at least 2 weeks had used braces to relieve their complaints; the percentage increased to 37% in patients who experienced pain for 6 months or longer.25
Lumbar orthotic management
Contemporary corsets (Fig. 8-1) are composed of sturdy, lightweight canvas or elastic material. Vertical reinforcing stays usually are necessary to prevent the upper margin from curling away from the trunk. In the front, corsets extend from a point just below the xiphoid process to a point just above the pubic symphysis. Corsets cover the back from below the inferior border of the scapulae to the gluteal folds. Some corsets include posterior reinforcements made of rigid thermoplastic or metal that can be custom molded to the patient. Perineal straps usually are included, mainly for use by men, to prevent the garment from sliding upward with forward flexion; however, these straps can be uncomfortable and often are removed. Women’s corsets usually include garters to aid with prevention of upward displacement. Abdominal belts cover the pelvis, extending from the iliac crests to the pubic symphysis anteriorly and gluteal folds posteriorly.
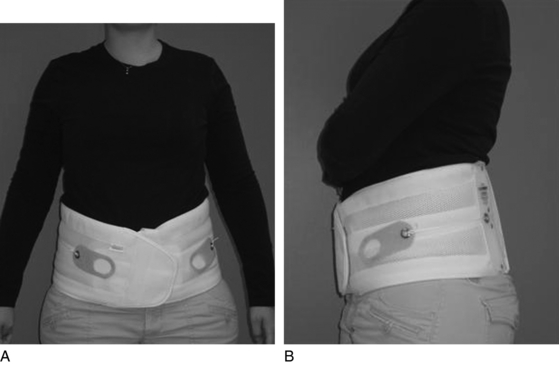
Fig. 8-1 Flexible lumbar corset.
Photos Courtesy of Dr. Daryl G Barth, CPO, of Orthotic and Prosthetic Associates of Central Illinois.
Rigid trunk orthoses or braces (Fig. 8-2) include stiff plastic or upholstered metal bands in both the vertical and horizontal planes, in contrast to corsets, which provide no horizontal reinforcement. When prescribed for pain relief, pelvic and thoracic bands are included that lie flat on the torso and terminate at the lateral midline. Frame-like constructs of some trunk orthoses make them cooler to wear than corsets. It is important that the rigid orthoses be fitted with the patient in both the standing and sitting positions to accommodate pelvic tilt and prevent pressure on the upper thighs or buttocks. Some rigid orthoses have inflatable pads that allow continued adjustment of fit. Custom-molded designs are available.
Mechanisms of action of lumbar orthoses
Several potential mechanisms of action for the pain-relieving ability of spinal orthoses have been proposed in the literature. The mechanical effectiveness of orthoses could result from intersegmental motion restriction, gross motion restriction, or decreased load on the spinal column. Other rationales include increased abdominal pressure, reduced muscle fatigue, increased postural awareness or proprioception, as well as the miscellaneous effects of massage, heat, and placebo. Unfortunately, conflicting results in the literature have led to criticism of most hypotheses based on theoretical grounds, with the mechanisms of action remaining a matter of considerable debate.14,83 Quite possibly, a combination of factors, varying from patient to patient, results in the pain relief experienced by patients using lumbar orthoses.
Motion restriction
The effect most often expected from a brace is restriction of motion; however, available literature investigating different orthoses and their ability to restrict motion has reported inconsistent results. Excessive trunk motion, especially axial rotation, often is assumed to be the cause of back injury. Orthoses are prescribed to prevent this excessive motion and thus reduce low-back pain.5
Norton and Brown76 inserted pins into the spinous processes of lumbar vertebrae and found surprisingly small effects on intersegmental flexion and extension movements when several different braces were used. The orthoses were unable to eliminate intervertebral motion, and the more rigid braces actually increased motion at the lumbosacral junction. This finding was confirmed by Lumsden and Morris58 using similar techniques but studying mainly rotation. Increased motion at L5–S1 with use of lumbar orthoses also was demonstrated by Miller et al.,67 leading some authors to suggest that fixation of the pelvis is essential in restricting motion.58,100 Another study using flexion and extension lateral radiography found lumbar supports were able to restrict the sagittal movements of the lumbosacral spine, although considerable variation between individuals was noted.30
More recently, roentgen stereophotogrammetric analysis has failed to show a stabilizing effect on sagittal, vertical, or transverse intervertebral translations with use of either a molded rigid orthosis or a canvas corset with a molded plastic posterior support.4 The authors concluded that an external lumbar support can decrease the overall load on the lumbar spine by restricting gross motions of the trunk but appears to have no stabilizing effect on the intervertebral mobility of the lower lumbar spine. This concept had been suggested previously,55 with gross motion restrictions thought to be of greater importance than intersegmental motion restrictions in the effectiveness of orthoses in patients with low-back pain.73
An extensive literature review focusing on proposed mechanisms of action concluded that lumbar supports reduce trunk motion with respect to flexion, extension, and lateral bending but provide no significant effect on rotation.99 In essence, no orthotic device has the ability to completely eliminate motion within the spinal column, and specific orthoses display a great deal of variability in motion restriction.
Unloading of the spinal column
Another common rationale for use of lumbosacral orthoses is based on the premise that the devices directly or indirectly provide some assistance to trunk extensor moment, reducing the activation of erector spinae muscles and consequently the magnitude of spinal compression forces. In direct unloading, the orthosis actually bears some of the load that would otherwise be transmitted through the lumbar trunk. In indirect unloading, the orthosis transmits little load but raises the intraabdominal pressure enough to unload the vertebral column.73 By compressing the abdomen, lumbar corsets and braces convert the trunk into a semirigid cylinder, reducing the usual paraspinal musculature workload by shifting a portion of the load from the spine to the entire trunk. A larger percentage of the upper body weight then is supported by the abdomen, relieving the vertebral column to some degree and requiring less back muscle force to extend the trunk.
In an attempt to demonstrate the spine unloading function of braces, numerous studies have examined intraabdominal pressure, differences in trunk musculature electromyogram, and changes in vertebral compression forces. Bartelink6 was the first to suggest that an increase in intraabdominal pressure could be used to unload the spine. Early work by Morris et al.71 showed that braces and corsets increased the intraabdominal pressure of the wearer by 10 to 15 mm Hg at rest. Morris and Lucas70 studied static lifting postures and found that myoelectric activity in the abdominal muscles decreased when braces were worn; however, intraabdominal and intrathoracic pressures were unchanged. Nachemson and Morris72 tested an inflatable corset and found that intraabdominal pressures remained generally low and inconsistent.
Waters and Morris103 measured the effect of chairback braces and lumbosacral corsets on the myoelectric activity of trunk muscles during level walking and found a great deal of variability in muscle activity. Nachemson et al.74 found inconsistent trends in the effect of orthoses on the myoelectric activity of trunk muscle and encountered no significant changes in intragastric pressure. This finding was supported by Lantz and Schultz,56 who reported that none of the orthoses they tested was consistently effective in reducing myoelectric activity, and that, in many cases, electromyographic signals increased when the orthoses were worn. They concluded that wearing a lumbar orthosis is mechanically effective only sometimes, often is not effective, and sometimes is counterproductive. They also indicated that the load restrictions were not dramatic even when wearing an lumbar orthosis was effective.56
On the other hand, Cholewicki16 suggested that although the additional support supplied by a lumbosacral orthosis may produce only a modest overall reduction in trunk muscle activity as measured by electromyography, the device still may be of functional significance in patients suffering from low-back pain. These patients exhibit increased trunk muscle contraction during activities of daily living, presumably in an effort to enhance the stability of the lumbar spines, thus creating a significant physiologic burden.98
In healthy subjects, as little as 2% of maximal voluntary activation from all trunk muscles may be sufficient to stabilize the spine in a neutral, upright standing position.17 Ergonomic studies have shown that static muscle contractions sustained above 5% maximal voluntary activation lead to muscle fatigue and pain, with contractions below 5% maintainable indefinitely.8,51 A small reduction in trunk muscle activity may be sufficient to bring contractions to below the 5% threshold; therefore, lumbosacral orthoses may provide symptomatic relief to some patients with low-back pain by reducing their necessary static trunk muscle contraction, preventing muscle fatigue that may compound their existing pain.17
Spine compression forces during lifting tasks have been investigated to determine the unloading effect produced by orthoses. An often cited study by Nachemson and Morris72 demonstrated a 25% decrease in intradiskal pressure with use of an inflatable corset in normal subjects standing upright. Lumbar belts have been suggested to modify trunk kinematics, resulting in lower spinal loads; however, reductions in spine compression force were not observed when task kinematics were controlled.63,87,108 Postural shrinkage, proposed as an indicator of the cumulative mechanical stress placed on the spine during physical activity, has been compared in patients with and without orthoses, but results have been inconsistent.60,84
Although both positive and negative results have been reported,56,57,60 collectively the scientific literature does not appear to support the hypothesis that orthoses reduce the activity of erector spinae muscles, increase intraabdominal pressure, or significantly impact compression forces.99
Proprioception
Some articles discussing lumbar supports have suggested various mechanisms of action that imply proprioceptive enhancement, such as improving posture, increasing awareness of pelvis and spine positioning, reminding patients to lift properly, and reminding patients not to overstress the back. This increase in proprioceptive input may be effective in relieving pain by reminding patients of their position in space and stopping patients from placing their trunk in harmful positions. McNair and Heine66 described improved trunk proprioception through increasing afferent input via the mechanoreceptors in the skin with use of lumbar bracing. Newcomer et al.75 demonstrated an improvement in repositioning error, a commonly used method of measuring proprioception with position sense, in subjects wearing a lumbar support. These studies support the concept that braces provide enhanced proprioception through increased cutaneous input, but some authors have suggested that bracing also may activate mechanoreceptors of the underlying musculature and joint capsules, providing another source of proprioceptive input.
Patient factors
Many of the investigations on lumbar bracing mechanisms of action have found considerable interindividual variation in mobility with and without use of supports, implying that patient characteristics could be as, or perhaps more, important than actual corset characteristics in spinal immobilization. In a study that focused on central obesity measured using waist-to-hip ratio, Todo95 specifically investigated interindividual differences and commented that the efficacy of lumbosacral corsets may be affected by central obesity.
Miscellaneous
Local temperature elevation, an increased feeling of safety, and the placebo effect have been suggested as other potential mechanisms alleviating low-back pain with use of spinal orthoses.2 Thick or padded material incorporated into lumbar supports has been shown to increase lumbar skin temperature by almost 2°C, perhaps supporting the concept that increased warmth improves low-back pain.40 However, this finding has been criticized because the amount of padding necessary to potentiate this effect is more than usually found in standard orthoses or corsets.11
Authors have described the development of psychological dependence on orthoses as a result of the sense of security or safety provided by the devices. Ahlgren and Hansen1 conducted a survey of randomly selected patients for whom a corset had been prescribed for back pain and found that 50% were still using their corset 4 years later, perhaps because patients had developed this type of dependence.
Given the inconsistent literature on the mechanisms of action of orthotic devices, many have attributed the pain-relieving properties of the devices to a placebo effect.47 Proving or disproving these beliefs is a nearly impossible task because “blinding” of patients cannot be accomplished as easily as with other treatment modalities.
Side effects and other considerations
Because bracing attempts to control the position of the spine through the application of external forces, orthotic designs must account for regional variations of the surrounding anatomy, such as the vital soft-tissue structures of the anterior neck, the rigid thoracic rib cage, and the bony pelvis. The surrounding soft-tissue envelope has a substantial effect on the ability of an externally applied force to control spinal movement, but it also can be an area of potential complications. Adverse effects of wearing lumbar orthoses include local pain, skin breakdown, gastrointestinal disorders, decreased vital capacity, increased lower extremity venous pressure, higher blood pressure, and higher heart rates.14,64
Concern has been expressed over the possibility of disuse atrophy of the lumbar muscles with use of lumbar supports, leading some authors to deprecate the use of lumbar supports.83 One study indicated that more than 40% of corset wearers reported subjective weakness of the trunk musculature.2 Walsh and Schwartz102 found no significant change in abdominal muscle strength after 6 months of lumbar brace use by a group of warehouse workers. Another study actually found an increase in isometric trunk flexor strength after 2 months of using a soft lumbar belt, with an insignificant decrease in trunk extensor strength.44 Eisinger et al.29 demonstrated statistically significant weakness of both concentric and eccentric trunk extension as well as concentric trunk flexion in patients who used lumbar orthotics for chronic low-back pain. Taking these findings into account, some believe orthoses should be used only intermittently and selectively recommend that any bracing technique should include a strong abdominal exercise program with postural reeducation to prevent muscular atrophy once the patient achieves symptomatic relief.21,90
In the experience of some authors, the usefulness of orthotic devices is limited because many of the devices are so uncomfortable that patients soon stop wearing them. Any motion restriction achieved likely can be attributed to the discomfort caused by the pressure of the orthosis on the skin and bony prominences of the patient.96 Buchalter et al.13 demonstrated an inverse relationship between a brace’s ability to restrict motion and patient comfort. They found that the most comfortable brace, an elastic corset, was the least restrictive of the braces tested, whereas the Raney jacket provided maximal restriction but was the most uncomfortable to wear.
Outcome studies and effectiveness of lumbar orthoses for spinal pain
The natural history of low-back pain is extremely variable, thus compromising the ability to objectively evaluate treatment strategies for efficacy. Whether or not due to an identifiable injury, symptoms may resolve spontaneously within a few days or weeks, or they may persist for months or years. Approximately 40% of patients will have resolution of symptoms within 1 week, 60% within 3 weeks, and well over 90% after 2 months.27 These often quoted percentages have fueled a recommendation for essentially “benign neglect” in the first several months of symptom occurrence.62 However, contemporary literature supports the concept that although many patients experience improvement, up to 75% have one or more relapses, and 72% continue to have pain at 1 year.97,101
Another limitation inherent to all studies evaluating the pain-relieving efficacy of orthoses is the inability to achieve a blind methodology.24 Spratt et al.92 added that the undoubtedly heterogeneous pathology comprising patients grouped together as having nonspecific or idiopathic back pain makes difficult the evaluation of treatment strategies. In support of this concept, Willner105 found that pain deriving from a spondylolisthesis appeared to respond to lumbar bracing more favorably than back pain with no specific identifiable cause.
The literature on the effectiveness of orthoses in the treatment of spinal pain has revealed inconsistent results. Two early studies are conflicting. Million et al.68 demonstrated superior pain relief with use of a lumbar corset incorporating a rigid plastic support; however, Coxhead et al.22 found no treatment at all was as effective as use of a corset. Similarly, Hsieh et al.46 and Pope et al.82 did not find differences in pain relief with use of a corset, soft-tissue massage, manipulation, or transcutaneous muscular stimulation. In contrast, Valle-Jones et al.96 demonstrated a significant difference with respect to pain, limitation of activity, ability to work, and use of analgesics in favor of lumbar support use for back pain after a 3-week period.
Koes and van den Hoogen53 concluded in a systematic review that the effectiveness of lumbar supports in the treatment of low-back pain remains controversial, adding that the methodologic quality of available randomized trials varies widely. Similarly, in a systematic review of the available literature using the Cochrane database, Jellema et al.48 found “limited” evidence that lumbar supports are more effective than no treatment at all for low-back pain. Unfortunately, whether lumbar supports are more effective than other treatments remains unclear.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








