46 Oral microbiology
The oral cavity harbors a number of microorganisms, which form the normal human oral microflora (e.g. viridans streptococci, anaerobic bacteria such as Fusobaterium spp, coagulase-negative staphylococci, Moraxella, Neisseria, Candida spp., herpesviruses). Most of the time bacteria, fungi and viruses live in a fine balance together without causing disease. Some people are asymptomatic carriers of potential pathogens such as Staphylococcus aureus or Streptococcus pneumoniae without causing harm. Oral disease can occur if the microbial flora or the host defences change. This may be as a result of hormonal changes, poor dental hygiene, immunosupression (e.g. HIV), stress or use of broad-spectrum antibiotics. There are also a number of systemic infectious diseases that manifest in the oral cavity (Table 3.46.1).
Table 3.46.1 SYSTEMIC INFECTIOUS DISEASE WITH ORAL MANIFESTATION
| Infection | Oral manifestation |
|---|---|
| Scarlet fever (Streptococcus pyrogenes) | ‘Strawberry tongue’ (white tongue with red papillae) |
| Syphilis (Treponema pallidum) | |
| Primary infection | Painless, small nodules and ulcers |
| Secondary infection | Shallow, ‘snail-track’ ulcers |
| Tertiary infection | ‘Gumma’, painless, punched out ulcers |
| Congenital | Hutchinson’s teeth (peg shaped teeth, notch in upper incisors) |
| Valley fever (fungal, Coccidioides immitis) | Oral ulcers |
| Hand, food and mouth disease (coxsackie virus) | Pharyngeal ulcers |
| Chicken pox (varicella zoster virus) | Mucosal vesicles and ulcers |
| HIV | Gingivitis |
| Measles (prodrome) | Koplik’s spots (red spots in buccal mucosa) |
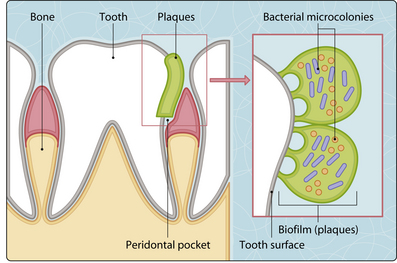
Dental plaques and caries
Teeth have a hard protective layer of enamel. Food can collect in pits and cervices of the teeth, encouraging bacterial colonization and growth, which initiates the development of dental plaque. Within the plaque, bacteria form primitive communication systems (biofilms) where they are protected from the host response and the effect of antimicrobial agents (e.g. antibiotics, disinfectants) (Fig. 3.46.1).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree