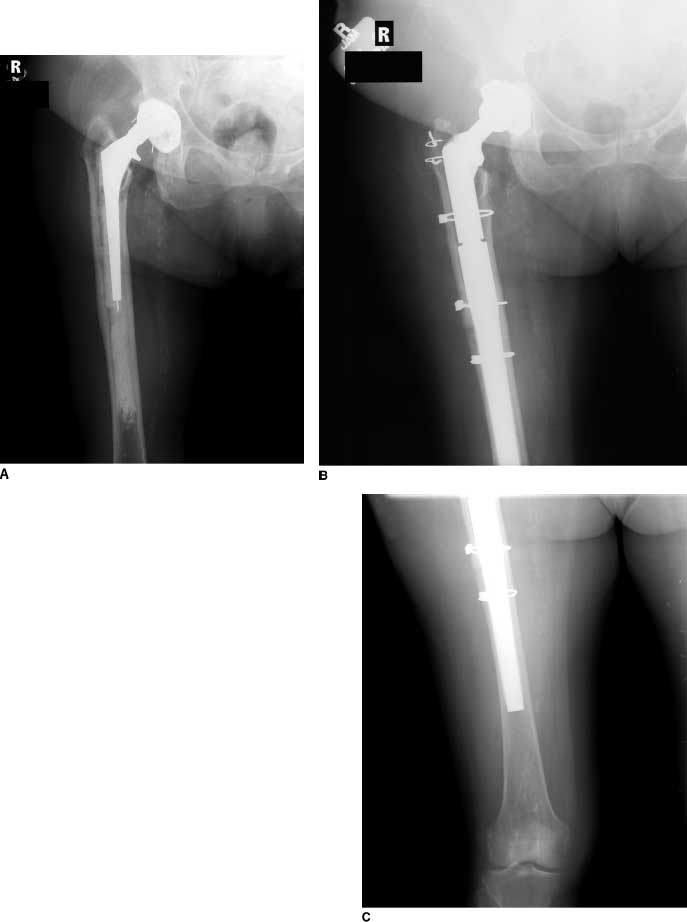
FIGURE 8-1. A: Radiograph of failed THA with marked protrusion. B: A transtrochanteric approach was necessary to facilitate safe hip dislocation and failed cup extraction.
Intrapelvic migration of the acetabular component requires special consideration. A retroperitoneal approach may be needed when the implant is in intimate contact with or attached to a vital intrapelvic structure. In most cases, as an acetabular component migrates medially, a membrane forms between the implant and the intrapelvic structures. In these circumstances, the implant usually can be extracted safely through the external pelvis (Fig. 8-2). However, if extraction through an external approach cannot be effected safely, then a retroperitoneal approach, over the pelvic brim, is needed. This approach may be performed in conjunction with a general surgeon.
FIGURE 8-2. Radiograph of loose acetabular component with notable intrapelvic migration. At revision the cup was extracted safely through the bone defect without a retroperitoneal approach.
Most loose femoral components can be removed through a conventional anterolateral or posterior approach. Circumstances in which extensile exposures are needed include a well-fixed femoral implant, a well-fixed cement column, and notable proximal bone deformity (Figs. 8-3 and 8-4). In each of these scenarios, an extended trochanteric osteotomy can provide tremendous benefits. A well-performed extended trochanteric osteotomy saves bone stock and facilitates a more rapid component removal. In addition, an extended osteotomy can preserve muscle and muscle attachments to bone, which in turn may improve functional results of the operation and reduce hip instability. Timely use of trochanteric osteotomy also can reduce the risk of a bony fracture during failed implant removal or revision implant insertion.
FIGURE 8-3. A: Radiograph of failed THA with loose stem and long cement column. B,C: An extended greater trochanteric osteotomy facilitated cement removal. The length of the osteotomy is determined by cement extraction needs but is limited by the need to maintain a tube of diaphyseal bone for new implant fixation.
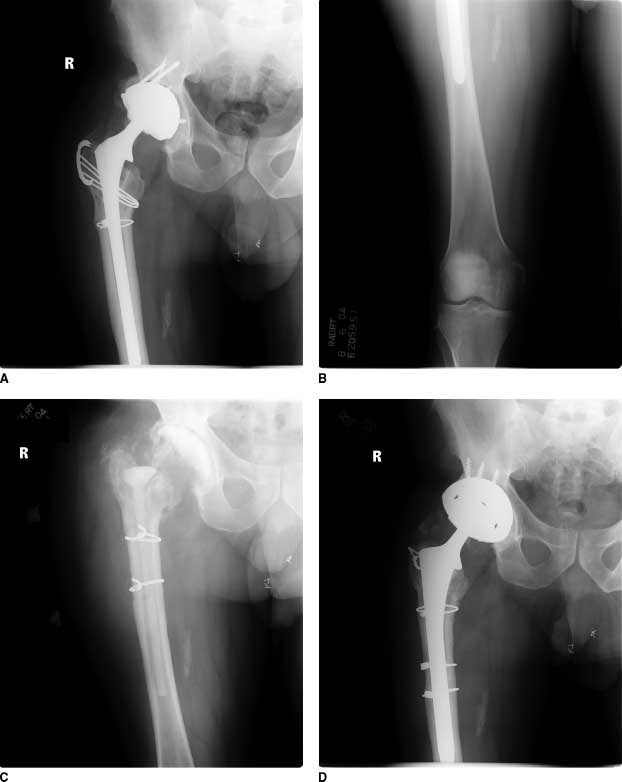
FIGURE 8-4. A,B: Radiographs of failed THA due to infection with well-fixed extensively porous-coated stem. C: An extended greater trochanteric osteotomy was performed to facilitate implant removal. D: The same exposure was used again at the time of hip reimplantation.
IMPLANT INSERTION
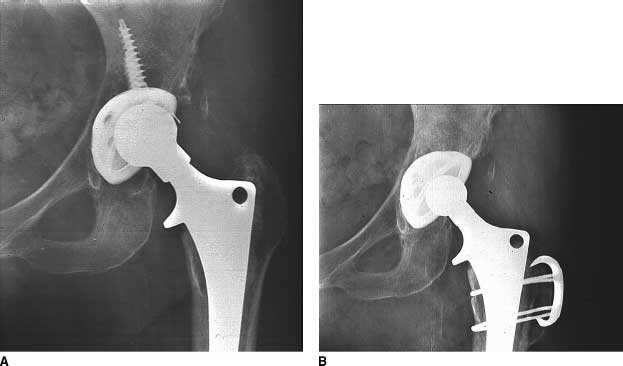
Insertion of most conventional hemispherical acetabular components can be performed through a conventional antersolateral or posterior approach. In contrast, bulky acetabular reconstruction devices (such as cages) often require extensile exposures. A conventional transtrochanteric exposure, which translates the abductors proximally, protects the superior gluteal nerve from damage during the insertion of cages that extend high onto the ilium (Fig. 8-5).

FIGURE 8-5. A: Failed THA with Paprosky Type IIIB bone loss. B: Radiograph after reconstruction with antiprotrusio cage. A conventional greater trochanteric osteotomy, which protects the superior gluteal nerve and abductors, was performed to facilitate safe implant insertion.
When posterior column pelvic plating is anticipated, an approach that allows the surgeon to gain direct access to the posterior column—either a posterior approach or a transtrochanteric approach—is advantageous.
Many conventional cemented and uncemented revision femoral components can be im-planted through a conventional anterolateral or posterior approach. However, when there is substantial femoral deformity, an extensile exposure facilitates placement of revision femoral implants (Fig. 8-6). Long uncemented implants usually can be placed more easily when an extended trochanteric osteotomy has been performed, because the osteotomy allows canal preparation and implant insertion without impingement against the proximal femur. Implantation of extensively porous-coated uncemented implants is facilitated by a lateral extended trochanteric osteotomy. Implantation of a long fluted tapered modular implants is facilitated by an anterior extended greater trochanteric osteotomy because it helps the surgeon negotiate the distal bow of the femur with a straight distal reamer and implant.
FIGURE 8-6. A: Radiograph of failed THA with marked proximal femoral deformity and broken failed stem. B,C: Radiographs after hip reconstruction. An extended greater trochanteric osteotomy was used to facilitate exposure, and after implant insertion a corrective diaphyseal osteotomy was also performed.
HIP STABILITY
When unsatisfactory soft tissue tension is anticipated after the planned hip reconstruction, the surgeon may consider a transtrochanteric approach. Transtrochanteric approaches allow advancement of the abductor complex to gain soft tissue tension and hip stability (Fig. 8-7). A trochanteric slide or a conventional trochanteric osteotomy is easiest to advance, but an extended trochanteric osteotomy also may be used for this purpose.
FIGURE 8-7. A: Radiograph of failed THA with polyethyl-ene wear, osteolysis, and well-fixed femoral component. Unsatisfactory soft tissue tension was anticipated after reconstruction. B: To gain soft tissue tension a greater trochanteric slide was used for exposure, and at the end of the procedure the greater trochanter was advanced to improve soft tissue tension.Conventional Trochanteric Osteotomy
SINGLE COMPONENT REVISION
Specific considerations apply when only the femoral component, the acetabular component, or a modular head and liner exchange will be performed.
If an acetabular shell will be retained during a femoral revision, or head and liner exchange, it is valuable to consider the anteversion of the existing acetabular shell. If the shell has little anteversion, then one may consider an anterolateral approach to the hip, which preserves the posterior capsular structures thereby reducing the risk of posterior instability. Contrariwise, if an acetabular component with much anteversion will be retained, then a posterior approach may be considered, because it will preserve the anterior soft tissues and anterior hip stability more satisfactorily.
When a femoral component will be retained during acetabular revision, in most cases either an anterolateral approach or a posterior approach can be performed successfully, provided adequate mobilization of the proximal femur can be achieved to provide access to the acetabulum. Under these circumstances specific methods are available to increase exposure (see below).
ACCESS TO THE FEMORAL SHAFT
When extra access to the femoral shaft is required for femoral plating or bone grafting, a lateral approach to the femur can be added to most of the approaches noted above. Depending on the surgeon’s preference, this involves either splitting the vastus lateralis longitudinally or reflecting the vastus lateralis in an anterior direction from its posterior attachments.4
KEEPING THE OPTIONS OPEN
For some revisions, the surgeon may initiate exposure with a conventional approach, which can be converted to an extensile exposure if needed. The initial exposure should be chosen carefully when this strategy is used, to keep desired exposure options available. A posterior approach does not limit the surgeon from performing a subsequent trochanteric slide, a conventional trochanteric osteotomy, or an extended greater trochanteric osteotomy. After an anterior or anterolateral approach, transtrochanteric exposures also may be performed; however, the vascularity of the trochanter may be compromised and healing may be less reliable. Furthermore, trochanteric advancement is less effective after anterolateral exposures because the abductors are partially detached from the trochanter.
TECHNIQUES
Posterior Approaches A conventional posterior approach is well known to most surgeons. In the revision setting, most surgeons prefer to take down a single large flap of posterior soft tissues that incorporates capsule, psuedocapsule, and short external rotators. By retracting the posterior border of the gluteus medius anteriorly, one can access more of the posterior capsule and thereby gain a larger flap of soft tissue for subsequent repair. Extra care to avoid damage to the sciatic nerve in the revision setting is warranted. In many cases the surgeon can identify the sciatic nerve in the operative field by visualization or palpation. When this is not possible, the nerve reliably can be identified beneath the gluteus maximus tendon (where typically it is surrounded by fat) and then traced proximally. Working with the knee flexed and hip extended relaxes the sciatic nerve and reduces the risk of damage. Retractors should not be placed directly against the nerve but rather padded by interposed soft tissues or sponges. A cobra-type retractor can be placed safely in the lesser sciatic notch to hold posterior structures away from the posterior column.
Posterior column plating for pelvic discontinuity or for the placement of large structural grafts involves dissecting the posterior soft tissues directly off the posterior column bone. During this process one must know precisely the position of the sciatic nerve. During posterior column plating one must also be cautious to avoid damage to the superior gluteal artery and nerve as dissection approaches the greater sciatic notch.
When the femoral component is retained, the femur must be translated anteriorly to provide access to the acetabulum. When the femur is in this position, the prosthetic femoral head or trunnion can squeeze the femoral nerve against the ilium, causing a nerve palsy. To avoid this problem, a pouch can be created against the ilium, anterolateral to the socket, in which the metal component can rest safely. The pouch is created by elevating abductors and reflected head of the rectus femoris from the ilium at the anterolateral quadrant of the acetabulum.
Closure of a posterior approach after revision hip arthroplasty should include, when possible, repair of the posterior capsule and soft tissues. Good closure of the posterior soft tissues probably reduces posterior dislocation risk by providing a check reign that limits excess femoral internal rotation and also provides a physical barrier posteriorly to resist dislocation. Usually the posterior soft tissue flap can be repaired to the posterior abductor border and to the posterior border of the greater trochanter through drill holes in bone. Care should be exercised throughout closure to avoid incarcerating the sciatic nerve with sutures.
Anterolateral Exposures
A family of related anterolateral approaches can be used for revision surgery. In most revisions it is advantageous to maintain the vastus lateralis and abductor muscle sleeve in continuity either through soft tissue or through a bone wafer.
The amount of gluteus medius reflected from the trochanter depends on the required exposure of the femur and acetabulum. In general, the more abductor that is elevated, the greater the exposure. This benefit is balanced by the fact that the more abductor that is elevated, the greater the risk the patient will limp if poor healing occurs. Extensile femoral exposure can be gained in any anterolateral approach by extending the split in the vastus lateralis distally (Fig. 8-8).
FIGURE 8-8. A,B: Ex-tended anterolateral exposure for revision THA. (Redrawn from McGann WA. Surgical approaches, Chapter 47. In: Callaghan JJ, Rosenberg AG, Rubash HE, eds. The Adult Hip. . Philadelphia, PA: Lippincott Williams & Wilkins; 2007:683–733.)
One of the most challenging aspects of revision through an anterolateral approach is gaining sufficient mobilization of the femur for good access to the femoral canal. The femur can be delivered from the wound more satisfactorily after posterior scar around the proximal femur is divided. This tissue usually is released most effectively with cautery or sharp dissection directly against the proximal femur. Excision of dense fibrous tissue and pseudocapsule in the inferior acetabular region just above the psoas tendon helps provide good access to the acetabulum. Occasionally division or recession of the psoas tendon is necessary to provide satisfactory acetabular or femoral exposure. Although psoas division is not recommended on a routine basis, there is not strong evidence that the release leads to sustained functional problems in most cases after revision.
When using an anterolateral exposure in revision, the surgeon must be particularly careful to avoid fracture of the posterior tip of the greater trochanter. The remaining abductors tether this weak bone, putting it at risk for avulsion during femoral canal preparation, prosthetic implantation, and hip reduction.
Sturdy repair of the abductors to their bed during closure is essential. Sutures passed through drill holes in the greater trochanter help provide a solid anchor for repair. If a wafer of bone has been reflected from the anterior greater trochanter, wires can be used to reattach the bone wafer. If the trochanteric bed to which the abductors will be attached is sclerotic or covered with shiny soft tissue membrane, the bed should be freshened with a burr to promote healing.
Extensile Exposures
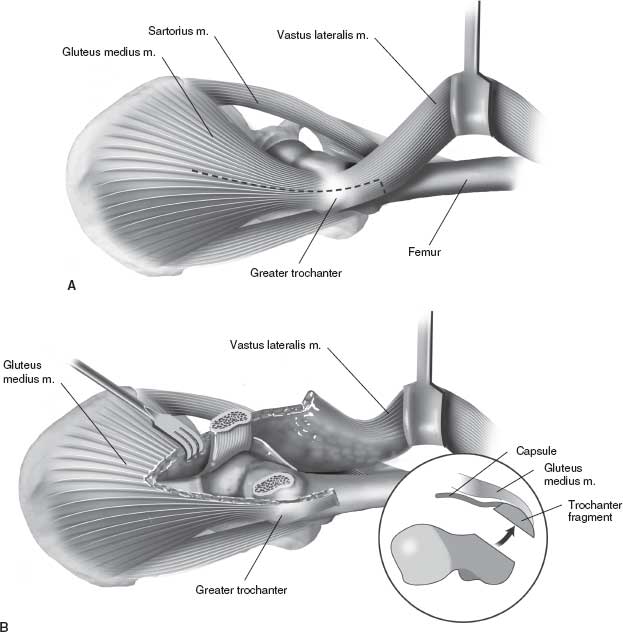
Trochanteric slide. A greater trochanteric slide is a trochanteric osteotomy that keeps the abductors, the greater trochanteric fragment, and the vastus lateralis all in continuity.5,6 Trochanteric slide can be performed after posterior exposure to the hip already has been performed, but the author prefers—when possible—to leave the posterior structures entirely intact (Fig. 8-9).7
FIGURE 8-9. Greater trochanteric slide. Note the abductors, greater trochanter, and vastus lateralis can be kept in continuity. If desired, the posterior soft tissue sleeve can be kept attached to the posterior femur, thereby preserving posterior hip stability. (Redrawn from McGann WA. Surgical approaches, Chapter 47. In: Callaghan JJ, Rosenberg AG, Rubash HE, eds. The Adult Hip. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:683–733.)
The abductors are isolated proximally, and the vastus lateralis is elevated from the femur just distal to the vastus tubercle. An oscillating saw is passed from posteriorly to anteriorly to perform the greater trochanteric osteotomy. The ideal osteotomized trochanteric fragment is approximately 1 cm in thickness. After the trochanteric osteotomy, the hip is externally rotated, the anterior and superior hip capsules are released from the femur, and then the hip is dislocated anteriorly. Completion of the exposure is performed by judiciously releasing capsule and pseudocapsule around the acetabulum and proximal femur as needed to optimize exposure.
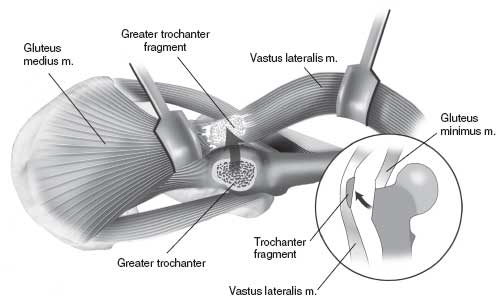
Conventional Trochanteric Osteotomy
A conventional trochanteric osteotomy provides certain benefits not provided by extended greater trochanteric osteotomies or a trochanteric slide. A conventional trochanteric osteotomy allows the abductors and trochanteric fragment to be reflected proximally, which gives greater exposure to the acetabulum and also protects the superior gluteal nerve. Like a trochanteric slide, conventional trochanteric osteotomy can be performed keeping the posterior soft tissue sleeve and soft tissues intact, thereby preserving posterior hip stability. If nonunion of a conventional trochanteric osteotomy occurs, proximal migration is more likely to occur compared to a trochanteric slide.
The vastus lateralis is divided just distal to its origin on the vastus tubercle. A saw is used to divide the greater trochanter from distal to proximal. A flat or “Chevron”-shaped osteotomy can be performed. A flat osteotomy is straightforward to perform and allows flexibility in the location of trochanteric placement at the time of repair. A “Chevron” osteotomy provides more inherent stability of the osteotomy but constrains the placement of the osteotomy at the end of the procedure. A “Chevron” osteotomy is performed by making two separate saw passes from distal to proximal so that the cut surface of the trochanteric fragment is concave and the surface of the remaining femur is convex (Fig. 8-10).
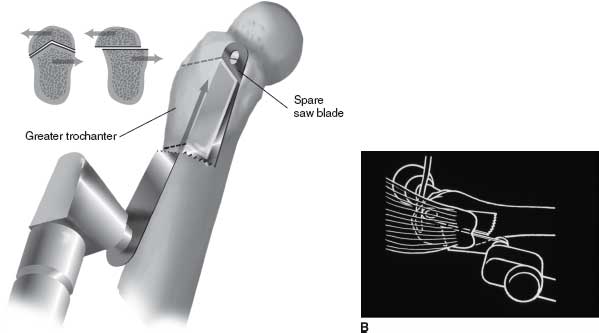
FIGURE 8-10. A: Chevron greater trochanteric osteotomy provides extra stability and resists rotation and anteroposterior translation. B: Chevron trochanteric osteotomy performed with a saw. After the first limb is made, a spare saw blade is placed to guide the second limb. (Redrawn from Berry DJ, Müller ME. Chevron osteotomy and single wire reattachment of the greater trochanter in primary and revision total hip arthroplasty. Clin Orthop 1993;294:155–161.)
For all trochanteric osteotomies, the surgeon must optimize the thickness of the greater trochanteric fragment. When there is a thick remaining host trochanter, the bed will be good and a thicker trochanteric fragment can be maintained. When the host trochanter is thinned, due to the cement or a large femoral implant, the osteotomized fragment must be kept thinner to maintain an adequate trochanteric bed. In all cases, creating an overly thin fragment risks fracture of the fragment, while creating an overly thick fragment risks leaving a poor trochanteric bed.
Repair of the trochanteric fragment is performed with wires, a cable grip, or a trochanteric claw plate.8 Wires have the disadvantages of being more cumbersome to use and being less strong than cables. However, wires cause less irritation of the soft tissues than cables. Many methods of trochanteric reattachment with wires have been described (Fig. 8-11),9,10 and union rates in revision series vary widely. Among the highest rates of success are a series by Harris and colleagues that reported a 97% union rate11 and a series of cases by Müller12 that also reported a 97% union rate. Broken wires usually cause limited irritation of the soft tissues, while fragmentation of trochanteric cables with resultant sharp ends and cable debris can cause problems, which include trochanteric bursitis, recurrent local bleeding, and accelerated polyethylene-bearing wear.13,14
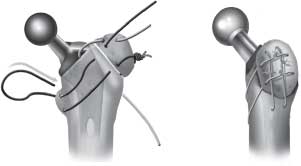
FIGURE 8-11. Four wire method of greater trochanteric attachment. (Redrawn from Yergler JD, Della Valle CJ, Silverton C, et al. Management of the trochanter, Chapter 83. In: Callaghan JJ, Rosenberg AG, Rubash HE, eds. The Adult Hip. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:1232–1256.)
Cables have the advantage of providing a very strong reattachment of the greater trochanter.15–18 If a trochanteric claw is utilized, it must fully engage the trochanter proximally to prevent trochanteric escape. It is also important to space medial cable attachment points properly to avoid a pivot point around which a claw can rotate, thereby releasing the trochanter (Fig. 8-12). In most cases, the proximal cable is passed through a drill hole in the proximal lesser trochanter, and the distal cable is passed beneath the lesser trochanter (Fig. 8-1). (Two drill holes can be used when necessary to space and position the medial cable attachment points optimally.) If a claw will not provide satisfactory fixation, a trochanteric cable plate can be considered. Vertically oriented cables placed in the coronal plane over the trochanter generally should be avoided because they create debris, which has direct access to the joint if they fail. Using a trochanteric claw and cables, McCarthy et al.16 reported a 96% union rate in revision THA when the trochanteric fragment gained bone-to-bone apposition.

FIGURE 8-12. A: The cables should not be placed too close to-gether; a “bucket-handle” effect can occur. The inferior cable is passed either inferior to the lesser trochanter distally to provide adequate spacing of the cables or through a drill hole more distally through the medial cortex. (Redrawn from Yergler JD, Della Valle CJ, Silverton C, et al. Management of the tro-chanter, Chapter 83. In: Callaghan JJ, Rosenberg AG, Rubash HE, eds. The Adult Hip. . Philadelphia, PA: Lippincott Williams & Wilkins; 2007:1232–1256.)
Extended Greater Trochanteric Osteotomy
Extended greater trochanteric osteotomy has become an essential tool of the revision hip surgeon.19–28 There are many greater trochanteric osteotomy variations. The osteotomy can involve the lateral or the anterior femur and can be performed so that the hip is dislocated either anteriorly or posteriorly. In most cases, the osteotomy is performed before the femoral component is removed, but in some cases the osteotomy is performed after the stem has been extracted.
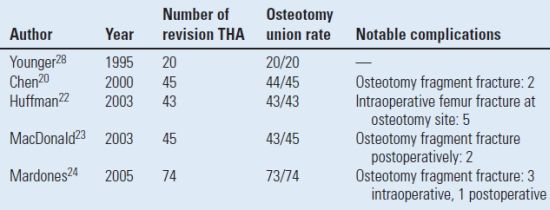
Extended osteotomies provide several important advantages in revision THA.5,29 First, they provide extensile exposure to the femoral canal for implant removal and implant insertion. Second, they have a high union rate (Table 8.1) because of the large bone contact area for healing, retention of vascularity to the fragment, and the good quality diaphyseal bone for fixation.
TABLE 8.1 Results of Extended Greater Trochanteric Osteotomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree