Olecranon Fractures: Open Reduction and Internal Fixation
James A. Goulet
Kagan Ozer
INTRODUCTION
Fractures of the olecranon constitute approximately 10% of fractures that occur about the elbow. They vary in complexity from relatively simple transverse fractures to highly comminuted and unstable fracture dislocations. Due to the wide spectrum of fracture patterns, no single method of treatment is applicable to all fractures. Olecranon fractures occur in all age groups with a bimodal injury pattern. Peaks occur in younger adults following higher injury trauma and in older patients with poor bone quality following ground-level falls. The goal of treatment in displaced fractures is to achieve stable internal fixation that allows early range of elbow motion.
The critical element in treatment of a proximal ulnar fracture is restoration of the size and shape of the trochlear notch. Small areas of comminution and minor incongruities in the transverse groove are well tolerated, since this portion of the olecranon is responsible only for limited load transmission. Although olecranon fractures frequently occur as isolated injuries, failure to recognize concomitant bone or soft-tissue injuries associated with ulnar fractures often preclude restoration of normal elbow function. Careful attention to associated injuries with repair of the lateral ligament complex, repair of the anterior capsule and coronoid process, and repair or replacement of the radial head when these structures are injured is critical for restoration of elbow function. Evaluation of fracture displacement, comminution, and ulnohumeral instability determines the method of surgery to be used to treat olecranon fractures.
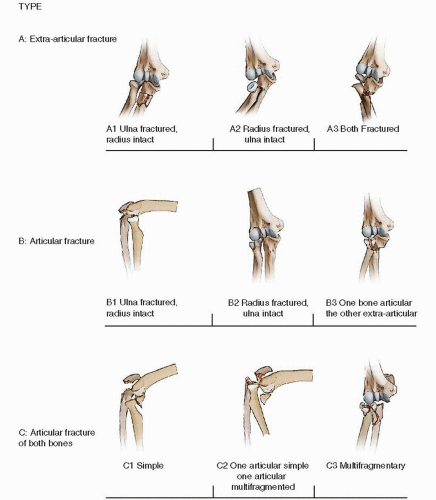
There are a large number of classifications for olecranon fractures that have been described. Colton devised a simple descriptive system that is still widely employed. Both the Schatzker and Mayo classifications are descriptive based on the fracture pattern and a consideration of the type of internal fixation required (2,4,15). The AO/OTA classification is probably the most widely used in North America (Fig. 10.1).
INDICATIONS AND CONTRAINDICATIONS FOR SURGERY
Nondisplaced and very minimally displaced fractures (<2 mm) can be treated nonoperatively if the triceps mechanism remains intact. Patients who can actively extend their elbow against gravity can usually be treated nonoperatively. These injuries are treated in a well-molded long arm cast, which is converted to a removable splint, and gentle active motion is initiated 2 to 3 weeks after injury.
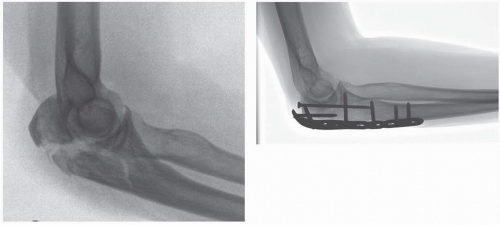
Most displaced olecranon fractures require surgical treatment (Fig. 10.2). Treatment alternatives include simple tension band wire fixation, fixation with plates (with or without locking screws), and olecranon excision with triceps advancement (1, 2, 3, 4, 5, 6, 7, 8, 9, 10 and 11). Treatment is influenced by the size of the olecranon fragment, the degree of comminution, and the bone quality. Because the olecranon and proximal ulna are subcutaneous in location, low-profile implants are important to reduce the incidence of painful prominent hardware.
 FIGURE 10.2 A displaced olecranon fracture with disruption of the extensor mechanism and articular surface. This is a very strong indication for surgery. |
Tension band wire fixation is reserved for simple transverse fractures and most noncomminuted injuries, which constitute the majority of olecranon fractures (Fig. 10.3). Tension band wiring is contraindicated in comminuted fractures as it cannot preclude shortening with this technique. In these fractures and those associated with ulnohumeral instability, plates and screws often provide better fixation (Fig. 10.4). Conventional nonlocking plates are adequate for fractures in younger patients with good bone quality and no fracture gaps. Comminuted length-unstable fractures, in patients with poor bone quality, and olecranon fractures associated with radial head or coronoid fractures are treated with locked plates. In the past decade, precontoured periarticular proximal ulnar-locking plates have been developed and can be very helpful.
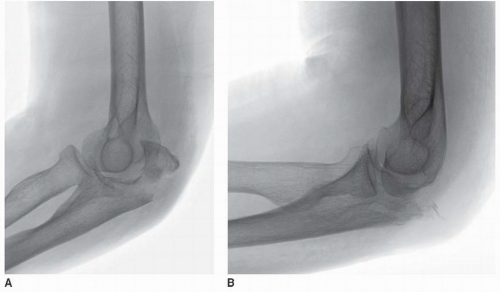
Olecranon excision with triceps advancement is used occasionally in patients with small comminuted fractures that do not affect elbow stability (5,12,13). Most are elderly patients with significant osteoporosis (Fig. 10.5A,B). Olecranon excision is contraindicated for fractures distal to the semilunar notch or for fractures
associated with ligamentous instability. In young patients, avulsion of the triceps tendon from the olecranon or contaminated open fractures with crush injury of the proximal olecranon are best treated with excision and reattachment of the triceps tendon.
associated with ligamentous instability. In young patients, avulsion of the triceps tendon from the olecranon or contaminated open fractures with crush injury of the proximal olecranon are best treated with excision and reattachment of the triceps tendon.
PREOPERATIVE PLANNING
History and Physical Exam
A careful history and physical exam should be performed on all patients with an elbow injury. The history should identify the mechanism of injury (low vs. high energy, ballistic injury, etc.), pertinent comorbidities (diabetes mellitus, cardiac problems, etc.), pertinent past surgical history, medications, and drug allergies. Hand dominance should also be established. The physical exam must evaluate and document objective findings such as swelling, ecchymosis, open wounds, neurologic status, and peripheral pulses. Patients with minimally displaced olecranon fractures should be evaluated to determine if active elbow extension is present, because it is an important criterion for nonoperative treatment. A full trauma workup using Advanced Trauma Life Support (ATLS) protocols is necessary in patients with high-energy trauma, patients with complex associated injuries, patients who are obtunded, and patients who have a head injury.
IMAGING STUDIES
In patients with suspected elbow injuries, an anteroposterior (AP) and lateral radiographs should be obtained. Due to pain associated with positioning of the elbow, high-quality orthogonal radiographs are often difficult to obtain in the conscious patient. Traction films with light sedation can be helpful for evaluation of complex fractures in a cooperative patient. In some patients, optimal films cannot be obtained until the patient is anesthetized in the operating room. Based on the physical examination, x-rays of the entire humerus or forearm may be indicated. Computed tomography scans are not usually necessary for isolated olecranon fractures and are most often used for olecranon fractures associated with articular impaction, radial head or coronoid fractures, or fracture dislocations. There are very few indications for magnetic resonance imaging scans.
TIMING OF SURGERY
The timing of surgery for olecranon fracture fixation is determined by the status of the soft tissues. With open fractures, irrigation and débridement should be performed as soon as the patient’s condition and institutional resources permit. Immediate internal fixation may be beneficial for Grade I and II open fractures, in patients who are hemodynamically stable. In patients with highly comminuted fractures associated with grossly contaminated wounds, splinting or external fixation is preferred with sequential débridements followed by delayed
internal fixation. If a vascular injury is present, exploration, repair, and external fixation should be performed urgently in collaboration with a vascular surgeon. Low-velocity gunshot wounds without a neurovascular injury are treated with local wound care, antibiotic administration, and fracture stabilization if indicated. For closed olecranon fractures, internal fixation is performed electively when the soft tissues permit. Because the olecranon is a subcutaneous bone, soft-tissue abrasions may require local skin care prior to internal fixation.
internal fixation. If a vascular injury is present, exploration, repair, and external fixation should be performed urgently in collaboration with a vascular surgeon. Low-velocity gunshot wounds without a neurovascular injury are treated with local wound care, antibiotic administration, and fracture stabilization if indicated. For closed olecranon fractures, internal fixation is performed electively when the soft tissues permit. Because the olecranon is a subcutaneous bone, soft-tissue abrasions may require local skin care prior to internal fixation.
SURGICAL TACTIC
Following a careful preoperative assessment of the patient and a critical review of the injury radiographs, a treatment plan is developed. This determines what should be available in the operating room if surgery is required. For simple, noncomminuted transverse fractures, the surgeon should plan to have 18-gauge stainless steel wire, Kirschner (K) wires, and/or 4.5- or 6.5-mm cannulated screws for intramedullary fixation, a battery-powered drill, and a no. 14 gauge angiocath to pass the wire beneath the triceps tendon. Small and medium pointed reduction clamps should also be available.
More complex fractures require a wider array of equipment. Standard “small fragment” implants and instrument sets are requested for plate fixation of fractures distal to the semilunar fossa. Fracture-specific periarticular olecranon-locking plate sets should also be available for comminuted olecranon fractures or when bone quality is poor. With high levels of comminution, provision should be made for “minifrag” 2.0-, 2.4-, and 2.7-mm plates and screws.
A proximal radial prosthesis should also be available when a displaced radial head or neck fracture is present. Suture anchors are indispensable when ligamentous instability is suspected.
SURGERY
Either regional or general anesthesia can be utilized. The patient is placed in a supine position. A nonsterile tourniquet is applied to the upper arm. To facilitate visualization and stability, the table is tilted obliquely toward the patient’s noninjured side. Surgery is performed with the forearm placed across the chest, with a supportive bolster placed beneath the proximal forearm (Fig. 10.6A). When an assistant is not available, the wrist may be secured with a sterile Kerlex (Kendall Healthcare Products, Mansfield, MA) and attached to a weight on the patient’s contralateral side. When an assistant is available, it is their job to support the arm. Flexion of the elbow can be adjusted by varying the height of the support under the proximal forearm. For simple fractures, fracture reduction
often can be achieved with the elbow in 90 degrees of flexion, but most complex fractures require the freedom to freely flex and extend the elbow. Some surgeons prefer placing the patient either in a lateral or in a prone position. However, supine positioning minimizes setup time, limits the complexity of anesthetic monitoring, and accommodates management of patients with multiple injuries who cannot be positioned either lateral or prone.
often can be achieved with the elbow in 90 degrees of flexion, but most complex fractures require the freedom to freely flex and extend the elbow. Some surgeons prefer placing the patient either in a lateral or in a prone position. However, supine positioning minimizes setup time, limits the complexity of anesthetic monitoring, and accommodates management of patients with multiple injuries who cannot be positioned either lateral or prone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree