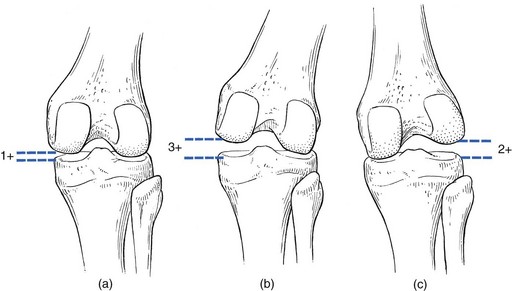
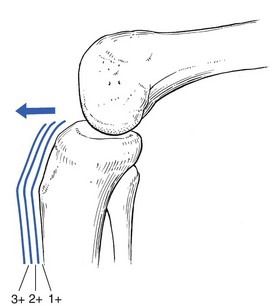
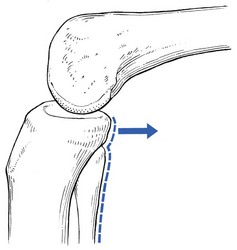
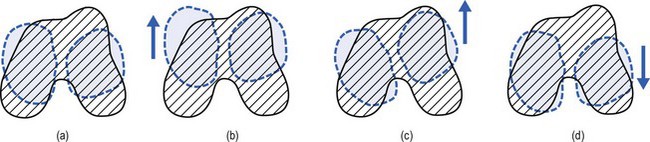
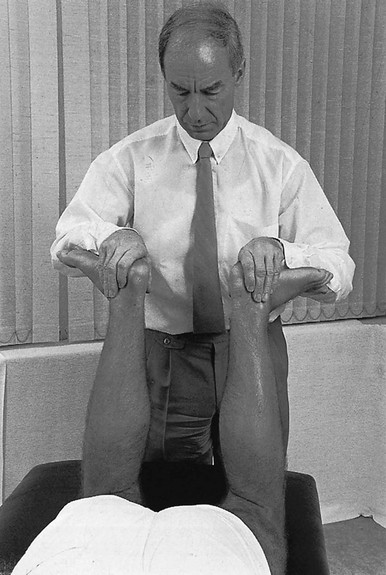
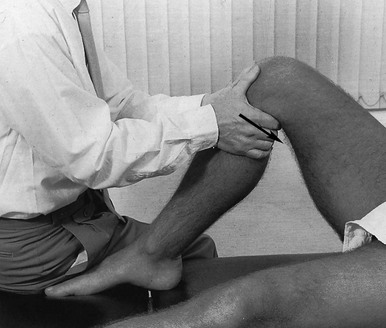
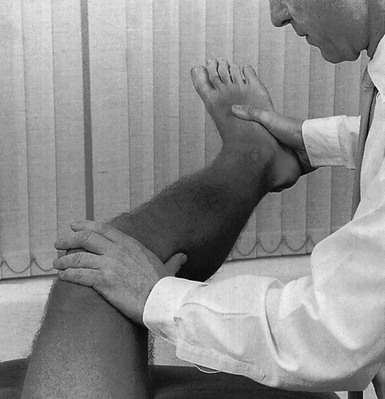
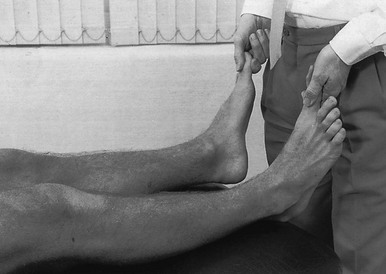
If the history indicates that there is possibly instability, an examination to detect the exact location and degree of this is performed. It is important to make this supplementary examination only when symptoms and signs found in the routine clinical assessment indicate ligamentous instability to be the cause of disability. Indeed, it is important to realize that not every lengthened ligament leads to problems.1 If the athlete’s muscles are strong enough to provide dynamic stability, a slightly unstable knee will not cause trouble. Conversely, it is quite possible that an athlete with slight laxity of one or more ligaments has a chronic painful lesion as well. If the diagnosis of the latter is missed because the routine functional examination is not performed, it may well be that the patient is sent for surgery, which will solve the slight instability but does not cure the main problem. Knee instability is the result of loss of static and dynamic function. Stability depends on the tautness of the ligaments, congruency of joint surfaces, effectiveness of the menisci and the well-balanced action of all musculotendinous units acting across the knee joint. Of these structures, muscles and tendons play a central role in joint stabilization. They are said to be the ‘first defenders’ in distortion and loading situations.2 The degree of instability is demonstrated during stress tests and can be graded on the following scale (Fig. 1): • mild/1+ = 5 mm or less separation of joint surfaces • moderate/2+ = between 5 and 10 mm separation Instability may be classified as straight or rotatory. This is defined as an increased range of angular movement in the frontal plane, i.e. valgus/abduction or varus/adduction movement (Fig. 2), or an increased range of gliding movement in the sagittal plane, i.e. the simultaneous forward or backward gliding movement of the tibial condyles in relation to the femoral condyles (Fig. 3). This implies increased rotation movement of the tibia on the femur. The posterior cruciate ligament, located in the centre of the joint, is the fundamental stabilizer and is the axis of the joint, both in flexion–extension and in rotation. Consequently, this ligament is always intact in rotatory instabilities; from the moment the ligament is completely torn, there is no longer a centre of rotation and any kind of straight instability can result.3,4 There are three types of rotatory instability: • Anteromedial rotatory instability: there is an abnormal forward gliding movement of the medial tibial plateau with respect to the medial femoral condyle, while the lateral tibial plateau retains a relatively normal relationship with the lateral femoral condyle (Fig. 4b). • Anterolateral rotatory instability: there is an abnormal forward gliding movement of the lateral tibial plateau with respect to the lateral femoral condyle, while the medial tibial plateau retains a relatively normal relationship with the medial femoral condyle (Fig. 4c). • Posterolateral rotatory instability: there is an abnormal backward gliding movement of the lateral tibial plateau with respect to the lateral femoral condyle. Again, as in anterolateral rotatory instability, the medial tibial plateau remains in normal contact with the corresponding femoral condyle (Fig. 4d). The patient is placed supine on the couch, the head resting on a pillow to enable observation of the examiner without active raising of the head (which often causes tightening of the hamstrings). The thigh rests on the couch and the lower leg hangs over the side, with the knee in 30° of flexion. One hand is placed about the lateral aspect of the knee, the other grasps the lower leg at the ankle (Fig. 5). Then abduction stress is applied gently and repeatedly, gradually increasing up to the point of pain. The degree of movement and the end-feel are estimated. This test is performed in the same position as the previous one, but the hands are changed; so one hand is placed about the medial aspect of the knee while the other grasps the lower leg at the outer side of the ankle (Fig. 6). The degree of movement and end-feel are estimated. The test is performed with the patient supine and the knee in 20–30° of flexion. The distal femur is grasped from the lateral side to obtain control just above the lateral femoral condyle. The examiner uses the opposite hand to displace the proximal tibia directly anteriorly (Fig. 7). In acute rupture of the anterior cruciate ligament this test is preferred to the anterior drawer test in the 90° flexed position because muscle defence by the hamstrings may prevent the forward movement of the tibia and give rise to a false-negative result.5 Liljedahl et al6 found only 3 of 35 patients to have a positive anterior drawer test in 90° of flexion, whereas with anaesthesia 31 and on arthrography 29 were positive. The test is first performed with the lower leg and foot externally rotated beyond the neutral position and as far as is comfortably possible, then internally rotated (Fig. 8). Sometimes doubt remains as to whether the range of rotation has been increased. A decisive assessment can be made with the patient prone and the knees flexed to a right angle (Fig. 9). The movement of external or internal rotation is performed bilaterally and the range of movement is assessed by the twisted position of the feet. The patient is in supine position with the hip flexed to 45° and the knee to 90°. The foot is flat on the couch, in neutral position. The heels of both hands are placed anteriorly against the proximal part of the tibia (Fig. 10). Both thumbs at the anterior border of the joint can estimate the range of movement. The proximal part of the tibia is then pushed backwards repeatedly, first gently then with a strong jerk. The posterior drawer test, which includes palpation of the tibia–femur step-off, was recently demonstrated to be the most sensitive and specific clinical test for posterior cruciate ligament deficiency (accuracy 96% with a 90% sensitivity and a 99% specificity).8 The patient lies supine, the hip flexed to about 45°, the knee to 90°. The examiner supports the patient’s leg, with one hand at the foot, the other at the proximal end of tibia and fibula. The hand at the foot rotates the tibia slightly internally while the other hand exerts a mild valgus stress at the knee (Fig. 11). Extreme internal rotation may dampen a shift significantly. Maintaining slight internal rotation and mild valgus stress, the examiner gradually extends the knee. The test demonstrates an anterolateral rotatory instability because of a tear in the middle third of the lateral capsular ligaments. Frequently, the anterior cruciate ligament and/or menisci are also ruptured and increase the instability.9 Bach et al10 found that the degree of pivot shift, probably because of the role of the iliotibial band, strongly correlates with the position of the hip and knee joint. They advised 30° of hip abduction and 20° of tibial external rotation as the position in which instability is most clearly demonstrated. The patient lies supine on the couch. Both legs are lifted simultaneously by grasping the big toes (Fig. 12). The amount of external rotation of the proximal end of the tibia and the degree of recurvatum are observed. In a positive test, unilateral excess of external rotation and recurvatum is obvious, which is seen as increased tibia vara. Clinical tests for knee instability are summarized in Table 1. Table 1 Summary of clinical tests for instability
Disorders of the inert structures
Ligamentous instability
Ligamentous instability
Types of instability
Degree of instability
Classification of instability
Straight instability
Rotatory instability
Functional examination
Tests
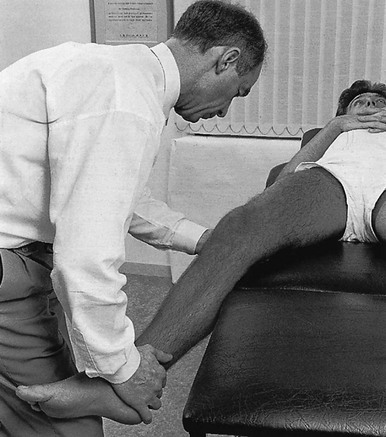
Passive abduction or valgus stress test in 30° of flexion
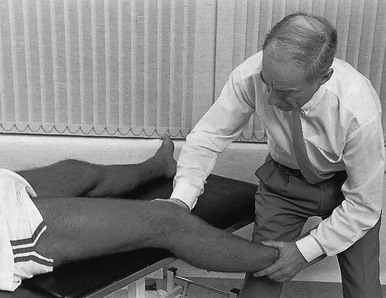
Passive adduction or varus stress test in 30° of flexion
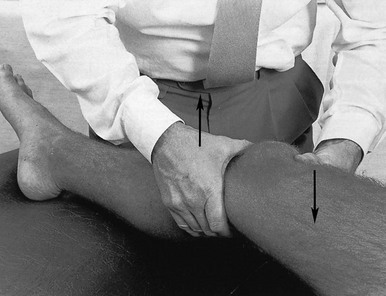
Lachman test
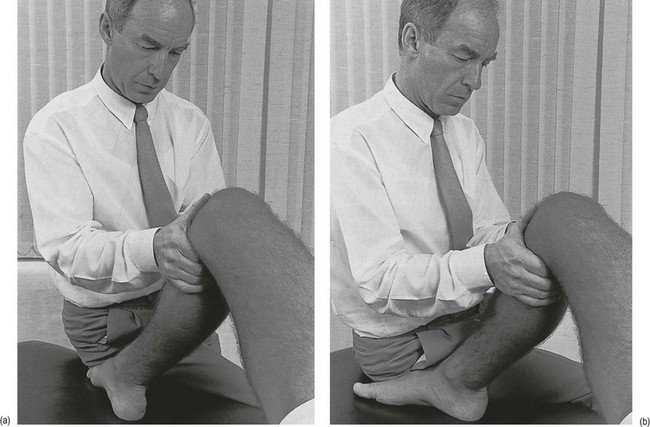
Anterior drawer test in external and internal rotation
Prone rotation test7
Posterior drawer test
‘Jerk’ test and pivot-shift test
External rotation–recurvatum test
Type of instability
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access