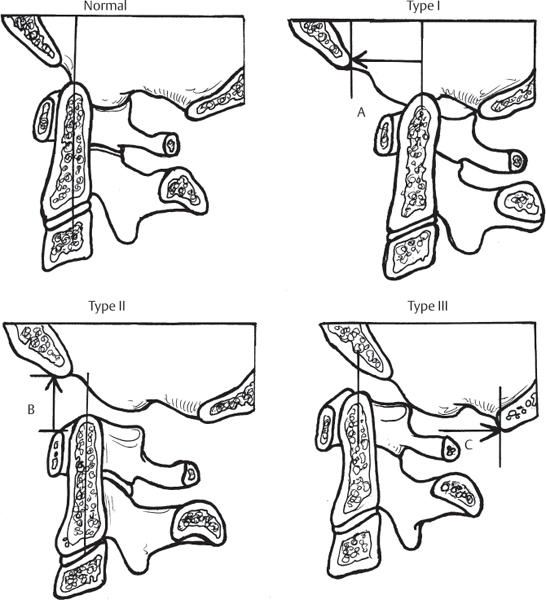
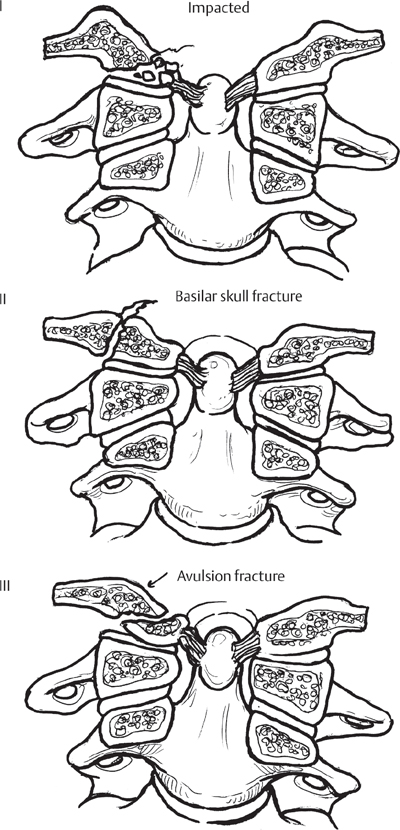
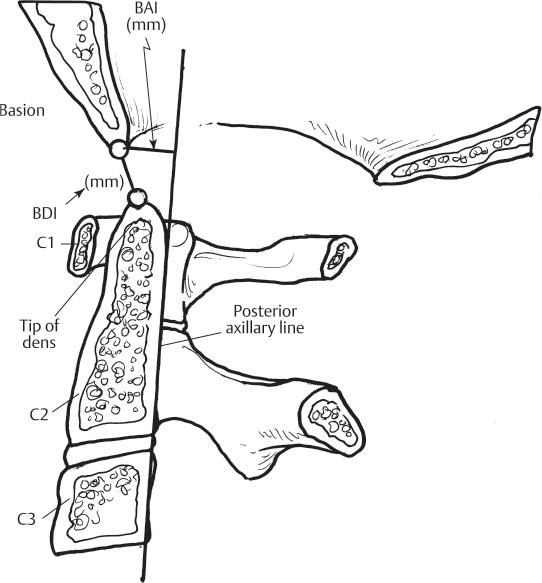
1 Injuries at the occipito-atlantal (OA) junction exist on a spectrum, from simple posterior ligamentous strain to fracture of the occipital condyles and true OA dissociation, which represents the complete disruption of the osseo-ligamentous complex of the OA joint. OA dislocations manifest as varying degrees of subluxation, or disarticulation, of the occipital condyle(s) from the articular surface of the first cervical vertebra (atlas). These injuries are often precipitated by massive forces applied across the OA junction and usually result from high-speed motor vehicle accidents, falls from substantial heights, or accidents in which a pedestrian is struck by a motor vehicle. OA dislocation/dissociation in particular is feared because of high associated rates of neurologic injury and mortality. Until recently, OA dislocations were considered uniformly fatal, but, thanks to advances in emergency medical response and scientific understanding regarding these injuries, successful interventions and cases of OA dissociation without neurological deficit have recently been reported. Occipital condyle fractures were classified in the system described by Anderson and Montesano (Fig. 1.1). In this classification, type I and II fractures are considered stable, while type III fractures may be unstable because of compromised ligamentous structures. Tuli and colleagues attempted to derive a classification of occipital condylar injuries that is more capable of informing outcome. In this system, type 1 fractures are nondisplaced, type 2a fractures are displaced but stable because ligamentous structures are competent, and type 2b fractures are displaced and unstable secondary to compromised ligaments. OA dislocations were initially classified by Traynelis et al. in a purely descriptive system based on the direction of displacement (Fig. 1.2). This classification has been criticized on the grounds that it does not inform treatment or outcome and that in severe OA dissociations, hypermobility may enable a single patient to be classified in all three categories depending on the location of the occiput at the time various imaging studies are obtained. Recently, Bellabarba et al. and Horn et al. have both derived newer schemes intended to inform treatment of OA dislocations. Both classifications employ computed tomography (CT) and magnetic resonance (MR) imaging (MRI), and the system of Bellabarba et al. also employs provocative traction. In Bellabarba et al.’s classification, type I injuries are aligned within 2 mm of normal by CT and distract < 2 mm with provocative traction, type II dislocations distract more than 2 mm, and type III injuries are grossly misaligned on CT imaging alone. Horn et al. employ a more simple system in which type I injuries are considered stable and type II injuries are unstable. To be considered stable in the system of Horn et al., a patient’s CT must be essentially normal at the OA junction, and any evidence of ligamentous injury in the posterior structures, or OA joints, solely detectable by MRI. Fig. 1.1 Classification system for OA dislocations. Type I dislocations have anterior displacement. Type II dislocations have vertical (upward) displacement of the occiput from the atlas (OA dissociation). (Note: Some authors have divided these into type IIa and IIb, in which the latter has vertical separation of the atlas from the axis; however, this is more accurately categorized as atlanto-axial instability and is discussed in Chapter 3.) Type III dislocations are posteriorly displaced. Fig. 1.2 Classification system for occipital condyle fractures as described by Anderson and Montesano. Type I fractures are considered impaction fractures and are stable. Type II fractures are basilar skull fractures that extend through the condyle and communicate with the foramen magnum. These are also usually stable. Type III fractures are unstable, as they are avulsion fractures that primarily represent ligamentous incompetence. OA injuries must be suspected in individuals who have suffered high-energy accidents and in those with cranial or cervical injuries and associated respiratory distress, neurological deficits, obvious cranial nerve injury, and/or sympathetic disruption. Because of the substantial force required to precipitate an OA dislocation, patients with these injuries often present intubated, with multisystem trauma. The initial detection of an OA injury may be delayed in patients in extremis from other injuries, patients who are already intubated and require mechanical ventilation, and patients for whom a full neurological examination is not possible. Patients with isolated occipital condyle fractures usually present without neurological injury. The main complaint in these situations is pain localized to the occipital region. All patients should receive a complete neurological evaluation, including rectal exam and evaluation of the bulbocavernosus reflex. Those patients suspected of having an OA dislocation should also undergo a rigorous examination of the cranial nerves, as deficits of these nerves may be present in as many as 40% of patients (cranial nerves IX, X, and XII are commonly involved in the event of condylar fractures, whereas VI, X, and XII are often reported in the setting of OA dislocations). Patients who are awake and cooperative may complain of pain in the occipitocervical region and have reproducible symptoms with palpation. If an OA dislocation is suspected, sandbags should be used for head immobilization during the initial evaluation. A cervical collar should be avoided, as it can distract the damaged OA joint. Once an OA dislocation has been confirmed by imaging, halo immobilization can be applied as a temporary means of stabilization. Axial traction should be avoided because it recreates the mechanism of injury and may lead to further neurological injury. Initial plain-film images and/or CT scans performed as part of the standard trauma evaluation should be obtained in all patients suspected of OA injuries. Condylar fractures are most commonly identified by CT examination but may be evident on plain radiographic imaging, particularly the open-mouth odontoid view. Lateral plain-film radiographs and sagittal CT reconstructions of the OA junction should be scrutinized using the basion–dental interval (BDI) and basion–axial interval (BAI) described by Harris and colleagues (Fig. 1.3). Neither of these parameters should exceed 12 mm on lateral plain film or sagittal CT of the OA junction. A recent study has correlated poor prognosis for survival with BDI > 16 mm. Recently, Pang et al. advocated the use of occipital condyle–C1 interval (CCI) as the diagnostic gold standard for OA dislocation. These authors maintained that a CCI > 4 mm has the highest diagnostic sensitivity and specificity for dislocations and is the only radiographic parameter interrogating the actual joint compromised in OA injuries. Additionally, widening of the CCI is not influenced by patient positioning or the location of the occiput during imaging studies. MR imaging is often used as an adjunct to CT or as a means to detect ligamentous injury at the occipitocervical (OC) junction when CT scan is normal and “autoreduction” of an OC dislocation is suspected. Edema within the OA joint on MRI is a hallmark of capsular injury, as is disruption of the tectorial membrane or alar ligaments. Fig. 1.3 Radiographic examination of the occipitocervical (OC) junction can be challenging. Harris et al. described the basion–axial interval (BAI) and the basion–dental interval (BDI). The BDI is measured from the tip of the odontoid process (dens) to the basion (anterior portion of the foramen magnum). The BAI is measured from the basion to a line drawn perpendicular to the body of the axis (C2). If these intervals are greater than 12 mm, an OA dislocation should be highly suspected.
Occipito-Atlantal Injuries
![]() Classification
Classification
![]() Workup
Workup
History
Physical Examination
Spinal Imaging
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







