26. Obstetric and neonatal infections
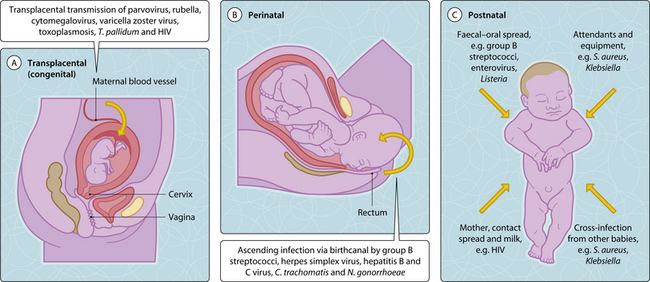
Both the pregnant woman and the newborn infant are to some extent immunocompromised. Most infections in pregnancy are not more common (an exception is urinary tract infection) but are more likely to be severe (particularly chickenpox, viral hepatitis and malaria). Primary infection in the mother induces IgM antibodies but these do not pass through the placenta to the fetus. Intrauterine infection may result in fetal death and spontaneous abortion or congenital infection and associated malformations. The baby may also acquire infection around the time of birth (perinatal infection) or after birth (postnatal infection) (Fig. 3.26.1). Puerperal infections are postnatal infections in the mother.
Congenital infections
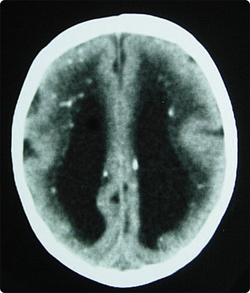
Most congenital infections may also cause spontaneous abortion. TORCH is an acronym for the infections of toxoplasma, rubella, cytomegalovirus and herpes simplex. It is a useful aide mémoire but is by no means all inclusive. Acute maternal Toxoplasma gondii infection is usually asymptomatic; however it can cause transplacental infection of the fetus. Primary toxoplasmosis in pregnancy can result, in a minority, in congenital damage with hydrocephalus, intracranial calcifications and chorioretinitis (Fig. 3.26.2). The diagnosis can be confirmed by amniocentesis; antiparasitic therapy needs to be continued in infancy. Most infants who are infected while in the womb have no symptoms at birth but may develop symptoms later in life.
Infections causing skin rashes and carrying a risk for congenital infections if they occur in pregnancy comprise rubella virus (German measles), varicella zoster virus (VZV; chickenpox) and parvovirus. Primary maternal rubella infection in the first trimester carries a high risk of congenital rubella syndrome (microcephalus, cataract, deafness and heart defects) in the fetus, resulting in termination of pregnancy in many cases. Vaccination in childhood has been introduced for prevention. Primary VZV infection in the first 20 weeks of gestation can cause congenital varicella syndrome (eye defects, hypoplastic limb, microcephalus), but in less than 2% (Fig. 3.26.3). VZV infection around delivery can cause neonatal varicella syndrome (rash, pneumonitis) and severe maternal varicella zoster pneumonitis, which can be treated with high doses of intravenous aciclovir. Giving VZV immunoglobulins to mother or neonate within 7 to 10 days of exposure may prevent fetal and neonatal varicella zoster syndrome. Parvovirus infections during the first 20 weeks of gestation cause fetal anaemia and hydrops in less than 10%, and can be diagnosed by cordocentesis and monitoring for fetal ascites.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree