Fig. 7.1
The right foot is fixed but becomes unloaded as the athlete shifts his weight and forward momentum to his left leg. The right knee is minimally flexed and sustains a relative external rotation twist while the body and the right femur are anteriorly translating and internally rotating
PCL injuries are more commonly found in conjunction with other ligamentous injuries. Shelbourne et al. identified a combined PCL-medial collateral injury (MCL) in patients who had sustained a valgus external rotation force to a flexed knee with a planted but nonweightbearing foot (Fig. 7.2) [10]. This injury typically occurs when the foot gets stuck on a surface or in a hole, the weight is on the other leg, there is valgus stress on the knee, and the tibia is externally rotated. The injured MCL is easily recognized but the PCL can be slight and often missed on physical examination.
Fig. 7.2
Combined PCL –MCL injuries can occur when the foot is planted or fixed, but not weight bearing, and the leg is either struck on the lateral side (a) or the foot being stuck causes a valgus stress with external rotation of the tibia (b). PCL posterior cruciate ligament, MCL medial collateral injury
PCL injuries in conjunction with a dislocated knee, either medial or lateral, can have varying degrees of injury and subsequent laxity and have implications for treatment. When the injury occurs as a result of major trauma, as in the case with automobile accidents, the more serious injuries to the rest of the body take precedence in emergency care. The injury to the PCL may not be recognized or addressed until the patient later has symptoms affecting function. Given that the PCL injury is frequently overlooked, the incidence of the injury with major trauma may never be known.
Therefore, an understanding of the mechanisms of injury for PCL injuries, whether isolated or combined with other knee structures, will raise suspicion for the injury and proper examination techniques will lead to an accurate diagnosis and appropriate management.
Clinical Diagnosis/Physical Examination
As previous stated, being suspect of PCL injury by understanding the mechanisms of injury is very important for diagnosing a PCL injury. With an isolated injury to the PCL, the patient usually feels the injury was significant but perhaps not debilitating. The patient can usually bear weight but may walk with a slightly flexed knee, avoiding terminal extension and external rotation. In contrast to anterior cruciate ligament (ACL) tears, the patient usually denies hearing or feeling a “pop” and the presence of an effusion may be minimal. Most isolated PCL injuries seen acutely after the injury are accompanied by posterior knee pain, a mild hemarthrosis and difficulty squatting. The patient will often report that “something is not right” in the injured knee, but cannot elaborate on what feels wrong.
If the knee injury includes a PCL injury with other ligaments injured, the swelling is usually much greater. Patients with PCL/MCL injuries have the symptoms of an isolated MCL injury, with pain and tenderness on the medial side of the knee and a feeling of medial instability in the knee. The patient may have localized swelling along the ligament. If the PCL injury is part of a knee dislocation with ACL and either medial or lateral collateral ligament (LCL) injuries, the patient will have a significant hemarthrosis. If there has been a significant capsular injury, swelling may dissect into the subcutaneous tissues resulting in the development of edema and ecchymosis in the leg below the knee. The main concern with multiple ligament dislocations is the possibility of neurovascular injury. Careful assessment must be made of the vascular and neurologic status of the limb, and consultation with a vascular surgeon may be required. Patients with ACL, PCL, and lateral-side knee injuries have an almost 30 % incidence of peroneal nerve injury [11].
If not seen acutely after a PCL injury , many of the patient’s symptoms will resolve and activities can be resumed without the patient knowing of the injury. Patients usually will not seek treatment unless they develop chronic knee symptoms, with pain being the most common complaint [1, 12]. Instability is usually a secondary complaint in about 20–45 % of patients with chronic PCL-deficient knees [1, 12].
Physical Examination
Physical examination serves to confirm the diagnosis suspected from the patient’s history. Physical examination of the acutely injured knee can be difficult due to pain, swelling, muscle spasm, limited range of motion (ROM), and patient apprehension. The normal, uninjured knee should be examined first so that a normal baseline for the patient can be determined by the examiner for all parameters, including knee stability. An examination of the normal knee allows the patient to know what to expect when the clinician examines the injured knee and may instill some confidence in the patient, allowing them to relax somewhat, thus making the examination a little easier.
The best physical examination test for diagnosing PCL injuries has been found to be the posterior drawer test, which was found to be 96 % accurate, 90 % sensitive and 99 % specific with an interobserver agreement for the grade of injury of 81 % [13]. The posterior drawer examination is performed with the knee bent at 90° of flexion. The examiner places his leg over the patient’s toes so the patient can relax the leg and the foot is stabilized on the examination table. The examiner places both hands on the front of the tibia with the thumbs over the femoral condyles. Force is applied and directed posteriorly to evaluate posterior excursion (Fig. 7.3). Posterior laxity is graded as described in Table 7.1, with grade 2 laxity indicating that the tibia is flush with the femoral condyles. Translation greater than 13 mm is classified as a grade 3 injury, which usually indicates that other knee ligamentous injuries are present.
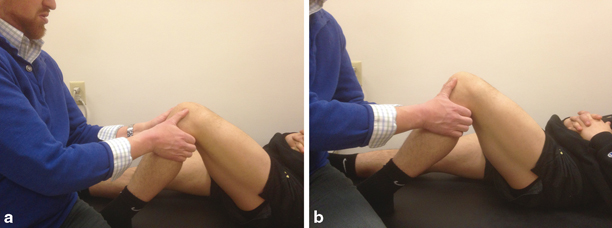
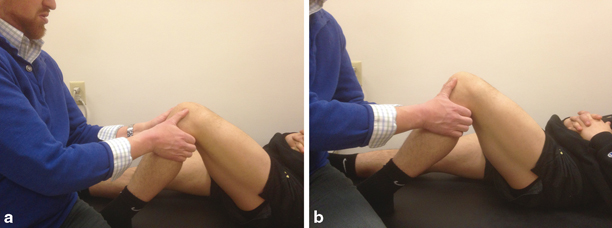
Fig. 7.3
Posterior drawer test: The patient is supine and has the hip and knee flexed to about 90°. The examiner sits at the edge of the patient’s foot so the foot cannot slide on the exam table. This allows the patient to relax his/her leg completely. The examiner places his/her hands so that the thumbs can feel for the normal prominence of the tibia in relation to the femoral condyles (a). The index fingers can be used to feel for relaxation of the hamstring muscles. The examiner pushes directly posterior on the tibia and feels for translation of the tibia and the loss of normal prominence of the tibia. When the tibia is completely flush with the femoral condyles upon posterior force, the patient has 2 + posterior laxity (b)
Table 7.1
Grade of posterior cruciate ligament laxity as evaluated with posterior drawer examination
Grade | Difference on posterior drawer (mm) | Anatomical landmarks |
|---|---|---|
1 | 3–5 | Tibial plateau prominence remains anterior to femoral condyles |
1.5 | 6–8 | Tibial plateau prominence not quite flush with the femoral condyles |
2 | 9–10 | Tibial plateau and femoral condyles lie flush |
2.5 | 11–13 | Anterior tibial plateau is slightly posterior to the femoral condyles |
3 | > 13 | Anterior tibial plateau is grossly posterior to the femoral condyles |
The accuracy of the posterior drawer exam comes with experience. If the posterior drawer exam becomes a part of the regular routine of a thorough knee examination for any patient with a knee injury, the clinician gains experience for feeling differences in PCL laxity and the feel of an endpoint of stability. If the patient’s knee cannot be bent to 90° due to significant injury or swelling, one can reexamine the patient a few days later to give time for the initial pain and swelling to subside.
With both knees bent to 90° for the posterior drawer exam, the clinician can also observe for posterior sag of the tibia in the involved knee compared with the normal knee (Fig. 7.4). With an intact PCL , the anteromedial proximal tibia will be about 1 cm anterior to the distal femoral condyles. When the PCL is injured with laxity, the proximal tibia will sag to varying amounts related to different degrees of PCL injury . The traditional way for looking for posterior sag is with both the hips and knees flexed to 90°. The clinician can observe the knees from the patient’s side, and this method has the added advantage of gravity for producing sag of the tibia. However, this method may cause more pain for a patient with an acute PCL injury and may not be possible. Other tests to assess clinical integrity of the PCL include the reverse Lachman test, the dynamic posterior shift test [14], and the quadriceps active drawer test [15].


Fig. 7.4
Posterior sag: The knee in the foreground shows posterior sag of the tibia compared with the normal knee that can be seen with PCL injury.PCL posterior cruciate ligament
When a multiple ligament injury is suspected, further ligamentous testing should be performed. The medial and LCL can be examined by applying valgus and varus stresses respectively at 30° of knee flexion . Repeating these tests at 0° of flexion will also assess the capsular and cruciate components to valgus and varus stability. Repeating the posterior drawer test with the tibia placed in internal rotation will assess the medial structures. If the posterior drawer decreases with internal tibial rotation, the medial structures are most likely intact. In combined ligament injuries (PCL /MCL or PCL/ACL/MCL), the usual tightening observed when the posterior drawer is performed with the patient’s tibia in internal rotation is lost.
Diagnostic Imaging
Plain Radiographs
A routine series of radiographs include a 45° flexed weightbearing posteroanterior [16], lateral, and Merchant’s view [17] radiographs, and these images should be obtained for all patients with acute knee injuries. The radiographs, however, are not diagnostic for a PCL injury . Occasionally, an avulsion fracture of the tibial PCL insertion may be seen, but these are fairly uncommon [18]. A modified axial view has been described that allows for measuring of the amount of posterior tibial translation, which is compared to the uninjured side [19].
Magnetic Resonance Imaging
In the acute setting, magnetic resonance imaging (MRI ) of the PCL -injured knee has been reported to be 99–100 % sensitive and specific [20, 21]. We do not recommend routine MRI examinations for patients with PCL tears because the severity of damage to the PCL as seen on the MRI does not correlate with function or laxity. In my opinion, MRI diagnosis of PCL injuries with knee dislocations has led to unnecessary surgical treatment of the PCL. This overtreatment stems from a lack of knowledge that the PCL can heal [22, 23], even when a “complete tear” is diagnosed from the MRI scan [22].
Tewes et al. [23] obtained follow-up MRI scans at an average of 20 months after injury for 13 patients with high-grade PCL tears. The results showed that the PCLs of 10 of 13 patients (77 %) had regained continuity, although with an abnormal appearance. Clinical or functional status did not correlate with the degree of posterior laxity.
In a similar study, Shelbourne et al. [22] obtained MRI scans acutely after injury and then again at a mean of 3.2 years after injury on 27 patients with isolated acute PCL tears and 17 patients with acute PCL injuries in combination with other ligamentous injuries. The investigators assessed the healing potential of partial and complete tears as graded on the MRI scans. The results showed that all partial and most complete (19 of 22) PCL tears regained continuity on MRI scans and that location, severity, and associated ligament injury were not factors. The healed PCL did demonstrate abnormal morphology in 25 of the 37 continuous PCLs at follow-up.
Ahn et al. [24] evaluated PCL laxity in 49 patients who were treated with casting and bracing after acute PCL injury to determine if there would be a change in laxity with treatment. The grade of laxity at initial evaluation was grade 1 in 13 patients and grade 2 in 25 patients. At a mean of 24 months after injury, the grades of PCL instability improved grade 0 in 3 patients, grade 1 in 21 patients, and grade 2 in 14 patients.
The time to obtain PCL healing after acute injury is as yet unknown. However, Shelbourne et al. [25] described the development of a firm endpoint and painless posterior drawer at follow-up examination of acute PCL injured knees at about 2 weeks after injury.
Given the findings of these studies showing a “normal” PCL in the chronic setting, MRI evaluation of the PCL for patients who suffer chronic instability may not be helpful (Fig. 7.5). Therefore, treatment decisions should not be based on MRIs, but on clinical examination.
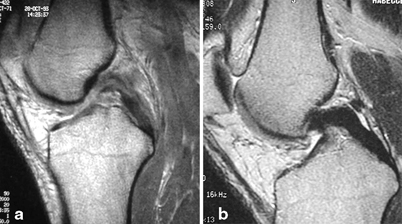
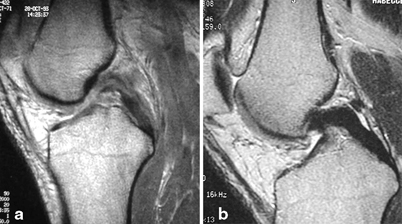
Fig. 7.5
The MRI scan (a) of an acute PCL injury determined to be a complete PCL tear. A follow-up scan (b) at 8 months after injury shows the PCL to be in continuity. PCL posterior cruciate ligament, MRI magnetic resonance imaging
With PCL laxity, the MRI scan will often show the posterior medial meniscus to be behind the femur and out of contact with the femoral condyle. If this is seen on a scan with the PCL in continuity, it may serve as an adjunctive sign of a previous PCL tear that has healed with PCL laxity (Fig. 7.6).


Fig. 7.6
MRI scanning in PCL lax knees often shows the posterior medical meniscus (white arrow) to be behind the femur and out of contact with the femoral condyle. PCL posterior cruciate ligament, MRI magnetic resonance imaging
Natural History Studies
Most published studies of PCL injuries treated nonoperatively were conducted retrospectively and included patients who sought treatment because of chronic PCL laxity and painful symptoms or include patients with multiple knee ligament injuries [1–4]. These studies do not give a true picture of the natural history of isolated PCL injuries and may represent a worse outcome than what would be found from evaluating a population of patients prospectively after acute isolated PCL injury .
Only a few PCL studies report long-term subjective or objective results for isolated, PCL injuries in patients followed prospectively after an acute injury [25–27].
Patel et al. [26] evaluated 57 patients (58 knees) who were seen acutely for isolated PCL injuries and were treated nonoperatively with rehabilitation to restore the knee ROM and strength. Patients were evaluated again at a mean of 6.9 years after the injury and they were not being seen because they were having troubling symptoms. No correlation was found between subjective scores and length of follow-up or between subjective scores and grade of PCL laxity. The mean Lysholm score was 85.2 ± 10 points. Radiograph showed medial compartment degenerative changes in ten knees (seven mild grade 1; three knees moderate grade 2) and four knees had mild grade 1 patellofemoral changes.
In a subjective follow-up study of 215 patients at a mean of 7.8 years after acute, isolated PCL injury , a similar lack of correlation was found between subjective scores and grade of PCL laxity [27]. The subjective results were lower than scores of normative data of patients with no history of injury to the knee, but the scores did not decrease significantly with time.
Shelbourne et al. [25] reported the natural history of 133 patients after acute, isolated PCL injury . Sixty-eight of the patients returned for objective follow-up at a mean of 5.4 years after the injury and the other 65 returned subjective surveys. There was no statistically significant difference in subjective survey scores between patients who returned for both objective and subjective follow-up and patients who were able to return surveys only. No change in laxity was found from initial exam to final follow-up, and patients with greater laxity did not have worse subjective or objective scores. No correlation was found between radiographic joint space narrowing and grade of laxity. Ten of 67 patients (1 patient refused radiographs) had evidence of arthrosis in the injured knee alone, and 15 patients had arthrosis in the both the injured and noninjured knees. Regardless of PCL laxity, one half of the patients returned to the same sport at the same level, one third of the patients returned to the same sport at a lower level, and one sixth of patients were not able to return to the same sport.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








