For many nutrition deficiencies, a direct cause and effect of different symptoms and diseases has been established. These are known as primary nutritional deficiencies. Secondary deficiencies occur when the vitamin or nutrient requirement may be increased, such as in patients who have pernicious anemia who lack the intrinsic factor needed to absorb vitamin B12. Less well recognized are the effects of nutritional deficiencies on chronic disease, especially acute and chronic neuromuscular diseases. This article identifies some of the causative factors and provides the reader with a guideline for what to consider in the evaluation of individuals who have neuromuscular problems. The context of these disorders is best understood on a foundation of basic nutrition information.
Much is known about the effects of malnutrition on health in general. The British navy discovered that carrying limes on board would prevent the ravages of scurvy, a dreaded disease later found to be the result of vitamin C deficiency. For many nutrition deficiencies, a direct cause and effect of different symptoms and diseases has been established. These are known as primary nutritional deficiencies. Secondary deficiencies occur when the vitamin or nutrient requirement may be increased, such as in patients who have pernicious anemia who lack the intrinsic factor needed to absorb vitamin B12. Less well recognized are the effects of nutritional deficiencies on chronic disease, especially acute and chronic neuromuscular diseases. This article identifies some of the causative factors and provides the reader with a guideline for what to consider in the evaluation of individuals who have neuromuscular problems. The context of these disorders is best understood on a foundation of basic nutrition information.
Nutrition management principles
Food contains nutrients to support health and life. Good nutrition management ensures that individuals obtain all the substances in their diet to optimize health and provide a degree of satisfaction, because eating is one of the more powerful social activities. Almost every special occasion and most shared meals involve interaction with others. The subject of nutrition thus is intimately linked to one’s psychologic sense of well being .
Individuals are well nourished, malnourished, or have overt nutritional deficiencies. Malnutrition has been defined as the lack of one or more nutrients in the diet. An abundance of food, increased longevity, and financial resources to purchase different foods, however, has resulted in excessive and unbalanced nutrient intake.
Three conditions can result in suboptimal function secondary to malnutrition: (1) nutrition deficiency (undernutrition)—the result of insufficient intake of one or more nutrients to meet one’s nutritional requirements for cellular health and optimal metabolism; (2) nutrient excess (overnutrition)—the result of excessive intake of one or more nutrients; and (3) nutrient imbalance—the result of consuming inadequate amounts of some nutrients and excessive amounts of others.
Malnutrition is a continuum in which body stores of nutrients are altered such that there is an imbalance, with some nutrients being depleted and others being excessive. If the imbalance persists, alterations of metabolism at the biochemical level and overt disease may result .
Nutrients
These are chemical substances that must be consumed to sustain life. They must also be consumed in the right proportions and in combination with other nutrients that enhance their absorption. The six general categories of these nutrients are water, proteins, carbohydrates, fats, vitamins, and minerals.
Water is the most basic compound essential for life, comprising more than 50% of the body mass. It is an integral part of cell structures and the basic medium for all body fluids. Proteins, carbohydrates, and fats all supply energy and have different functions in body composition, cell structure, and metabolic activity. The basic components of protein, amino acids, and of fats, essential fatty acids, cannot be synthesized in the body and need to be ingested from foods containing them. Optimal ratios of these three nutrients are essential for health and can be obtained from a balanced diet. Excessive consumption of one, such as protein, in the absence of adequate caloric intake from the other three nutrients can be harmful, because the liver needs to chemically remove the nitrogen to use it for energy. If the body’s ability to excrete the nitrogen is exceeded, then ammonia may build up in the body. Excessive protein, fat, or carbohydrate is also converted to fat, leading to obesity, and skeletal muscle may be broken down to meet energy requirements if the caloric intake is inadequate .
Much is known about the deleterious effects of a diet inadequate in protein. Many individuals in the United States eat more than the recommended daily allowance for protein, yet certain population groups, such as those who have alcoholism, anorexia, illness of chronic disease, and the frail elderly who may already be malnourished, are at risk for developing protein calorie malnutrition. Epidemiologic studies have found a direct relationship between the risk for developing multiple sclerosis (MS) and dietary fat intake, especially animal fat . One study found a correlation between a high intake of complex carbohydrates and MS .
Vitamins are either water- or fat-soluble, and many are cofactors for enzymatic reactions in metabolism. Fat-soluble and some water-soluble vitamins are stored in the body to varying extents, so they may not need to be ingested daily, but become depleted over time if the intake is less than adequate. Minerals are inorganic elements and include trace elements that are essential for health ( Table 1 ).
| Nutrient | Major functions |
|---|---|
| Water-soluble vitamins | |
| Thiamin (vitamin B1) | Coenzyme in carbohydrate metabolism; nerve function |
| Riboflavin (vitamin B2) | Coenzyme in citric acid cycle, fat metabolism, and electron transport chain |
| Niacin (vitamin B3) | Coenzyme in citric acid cycle, fat metabolism, and electron transport chain |
| Biotin | Coenzyme in glucose production and fat synthesis |
| Pyridoxine | Coenzyme in protein metabolism, neurotransmitter, and hemoglobin synthesis |
| Pantothenic acid | Coenzyme in citric acid cycle and fat metabolism (synthesis and beta-oxidation) |
| Folate | Coenzyme in RNA and DNA synthesis |
| Vitamin B12 | Coenzyme in folate metabolism, nerve function |
| Vitamin C | Collagen synthesis; hormone and neurotransmitter synthesis; antioxidant |
| Fat-soluble vitamins | |
| Vitamin A (retinoids and provitamin A carotenoids) | Vision; growth; cell differentiation; immunity; antioxidant |
| Vitamin D | Absorption of calcium and phosphorous; bone maintenance |
| Vitamin E | Antioxidant |
| Vitamin K | Blood clotting |
| Major minerals (<100 mg/day) | |
| Calcium | Bone and tooth structure; blood clotting; muscle contractions; nerve transmission |
| Phosphorous | Bone and tooth structure; intermediary metabolism; membrane structure; ATP |
| Sodium | Major extracellular cation; nerve transmission; regulates fluid balance |
| Potassium | Major intercellular cation; nerve–nerve transmission |
| Magnesium | Bone structure; enzyme function; nerve and muscle function; ATP |
| Chloride | Major extracellular anion; nerve transmission |
| Sulfur | Part of vitamins and amino acids; acid–base balance |
| Minor minerals (<20 mg/day) | |
| Iron | Part of hemoglobin and myoglobin; immunity |
| Cobalt | Part of vitamin B12 |
| Manganese | Functions in carbohydrate and fat metabolism; superoxide dismutase |
| Molybdenum | Cofactor for several enzymes |
| Fluoride | Strengthens tooth enamel |
| Copper | Iron metabolism; superoxide dismutase; nerve and immune function; lipid metabolism; collagen |
| Zinc | Cofactor in hundreds of enzyme systems; protein synthesis; growth; immunity; superoxide dismutase; alcohol metabolism |
| Iodine | Synthesis of thyroid hormone |
| Selenium | Antioxidant function as component of glutathione peroxidase |
| Chromium | Glucose tolerance |
Nutrients
These are chemical substances that must be consumed to sustain life. They must also be consumed in the right proportions and in combination with other nutrients that enhance their absorption. The six general categories of these nutrients are water, proteins, carbohydrates, fats, vitamins, and minerals.
Water is the most basic compound essential for life, comprising more than 50% of the body mass. It is an integral part of cell structures and the basic medium for all body fluids. Proteins, carbohydrates, and fats all supply energy and have different functions in body composition, cell structure, and metabolic activity. The basic components of protein, amino acids, and of fats, essential fatty acids, cannot be synthesized in the body and need to be ingested from foods containing them. Optimal ratios of these three nutrients are essential for health and can be obtained from a balanced diet. Excessive consumption of one, such as protein, in the absence of adequate caloric intake from the other three nutrients can be harmful, because the liver needs to chemically remove the nitrogen to use it for energy. If the body’s ability to excrete the nitrogen is exceeded, then ammonia may build up in the body. Excessive protein, fat, or carbohydrate is also converted to fat, leading to obesity, and skeletal muscle may be broken down to meet energy requirements if the caloric intake is inadequate .
Much is known about the deleterious effects of a diet inadequate in protein. Many individuals in the United States eat more than the recommended daily allowance for protein, yet certain population groups, such as those who have alcoholism, anorexia, illness of chronic disease, and the frail elderly who may already be malnourished, are at risk for developing protein calorie malnutrition. Epidemiologic studies have found a direct relationship between the risk for developing multiple sclerosis (MS) and dietary fat intake, especially animal fat . One study found a correlation between a high intake of complex carbohydrates and MS .
Vitamins are either water- or fat-soluble, and many are cofactors for enzymatic reactions in metabolism. Fat-soluble and some water-soluble vitamins are stored in the body to varying extents, so they may not need to be ingested daily, but become depleted over time if the intake is less than adequate. Minerals are inorganic elements and include trace elements that are essential for health ( Table 1 ).
| Nutrient | Major functions |
|---|---|
| Water-soluble vitamins | |
| Thiamin (vitamin B1) | Coenzyme in carbohydrate metabolism; nerve function |
| Riboflavin (vitamin B2) | Coenzyme in citric acid cycle, fat metabolism, and electron transport chain |
| Niacin (vitamin B3) | Coenzyme in citric acid cycle, fat metabolism, and electron transport chain |
| Biotin | Coenzyme in glucose production and fat synthesis |
| Pyridoxine | Coenzyme in protein metabolism, neurotransmitter, and hemoglobin synthesis |
| Pantothenic acid | Coenzyme in citric acid cycle and fat metabolism (synthesis and beta-oxidation) |
| Folate | Coenzyme in RNA and DNA synthesis |
| Vitamin B12 | Coenzyme in folate metabolism, nerve function |
| Vitamin C | Collagen synthesis; hormone and neurotransmitter synthesis; antioxidant |
| Fat-soluble vitamins | |
| Vitamin A (retinoids and provitamin A carotenoids) | Vision; growth; cell differentiation; immunity; antioxidant |
| Vitamin D | Absorption of calcium and phosphorous; bone maintenance |
| Vitamin E | Antioxidant |
| Vitamin K | Blood clotting |
| Major minerals (<100 mg/day) | |
| Calcium | Bone and tooth structure; blood clotting; muscle contractions; nerve transmission |
| Phosphorous | Bone and tooth structure; intermediary metabolism; membrane structure; ATP |
| Sodium | Major extracellular cation; nerve transmission; regulates fluid balance |
| Potassium | Major intercellular cation; nerve–nerve transmission |
| Magnesium | Bone structure; enzyme function; nerve and muscle function; ATP |
| Chloride | Major extracellular anion; nerve transmission |
| Sulfur | Part of vitamins and amino acids; acid–base balance |
| Minor minerals (<20 mg/day) | |
| Iron | Part of hemoglobin and myoglobin; immunity |
| Cobalt | Part of vitamin B12 |
| Manganese | Functions in carbohydrate and fat metabolism; superoxide dismutase |
| Molybdenum | Cofactor for several enzymes |
| Fluoride | Strengthens tooth enamel |
| Copper | Iron metabolism; superoxide dismutase; nerve and immune function; lipid metabolism; collagen |
| Zinc | Cofactor in hundreds of enzyme systems; protein synthesis; growth; immunity; superoxide dismutase; alcohol metabolism |
| Iodine | Synthesis of thyroid hormone |
| Selenium | Antioxidant function as component of glutathione peroxidase |
| Chromium | Glucose tolerance |
Assessing nutritional status
Nutritional assessment means the gathering and interpretation of data from which the effect of disease, injury, other stressors, and nutritional intervention can be monitored over time. Nutritional screening identifies those patients who require more comprehensive nutritional assessment to determine the risk for malnutrition. The latter requires direct measurement of food intake for nutrients and calories, along with measures of clinical anthropometric, biochemical, and physiologic status. The extent of the assessment may vary depending on the person’s problems and the nutritional goals. Known physical examination findings may alert the health care provider to the presence of specific nutritional deficiencies ( Table 2 ).
| Clinical findings | Possible nutritional causes |
|---|---|
| Hair | |
| Dyspigmentation (flat sign) | Protein deficiency |
| Easily plucked | Protein deficiency |
| Sparse | Protein, biotin, zinc deficiency |
| Corkscrew hairs | Vitamin C deficiency |
| Nails | |
| Spoon nails (koilonychia) | Iron deficiency |
| Brittle nails | Iron deficiency, excess vitamin A |
| Transverse ridging | Protein deficiency |
| Skin | |
| Scaling | Vitamin A, essential fatty acid, zinc deficiency |
| Follicular hyperkeratosis | Vitamin A deficiency |
| Purpura | Vitamin C, K deficiency |
| Yellow coloration | Excess carotene |
| Pellagrous dermatitis | Niacin deficiency |
| Cellophane appearance | Protein deficiency |
| Eyes | |
| Night blindness | Vitamin A deficiency |
| Bitot spots | Vitamin A deficiency |
| Papilledema | Vitamin A excess |
| Pale conjunctivae | Iron deficiency |
| Mouth | |
| Angular stomatitis | Riboflavin, niacin, pyridoxine deficiency |
| Cheilosis | Riboflavin, niacin, pyridoxine deficiency |
| Tongue | |
| Pale, atrophic | Iron deficiency |
| Atrophic lingual papillae | Riboflavin, niacin, folate, vitamin B12, protein, iron deficiency |
| Glossitis (scarlet) | Riboflavin, niacin, folate, vitamin B12, pyridoxine deficiency |
| Hypogeusia | Zinc deficiency |
| Gums | |
| Spongy, bleeding | Vitamin C deficiency |
| Musculoskeletal | |
| Beading of ribs | Vitamin D deficiency |
| Muscle wasting | Protein-calorie malnutrition |
| Tenderness | Vitamin C deficiency |
| Neurologic | |
| Confusion | Thiamin, niacin, vitamin B12 deficiency |
| Ophthalmoplegia | Thiamin, phosphorous deficiency |
| Peripheral neuropathy | Thiamin, pyridoxine, vitamin B12 deficiency |
| Tetany | Calcium deficiency |
| Other | |
| Cardiomegaly | Thiamine deficiency |
| Cardiomyopathy | Selenium deficiency |
| Hepatomegaly | Protein malnutrition |
| Edema | Protein, thiamin deficiency |
| Thyroid enlargement | Iodide deficiency |
Identifying nutritional risk
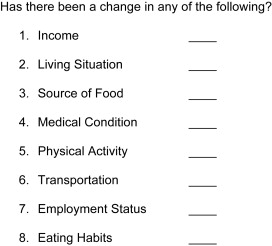
Nutritional risk that leads to malnutrition and hence neuromuscular complications involves many factors ( Fig. 1 ). Certain population groups have higher risk. Young children have special nutrient requirements for growth, whereas the elderly have slower metabolism and decreased activity that lead them to require fewer calories but that doesn’t decrease their need for specific nutrients. Those who are chronically ill have specific nutrition needs, and they may be on prolonged inadequate parenteral nutrition. Individuals who have eating disorders, anorexia and obesity, alcoholic patients who consume primarily alcohol, poor and homeless individuals who lack resources to purchase food, and those who have dysphagia, prolonged depression, or cognitive impairments may be at risk for inadequate intake of key nutrients. The elderly may have a unique combination of risk factors, including financial, social, multiple organ failure, decreased muscle mass, swallowing problems, and dementia, all of which may affect their ability to take in adequate nutrients and calories. As caloric intake decreases, it may be difficult to obtain essential nutrients. Still others who have malabsorption caused by diseases such as celiac sprue, Crohn disease, inflammatory bowel disease, or pernicious anemia are at risk. It is essential to consider multiple factors, including social, environmental, medical, and economic, which put the individual host at risk. When seeing an individual at follow-up, key questions include whether there has been any change in medical condition, cognition, mental health, physical activity, and ability to obtain or prepare food because of changes in income, employment status, transportation, or living situation. All of these factors determine one’s overall eating habits and nutritional status ( Fig. 2 ).

Neuromuscular disorders
For optimal functioning of the nervous system, one needs to have adequate intake of the water-soluble B-group vitamins—in particular, thiamine, niacin, pyridoxine, and vitamin B12, fat-soluble vitamins D and E, folic acid, copper, and zinc. Peripheral nerve problems and less frequently myopathy can occur because of deficiencies of one or more of these essential nutrients .
Thiamine deficiency
Thiamine deficiency is named “beriberi,” the first identified human nutritional deficiency. Thiamine serves as a coenzyme in the metabolism of carbohydrates and branch chain amino acids. When there is inadequate thiamine, there is a decreased synthesis of high-energy phosphates, and lactate accumulates. There is a decreased level of alpha KGDH, a rate-limiting enzyme in the tricarboxylic acid cycle, that results in the decreased synthesis of amino acid neurotransmitters . Vitamin B1 might have a role in nerve function involving acetylcholine receptor clustering and acetylcholine biosynthesis .
Main food sources for vitamin B1 include meat (pork), cereals and grain products, legumes, and fruits . Vitamin B1 is reabsorbed predominantly in the duodenum and jejunum through a carrier-mediated transport (at lower intakes) and passive diffusion (at higher intakes) . This vitamin cannot be synthesized ; the half-life is 10 to 14 days, and the body stores are 30 to 100 mg. A deficiency thus could occur in as little as 6 to 8 weeks. One needs a continuous dietary supply, 1 to 1.5 mg per day. Alcoholic individuals who consume primarily hard liquor (beer has B vitamins) are prone to thiamine deficiency. Because of inadequate intake, liver stores are rapidly deleted and gastrointestinal absorption is impaired, because alcohol inhibits the transport of thiamine in the gastrointestinal tract and blocks the phosphorylation of thiamine to thiamine pyrophosphate (TPP). Individuals who have higher metabolic rates and those who are malnourished or who are on high-carbohydrate, low-protein diets with the main staple being milled rice have higher requirements. This includes high-risk patients participating in vigorous exercise with high-carbohydrate intake or those who are receiving IV glucose. Administration of IV glucose to a vitamin-depleted alcoholic patient or one at risk may precipitate a florid syndrome if supplementary vitamins are not provided .
The most vulnerable to a deficiency are the tissues with the highest turnover, caudal brain and cerebellum. Different types of deficiency are dry, wet, and infantile beriberi, with the dry form causing sensorimotor distal, axonal, peripheral neuropathy as noted by electrodiagnosis and sural nerve biopsy, leg cramps, muscle tenderness, and burning feet . On clinical examination, one may find ankle and toe weakness with foot drop, decreased ankle jerks, and decreased fine motor and vibratory sense, with more generalized stocking/glove hypoesthesia, hypalgesia, and severe weakness later. Severe cases may also affect the phrenic and vagal nerves, and there may be associated autonomic neuropathy and tongue and facial weakness . The neurologic changes often do not resolve completely with treatment.
Wet beriberi may cause pedal edema, high-output congestive heart failure, cardiac failure with lactic acidosis, and sensorimotor peripheral neuropathy, and it can become dry after diuresis. These symptoms respond dramatically to parenteral administration of thiamine. The infantile form, or Shoshin beriberi, bears little resemblance to the adult type and involves cardiac problems, aphonia, and a pseudomeningismus .
The most common central nervous system (CNS)-related neurologic problem in the alcoholic individual is Wernicke-Korsakoff syndrome. Wernicke encephalopathy (WE) is characterized by gait ataxia secondary to cerebellar dysfunction or polyneuropathy, confusion, and ocular palsies (with nystagmus lateral and conjugate gaze) . There may be hypothermia, orthostatic hypotension, skin changes, truncal ataxia, features of liver disease, tongue redness, and an associated peripheral neuropathy in 80% of individuals. MRI reveals T2 enhancement around the third or fourth ventricle, periaqueductal midbrain, dorsal medial, thalami, and mammillary bodies and hemorrhagic brainstem lesions that can cause sudden death . Pathologic studies of the brains in fatal cases demonstrate necrotic or hemorrhagic lesions in many areas of the brainstem and brainstem nuclei. Wernicke encephalopathy may occur within 4 to 12 weeks after bariatric surgery as mentioned elsewhere in this issue, with most patients having the clinical triad mentioned . Treatment with parenteral thiamine results in significant recovery, with the abnormal findings on MRI disappearing.
Korsakoff psychosis occurs after the ocular manifestations and encephalopathy subside and involves similar areas of the brain as Wernicke. The psychosis is characterized by anterograde amnesia, retrograde amnesia to a lesser extent, a disordered time sense, and confabulation in the later stages .
The erythrocyte transketolase activation is the preferred laboratory study to confirm a deficiency, because urine and serum do not reflect tissue stores well . Treatment of thiamine deficiency is possible but may be precarious in at-risk patients.
They should receive parenteral thiamine before IV glucose or parenteral nutrition, because the IV glucose may consume what is there and may precipitate Wernicke encephalopathy.
To treat beriberi the patient needs 100 mg IV thiamine, then 100 mg intramuscular thiamine daily for 5 days, with a permanent oral maintenance dose of 50 to 100 mg . The wet type improves rapidly, with clearing of symptoms within 24 hours to 1 week and improvement in sensory or motor symptoms within weeks to months .
With alcoholism-related neuropathy, the lipophilic form of thiamine should be used, 320 mg daily for 4 weeks, then 120 mg daily for another 3 weeks .
Response to WE treatment is variable for improvement in gait ataxia/memory, but the apathy and lethargy may improve over months .
Even with thiamine treatment, there may be 10% to 20% mortality. Some patients who have Korsakoff syndrome have impaired memory and learning long term.
A proximal myopathy with muscle weakness and myalgias may also be associated with a thiamine deficiency , because it decreases the production of ATP needed for muscle contraction. With less ATP, the muscle sustains some injury, as reflected in elevated creatine kinase levels. With appropriate thiamine supplementation, the muscle strength improves in 1 week, especially proximally, with the myalgia subsiding in 2 months and the creatine kinase level normal in 3 months.
Niacin deficiency
Niacin is the end product of tryptophan metabolism and is converted into nicotinamide adenine dinucleotide and nicotinamide adenine dinucleotide phosphate, coenzymes important in carbohydrate metabolism.
Pellagra, the classic niacin deficiency, is rare in developed countries, except if corn is the dietary staple, because corn lacks niacin and tryptophan. Foods rich in niacin include meat, fish, poultry, enriched grains and breads, and fortified cereals. The RDA (Recommended Daily Allowance) is 16 mg daily for men and 14 mg daily for women of niacin equivalent, with 1 mg niacin equivalent equal to 51 mg niacin or 60 mg tryptophan. It is not common in individuals who have alcoholism and malabsorption, because it is absorbed by simple diffusion with 30% of niacin protein bound . A deficiency occurs in carcinoid syndrome, because tryptophan is converted to serotonin, not niacin. Biotransformation of tryptophan to nicotinic acid requires vitamins B2 and B6, iron, and copper, so one can also see secondary vitamin B6 deficiency. Pellagra affects the gastrointestinal tract, skin, and nervous system .
Patients have dermatitis, diarrhea, and dementia. The reddish-brown keratotic rash affects the face, chest, dorsum of the hands, and feet. There is anorexia, abdominal pain, diarrhea, and stomatitis. Neurologic problems are diffuse and complicated by other vitamin deficiencies. In fact, neuropathies may worsen if patients receive niacin supplementation without the rest of the vitamin B complex . The peripheral neuropathy is indistinguishable from other causes, such as thiamine deficiency. There may be confusion with coma, spasticity, and myoclonus and progressive encephalopathy in alcoholic patients .
Laboratory studies include the urinary excretion of methylated metabolites, N-methylnicotinamide and its 2-pyridone derivative (N-methyl-2-pyridone-5-carboxamide) . Treatment consists of oral nicotinic acid, 50 mg three times daily, or parenteral doses, 25 mg three times daily. Advanced pellagra is treated with intramuscular nicotinic acid, 50 to 100 mg three times daily for 3 to 4 days followed by oral supplementation . In Parkinsonism, treatment with L-dopa, especially when given with a decarboxylase inhibitor (carbidopa) increases the risk for niacin deficiency. Supplementation with niacin may increase the efficacy of L-dopa by extending the length of time that L-dopa levels remain elevated in the brain . Also, nicotinamide adenine dinucleotide (NADH), a coenzyme formed from niacin, is required for the synthesis of tetrahydrobiopterin, the cofactor for the enzyme (tyrosine hydroxylase) that catalyzes the conversion of tyrosine to L-dopa .
Riboflavin
The rare Strachan syndrome is partially related to a deficiency of this vitamin and causes orogenital dermatitis, painful sensory neuropathy, amblyopia, and deafness. It is found in severely malnourished populations and is believed to result from distal degeneration of central and peripheral processes of sensory neurons. Riboflavin supplementation seems to reverse the skin manifestations .
Vitamin B6
Vitamin B6 has three main active derivatives: pyridoxal, pyridoxine, and pyridoxamine . Its cellular functions as a coenzyme in the form of pyridoxal phosphate (PLP) are important in metabolic reactions, involving amino acids, lipids, nucleic acid, and one carbon units, for gluconeogenesis, neurotransmitter, and hemoglobin biosynthesis . The interconversion and metabolism depends on riboflavin, niacin, and zinc.
Niacin, carnitine, and folate also require vitamin B6 for their metabolism. Food sources are meat, fish, eggs, soybeans, nuts, and dairy products. It cannot be synthesized from exogenous sources and is absorbed by way of the intestine . All forms are phosphorylated for metabolic trapping.
The RDA is 1.3 mg daily for men and 1.4 mg daily for women, with the upper limit (UL) being 100 mg daily. Administration of 2 mg of vitamin B6 daily after bariatric surgery has been shown to prevent deficiency . Excess consumption in the range of 1 to 5 grams daily for 2 to 3 years can cause a pure sensory peripheral neuropathy , sensory ataxia, areflexia, impaired cutaneous and deep sensation, and a positive Romberg sign. These findings may reverse once excessive supplementation is withdrawn. A deficiency causes a microcytic hypochromic anemia, and treatment of 50 to 100 mg daily may prevent the development of neuropathy. Infants who have deficiencies may have seizures, but adults are more resistant.
Pregnant and lactating women, those taking estrogen, and the elderly are most at risk for a pyridoxine deficiency, which is more frequent with administration of vitamin B6 antagonists, isoniazid (INH), cycloserine, hydralazine, and penicillamine . With INH one can get an associated neuropathy, including limb weakness and sensory ataxia . It is dose related and associated with axonal degeneration and regeneration, affecting myelinated and unmyelinated fibers on sural biopsy ; it is reversible by discontinuing the drug or by supplementing the patient with vitamin B6 .
Treatment for Parkinsonism with L-dopa and a decarboxylase inhibitor may provoke a marginal vitamin B6 deficiency , which is important in Parkinson disease, because dopa decarboxylase catalyzes the conversion of dopa to dopamine and depends on pyridoxal phosphate, the activated form of vitamin B6. Some clinical trials of vitamin B6 supplementation to patients who have Parkinsonism suggest that tremor, muscle cramps, rigidity, bladder control, gait, and energy are improved, although further studies are needed to substantiate .
Vitamin B12
Cyanocobalamin (Cbl) is the chemical name for vitamin B12. The active forms are methyl Cbl and adenosyl Cbl . Food sources are meat, eggs, and milk, and there are no adverse effects associated with excess Cbl intake. Vitamin B12 is essential in DNA synthesis, being a cofactor for folate-dependent methionine synthase, and mitochondrial-β-oxidation of fatty acids being a cofactor for methylmalonyl CoA mutase . Stomach acid and pepsin dissociate Cbl from proteins and it binds with R protein secreted by the gastric of the small intestine, which is degraded in the neutral pH of the small intestine, and hydrolyzed by pancreatic enzymes to release the Cbl, which then binds with intrinsic factor (IF), secreted by gastric parietal cells. In the terminal ileum, the vitamin B12–IF complex finds an IF receptor and is absorbed by the intestinal mucosal cells. A deficiency of Cbl may cause pernicious anemia (PA), and one may also have an associated iron deficiency .
Neurologic manifestations of Cbl deficiency are caused by overproduction of myelinolytic tumor necrosis factor (TNF) alpha and reduced synthesis of epidermal growth factor and interleukin 6. Deficiencies are seen with metabolic problems and in the elderly. Those who develop MS before age 18 years also have lower serum vitamin B12 levels, suggesting that the deficiency may lead to vulnerability in the viral or immune mechanisms believed to cause MS, although MS may increase the need for vitamin B12 .
Causes of vitamin B12 deficiency are atrophic gastritis, achlorhydria-induced food Cbl malabsorption, acid reduction therapy with H2-blockers, ileal disease, resection with malabsorption, and, rarely, decreased dietary intake. Often the etiology is not known . The neuropathy associated with vitamin B12 deficiency may be related to interference with methylation reactions in the CNS . Myelopathy with and without neuropathy is seen with combined degeneration of the cervical and upper thoracic posterior columns . In the white matter there are foci of myelin and axon destruction. MRI reveals signal change in the subcortical white matter and posterior and lateral columns , and electrodiagnosis reveals axonal degeneration with and without demyelination. There is sensorimotor axonopathy, possible multifocal alterations in conduction, abnormal somatosensory-evoked potentials in central sensory pathways, visual-evoked potentials, and motor-evoked potentials .
Cognitive impairment, optic neuropathy causing cacco-central scotoma, paresthesias, and polyneuropathy can coexist. The clinical picture most often consists of paresthesia starting in the lower extremities and spreading up to the trunk, difficulty walking, gait disturbance, and in advanced cases, sphincter dysfunction. The physical signs characteristically show spastic and ataxic gait with signs of peripheral neuropathy, ie, absent ankle reflexes. In some cases, Lhermitte sign may be observed. Cognitive impairment is not uncommon in this condition, and severity varies from mild irritability and mood disturbance to frank dementia . Some patients may have high folate levels. The neurologic problems with low Cbl do not establish cause and effect of Cbl deficiency , which can also be seen with copper deficiency . Laboratory findings include macrocytic red blood cells, megaloblastic anemia, and low serum Cbl . Increased gastrin levels and markers for hypochlorhydria or achlorhydria are seen with pernicious anemia, and they have a high sensitivity and specificity for PA. These problems are also seen in 30% of elderly patients . Clinically the patient may have glossitis, weight loss, and loss of appetite, and some patients may have orthostatic hypotension . Diagnosis requires checking serum vitamin B12 level. A low level of vitamin B12 in serum in the setting of compatible clinical features, neuroimaging, and electrophysiologic studies establishes the diagnosis. In some cases of vitamin B12 deficiency, the vitamin B12 level could be within normal ranges. In such cases, serum methylmalonic acid and homocysteine, if elevated, help with the diagnosis . Treatment with 3 to 5 μg daily may suffice if absorption is normal. Malabsorption secondary to achlorhydria may require parenteral supplementation with 50 to 100 μg daily . Maintenance therapy is 1000 μg intramuscularly monthly . Response of the hematologic derangement should be prompt and complete within 6 months. Alcohol abuse affects the enterohepatic recycling of Cbl, affecting folate metabolism, and accelerates the breakdown of folate. The anemia of Cbl deficiency may respond to folate therapy, but the response is often incomplete .
Folic acid
Folate or folic acid consists of pterin linked to p-aminobenzoic acid. It acts through its coenzyme by modifying, accepting, or transferring one-carbon moieties in single carbon reaction in metabolism of nucleic and amino acids. Biochemical pathways requiring folic acid include interconversion of serine and glycine, methionine cycle, histidine catabolism, thymidylate, and purine cycles. Methyl-tetrahydrofolate (methyl-THF) is the predominant folate . Vitamin B12 acts as a coenzyme in the conversion of methyl-THF to THF, the biologically active form. Vitamin B12 deficiency can also cause folate deficiency with the megaloblastic anemia being indistinguishable from Cbl deficiency .
Foods rich in folate include spinach, yeast, peanuts, liver, beans, and beer, with the bioavailability being 50% from food and 100% from folic monoglutamate. Fortification of grains and cereals has been mandated since 1998 in the United States for the prevention of neural tube defects, but folates in food are labile and are lost with boiling. The RDA is 400 μg daily of dietary folate equivalent, with the UL being 1000 μg daily. Absorption is in the proximal small intestines; cellular folate uptake occurs by passive diffusion, and folate undergoes polyglutamation that permits attachment to enzymes. Daily losses are 1% to 2% of body stores, and the body stores to daily requirement ratio is 100:1. Serum folate decreases within 3 weeks of decreased intake . A deficiency can be seen within 3 months or faster in those who have low stores or alcoholism. Metabolism can be impaired by methotrexate or inborn errors of metabolism. Patients taking carbamazepine are susceptible to folate deficiency, because the drug impairs absorption . Deficiency of folate is rarely seen in isolation except for small bowel disorders affecting absorption. These include inflammatory bowel disease, tropical sprue, or Celiac disease.
Alcoholic patients may have a deficiency of folic acid, usually in combination with other vitamins.
Neurologic problems are less common than they are with other nutrient deficiencies. Myeloneuropathy or polyneuropathy, including retrobulbar optic neuropathy, can be seen in association with folate deficiency or can be associated with affective psychiatric disorders .
Treatment of folate deficiency is 1 mg folate three times daily, followed by 1 mg daily. Parenteral administration of 1 to 5 mg daily is appropriate for more ill patients. Women who have epilepsy should take 0.4 mg for prophylaxis against neural tube defects.
Vitamin D
Vitamin D has several active metabolites, with 25-hydroxyvitamin D levels less than 50 nmol/L in the serum being associated with increased body sway and decreased neuromuscular coordination, whereas a level less than 30 nmol/L is associated with decreased muscle strength. There is an osteomalacic myopathy that causes one to have difficulty getting up from a chair, an inability to ascend stairs, and diffuse muscle pain. It is difficult to quantitate this loss of strength, given its predilection for proximal muscles, although electrodiagnosis can confirm a myopathic pattern with decreased motor unit amplitude and duration and increased polyphasicity . A subclinical neuropathy can cause decreased nerve conduction velocities of the ulnar and peroneal nerves .
The skin can produce 80% to 90% of necessary vitamin D after exposure to UVB radiation, with hypovitaminosis D being more common in elderly individuals living in northern latitudes . The extent to which one’s body is covered with clothing or even sunscreen also affects the skin’s ability to synthesize vitamin D. Hypovitaminosis D-related myopathy has been diagnosed in immigrant teenagers who were veiled .
Vitamin D must undergo two hydroxylations in the liver and kidney to become the biologically active form, 1,25(OH) 2 D, with the conversion in the kidney regulated by parathyroid hormone. Other regulators include calcium, phosphate, growth hormone, and prolactin . A vitamin D binding protein (DBP) is a mediator of the effects of 25 OHD in muscle, and this active form, 25 OHD, may have more effect on striated skeletal muscle.
Calcium works together with vitamin D to maintain bone health in the human body . Vitamin D works through its active form, 1,25(OH) 2 D. The primary action of 1,25(OH) 2 D is to promote intestinal absorption of calcium and phosphorus through the small intestine. This reaction is regulated by parathyroid hormone. Moreover, calcium is important in nerve and muscle functions . Calcium is mainly absorbed in the duodenum and proximal jejunum, whereas vitamin D is absorbed mainly in the jejunum and ileum . In Roux-en-Y gastric bypass and biliopancreatic diversion, calcium and vitamin D deficiency predictably occur. Possible causes include bypassing the duodenum and proximal jejunum, food intolerance, and fat malabsorption. The frequencies of calcium and vitamin D deficiencies were reportedly 10% and 50%, respectively, after RYGB . The deficiency results in osteoporosis and osteomalacia. In one study, 800 IU of cholecalciferol in combination with 1200 mg of elemental calcium reduced hip fractures and other non-vertebral fractures after 18 months of treatment . There is a strong interdependency of the vitamin D deficiency with low levels of serum Ca and high levels of parathyroid hormone, so all three of these need to be evaluated. Increased secretion of parathyroid hormone, induced by vitamin D deficiency, contributes to bone fragility through loss of bone matrix and minerals, with decreased bone density at the hip and increased bone turnover .
Severe vitamin D deficiency in children causes rickets. At older ages, there is predominantly a myopathy (osteomalacia myopathy) affecting proximal strength, which may cause prominent muscle pain. A patient typically presents with progressive proximal weakness involving predominantly lower limbs, with gait difficulty, waddling gait, and difficulty rising from a chair or going up stairs. Physical examination reveals proximal weakness in the upper limbs and the muscles of the trunk . There is conflicting information about the findings on electrodiagnosis. Although the myopathy can be detected, other investigators have suggested slowing in the nerve conduction studies. Muscle biopsies have confirmed more atrophy of type II muscle fibers, which are fast and strong and recruited first to avoid falling. Because these fibers are preferentially affected in vitamin D deficiency, it may explain the high fall risk in vitamin D-deficient elderly patients .
Measurement of serum vitamin D, urine calcium, serum bone alkaline phosphatase (BAP), and serum parathyroid hormone (PTH) levels would help establish the diagnosis. In general, serum vitamin D and 24-hour urine calcium are decreased (total 25 OHD<15 ng/mL), and the levels of BAP and PTH are elevated . Treatment with vitamin D supplement results in definite improvement in strength and pain . If patients are deficient in vitamin D and calcium, the recommended supplements are 800 IU of cholecalciferol in combination with 1200 mg of elemental calcium . After bariatric surgery, the recommended vitamin D supplementation is 50,000 IU of vitamin D3 (cholecalciferol) or vitamin D2 (ergocalciferol) once per week . There is some evidence that vitamin D deficiency may be associated with an increased risk for type I diabetes, multiple sclerosis, rheumatoid arthritis, hypertension, cardiovascular heart disease, and cancers. Some suggest that yearly measurements of 25-hydroxyvitamin D should be part of the annual physical examination .
There is some evidence that the prevalence of MS is highest in regions where the vitamin D supplies are lowest and there is less environmental exposure to the sun, which limits vitamin D synthesis. Administration of one of the active metabolites of vitamin D, 1,25-OD 2 D, reduced disease activity in mice and rats with experimental allergic encephalomyelitis, suggesting some immune-mediated suppression of disease.
Supplementation with vitamin D for patients who have MS may therefore help to suppress the immunologic aspects of the disease and decrease bone resorption, fractures, and muscle weakness . An associated decrease in calcium can cause a change in solubilized proteins from mouse brain tissue to cause abnormalities similar to MS plaque .
Vitamin E
Alpha tocopherol is the active form of vitamin E, which typically includes supplements containing esters that prolong the shelf life, preventing oxidation . Foods containing vitamin E include vegetable oils, leafy vegetables, fruits, meat, nuts, and unprocessed cereal grains. Bioavailability depends on the food fat content and is better from enriched cereals than supplements . RDA is 15 mg daily, with the UL being 1000 mg daily.
Alpha tocopherol is an antioxidant and free radical scavenger that protects the cellular membrane from oxidative stress and inhibits the peroxidation of polyunsaturated fatty acids of membrane phospholipids. Absorption efficiency is less than 50% and requires bile acids, fatty acids, and monoglycerides for micelle formation. Biliary and pancreatic secretions are required for absorption. It takes 2 years for adipose tissue levels to reach steady state with dietary intake changes .
A deficiency is never caused by a dietary insufficiency, but rather is associated with Crohn disease, celiac disease, cystic fibrosis, blind loop syndrome, or small bowel resection. Another problem may result from inadequate intake with parenteral nutrition to maintain stores .
There is some suggestion that later development of Parkinson disease is associated with a low intake of vitamin E-rich food earlier in life . Neurologically, deficiency causes a spinocerebellar syndrome with variable peripheral nerve involvement . One may see ataxia, hyporeflexia, proprioceptive, or vibratory loss. Cutaneous sensations are affected less. There may be dysarthria, tremor, nystagmus, ophthalmoplegia, ptosis, pigmentary retinopathy, or myopathy, which is rare in humans .
Biopsies from the sural nerve reveal centrally-directed fibers of large myelinated neurons most involved .
Levels of vitamin E depend on serum lipids, cholesterol, and very low density, with hyperlipids increasing vitamin E. With a deficiency, serum vitamin E levels may not be detectable, but fat malabsorption with increased stool fat and decreased serum carotene levels may be present. Treatment when the deficiency is associated with malabsorption is 200 IU per kg daily of intramuscular di-x tocopherol (0.8–2.0 IU/kg/day) . With cholestatic liver disease, treatment with fat-soluble vitamin E is ineffective because of fat malabsorption. A water-soluble product helps increase levels of vitamin E in this case.
Copper
Copper deficiency in animal species does cause a myelopathy. Ruminants develop swayback. In humans, Menkes disease occurs, which is caused by a congenital deficiency . Myelopathy or myeloneuropathy may resemble a vitamin B12 deficiency . Copper and cyanocobalamin deficiencies may coexist, so if one still has neurologic problems after vitamin B12 supplementation, copper deficiency should be considered.
Copper functions as a prosthetic group in metalloenzymes, which act as oxidases that transfer electrons in mitochondria and help maintain the structure and function of the nervous system . It also plays an important role in iron metabolism, the neurotransmitter system (dopamine β-hydroxylase), and collagen synthesis (lysyl oxidase).
The RDA for copper is 900 μg daily, with the UL being 10,000 μg daily. Foods rich in copper are organ meats, seafood, nuts, seeds, wheat bran cereals, whole grain products, and cocoa products. Tea, potatoes, milk, and chicken do not contain much copper. Deficiency can be seen with prolonged parenteral nutrition use .
Absorption is by saturable active transport at lower levels of intake and passive diffusion at higher levels of intake in the stomach and throughout the small intestine. It is bound to albumin and transported by way of the portal vein to the liver for uptake there. Parenchymal cells then released into plasma are bound to ceruloplasmin 95% of the time. Urinary excretion is low, and excretion of copper into the gastrointestinal tract is the major pathway regulating copper homeostasis, preventing deficiency. Copper absorption can be inhibited by high zinc intake because of a zinc-induced high level of metallothionein. Metallothionein has a high affinity for copper, and the copper-bound metallothionein is sloughed off into the intestine, thus losing copper from the body. High zinc intake can precipitate copper deficiency in a predisposed patient . Copper absorption into intestinal mucosa requires copper transporters (Ctr1 copper transporter and DCT-1) . It is then transported to ATP7A to be exported from the intestinal cells into the circulation. Dietary factors affecting bioavailability are acid, amount of copper, molybdenum, or zinc intake, which, when excessive, reduces copper absorption and may possibly compete for common transport. Problems are usually related to impaired absorption, such as following bariatric surgery , with acquired deficiency being rare because of the ubiquitous distribution.
Neurologic manifestations include myelopathy with a spastic gait and sensory ataxia secondary to sensory loss from dorsal column involvement , similar to a vitamin B12 deficiency. There can be CNS demyelination and optic neuritis . Neurogenic bladder symptoms and Lhermitte signs may be observed. Brisk knee reflexes, extensor plantar response, and absent ankle reflexes are common physical signs. Electrodiagnosis reveals a peripheral neuropathy, sensorimotor axonal type; somatosensory-evoked potentials are consistent with a central delay; visual-evoked potentials are prolonged. Spinal MRI may have an increased signal on T2-weighted images in the paramedian cervical and thoracic cord . Hematologically there may be an anemia, neutropenia of unclear etiology, left shift granulocytosis with ringed sideroblasts but not sideroblastic anemia, or there may be no hematologic problems . In second generation rats, copper deficiency produces low dopamine levels in the corpus striatum and results in clinical signs similar to Parkinson disease , although in humans there is no evidence that copper supplementation is efficacious for the treatment of Parkinsonism. In animal studies, copper deficiency causes defective myelination . Serum copper is not totally adequate to assess copper stores . Ceruloplasmin is an acute phase reactant, and its increase parallels the increase in copper levels. It is seen during pregnancy, in liver disease, malignancy, hematologic disease, myocardial infarction, smoking, diabetes mellitus, uremia, and inflammatory and infectious diseases.
Treatment of low serum copper levels and low ceruloplasmin levels is copper supplementation orally, 2 mg daily. Response is fast, and one can reassess serum copper to determine the adequacy of replacement and reassess hematologic and sensory symptoms , with hematologic improvement being more dramatic than neurologic improvement. Neuroimaging studies may normalize after treatment . The frequency of copper deficiency after bariatric surgery is covered elsewhere in this issue.
Zinc
Zinc metabolism can be altered in diseases like Parkinsonism, in which there is oxidative stress . In guinea pigs that were zinc deficient, motor nerve conduction velocities were decreased and there was abnormal locomotion and posture . Catabolic states associated with inflammation or trauma may increase the use of zinc and may lead to a relative deficiency.
As mentioned, zinc can also induce copper deficiency, with treatment being discontinuing zinc, but hyperzincemia can accompany copper deficiency without exogenous zinc supplementation. Zinc levels therefore should also be checked in copper deficiency, as noted .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







