A wide variety of neuromuscular diseases affect children, including central nervous system disorders such as cerebral palsy and spinal cord injury; motor neuron disorders such as spinal muscular atrophy; peripheral nerve disorders such as Charcot-Marie-Tooth disease; neuromuscular junction disorders such as congenital myasthenia gravis; and muscle fiber disorders such as Duchenne’s muscular dystrophy. Although the origins and clinical syndromes vary significantly, outcomes related to musculoskeletal complications are often shared. The most frequently encountered musculoskeletal complications of neuromuscular disorders in children are scoliosis, bony rotational deformities, and hip dysplasia. Management is often challenging to those who work with children who have neuromuscular disorders.
A wide variety of neuromuscular diseases affect children, including central nervous system disorders such as cerebral palsy and spinal cord injury; motor neuron disorders such as spinal muscular atrophy; peripheral nerve disorders such as Charcot-Marie-Tooth disease; neuromuscular junction disorders such as congenital myasthenia gravis; and muscle fiber disorders such as Duchenne’s muscular dystrophy. Although the origins and clinical syndromes vary significantly, outcomes related to musculoskeletal complications are often shared. The most frequently encountered musculoskeletal complications of neuromuscular disorders in children are scoliosis, bony rotational deformities, and hip dysplasia. Management is often challenging to those who work with children who have neuromuscular disorders.
Scoliosis
Scoliosis refers to deviation from normal spinal alignment. A commonly accepted definition of scoliosis is a curvature in the coronal plane of greater than 10°. The coronal curvature is almost always associated with a sagittal alignment abnormality, such as kyphosis, lordosis, or a rotational component. Scoliosis may be classified as idiopathic, congenital, or neuromuscular in origin. Overall, idiopathic scoliosis accounts for the significant majority of cases of scoliosis in children and adolescents, whereas scoliosis associated with neuromuscular disease, congenital deformity, and other causes occurs less frequently in the total population. Neuromuscular scoliosis can occur as a complication of a wide variety of disease processes in children, including upper and lower motor neuron conditions and myopathies.
Scoliosis may lead to functional deficits, such as decreased sitting balance. The upper extremities may be required to maintain upright posture, thereby reducing the availability of the arms for functional daily tasks. Neck, shoulder, and spine range of motion may be limited. In Duchenne’s muscular dystrophy, for example, the rigid neck, hyperextension deformity with associated marked increase of cervical lordosis forces patients to bend their trunk forward and assume an awkward posture to look straight ahead . Scoliosis may result in skin breakdown or pain. As scoliosis becomes more severe, reduction in lung volumes and diaphragmatic heights may occur . Beyond 100°, pulmonary hypertension and right ventricular hypertrophy may develop .
Epidemiology
Idiopathic scoliosis occurs in 2% to 3% of the adolescent population . In contrast, the rates of spinal deformity in children who have neuromuscular disease are generally much higher and depend on the diagnosis ( Table 1 ). For example, 20% of patients who have mild cerebral palsy may develop scoliosis, but nearly 100% of those who have thoracic spinal cord injury that occurs before puberty will develop this disease. Although idiopathic scoliosis is much more common in girls than boys , neuromuscular scoliosis does not discriminate between the genders. Children who have undergone selective dorsal rhizotomy for spasticity control seem to have a higher incidence of spinal deformity than those who have not undergone this procedure .
| Cerebral palsy | Myelomeningocele | Duchenne’s muscular dystrophy | Spinal cord injury | Charcot-Marie-Tooth | Spinal muscular atrophy | |
|---|---|---|---|---|---|---|
| Scoliosis | 38%–64% | 20%–94% | 63%–90% | 100% (if injured before adolescent growth spurt) | 10% | 70%–100% |
| Hip dysplasia | 2%–60% | 1%–28% | 35% | 29%–82% | 6%–8% | 11%–38% |
Origin
The origin of idiopathic scoliosis is unknown, although genetic, environmental, and undetected neuromuscular dysfunction are hypothesized causes . In neuromuscular scoliosis, the situation is even more complex. Upright posture may be impaired because of abnormalities in the intricate coordination among central nervous system, muscle, bone, cartilage, and soft tissue. Asymmetric weakness, spasticity, abnormal sensory feedback, or mechanical factors such as pelvic obliquity or unilateral hip dislocation may cause an initial, flexible spinal curve. However, which parameter contributes most or even determines the direction of the curve is still unknown. No significant correlation between muscle asymmetry or side of dislocated hip and side of scoliotic convexity has been discovered . Whatever the origin or initial trigger, once a postural abnormality is present, a vicious cycle of progression may occur such that unequal compression on vertebrae causes unequal growth. Asymmetric growth may cause further unequal compression on the spinal structures, causing the cycle to perpetuate itself. If this cycle is sustained beyond a critical threshold of weight and time, fixed deformity with changes in vertebral and rib structure may follow, and spinal deformity develops . Various triggers may cause the imbalanced spinal axis, but biomechanical forces may account for its progression . Neuromuscular scoliosis is more likely to be rapidly progressive than idiopathic . Some evidence indicates, however, that if the underlying origin is corrected, such as spinal cord untethering, the spinal curvature may improve .
Evaluation
Many neuromuscular diagnoses are confirmed at or around birth. In those circumstances, subsequent evaluations occur with full knowledge of expected outcomes related to spinal deformity. However, conditions such as the hereditary motor sensory neuropathies may not be recognized until later in childhood, and scoliosis may be the presenting symptom. The history of a child who has scoliosis should include information about pre- and perinatal events; developmental milestones; evidence of skill regression; age of onset of symptoms; other system disorders or anomalies (especially renal and cardiac); the presence of associated symptoms such as sensory loss, weakness, or pain; functional deficits; and family history.
Therefore, idiopathic scoliosis is a diagnosis of exclusion. All children and adolescents who have scoliosis should undergo a careful neurologic and musculoskeletal examination. In one study, 23% of children referred to an orthopedic practice who had scoliosis and an atypical curve, congenital scoliosis, gait abnormality, limb pain, or weakness or foot deformity, had an MRI-identified spinal cord pathology . In children who have no known neuromuscular disease, MRI should be obtained when a rapidly progressive curve (more than 1° per month), left-sided thoracic curve, neurologic deficit, limb deformity, or worrisome pain symptoms are identified.
The physical examination should include evaluation for pelvic obliquity, shoulder girdle asymmetry, waist crease asymmetry, rib prominence, or asymmetry with spinal flexion, leg length discrepancy, fixed foot deformity, hip dislocation or subluxation, and limitation of spinal or extremity range of motion. A full neurologic examination should be performed, including an assessment of strength, muscle tone, reflexes (including abdominal reflexes), sensation, balance, cranial nerve function, speech and language, and cognition. A functional assessment is also an important component. Abnormalities in any of these areas may provide clues to origin, expected outcomes, and treatment strategies.
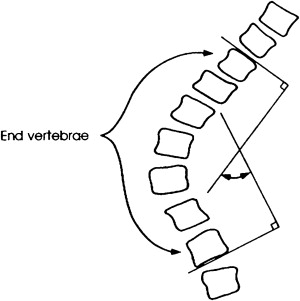
Radiographic evaluation includes a posteroanterior view of the entire spine. Standing films are most useful, although sitting films may be substituted when necessary. The Cobb method is the most commonly used technique to measure the degree of scoliosis ( Fig. 1 ). A widely accepted grading classification denotes a mild curve if between 10° and 40°, a moderate curve if between 40° and 65°, and a severe curve if greater than 65°. Intra- and interobserver measurement variability is within the range of 3° to 10° for noncongenital scoliosis . Curves are named for the location of the apex vertebrae, and are described as right or left based on their predominant convexity. They are designated C-shaped or double depending on their configuration. Idiopathic adolescent curves are more likely to be right-sided and thoracic in location. Experts have believed that neuromuscular curves have a higher incidence of left-sided convexity , although a recent retrospective study suggests that the curve patterns and apical levels in neuromuscular scoliosis are similar to those reported for idiopathic adolescent scoliosis . Before surgery, curve flexibility may be assessed using supine lateral bending, fulcrum, or traction radiographs .
Nonoperative treatment
If the vicious cycle can be disrupted or the continuous state of asymmetric loading can be prevented early enough that significant spinal bony deformity has not occurred, some experts are hopeful that the progression of scoliosis may be mitigated . A small body of literature suggests that exercise-based approaches in addition to bracing may be effective in some girls who have adolescent idiopathic scoliosis . However, the daily use of a spinal orthosis is the mainstay of treatment for girls who have idiopathic scoliosis.
The effectiveness of nonoperative treatment in children who have neuromuscular scoliosis is controversial. Although intuitively attractive, the theory that controlling the mechanical forces acting on the spine will result in decreased curve progression has infrequently been translated into clinical practice . Data are limited regarding efficacy of nonoperative treatment and bracing in preventing curve progression in neuromuscular scoliosis. Olafsson and colleagues reported on brace use in 90 consecutive children who had various types of neuromuscular scoliosis. They observed a 28% success rate (defined as curve progression of less than 10° per year and good brace compliance) with a higher likelihood of improvement in ambulators with hypotonia and short lumbar curves of less than 40° and in nonambulators with spasticity and short lumbar curves. Those who had longer, hypotonic curves experienced less success. In another group of children who had myelomeningocele and a curve not exceeding 45°, a Boston brace was used successfully to arrest or slow the progression of scoliosis in most . However, Miller and colleagues reported no benefit after 67 months of bracing in 20 children who had spastic quadriplegia related to curve magnitude, shape, or rate of progression. Whether spinal orthoses and other conservative management techniques may be helpful in slowing the progression of scoliosis in certain subpopulations of children who have neuromuscular disease remains to be seen, but the prevailing attitude suggests that they are not.
Nonoperative interventions, including sitting supports and custom seating, spinal orthoses, and functional strengthening programs may be useful to improve sitting balance and functional independence . In myelodysplasia, a soft thoracolumbosacral orthosis (TLSO) may be used to improve seating and positioning to free the upper extremities for functional tasks or as a temporizing measure to allow the child to develop increased trunk length before surgery .
Some are concerned that placing children who have neuromuscular disorders in a TLSO to improve postural function may cause further respiratory compromise, especially for children who have hypotonia. Bayar and colleagues treated 15 children who had neuromuscular scoliosis who used a polyethylene custom spinal orthosis for 8 to 10 hours and postural training, muscle strengthening, and stretching 5 days per week, with special emphasis on respiratory exercises for 4 weeks. Strength, range of motion, and balance improved although scoliosis did not. The forced vital capacity (FVC) while wearing the brace initially decreased by 18%. However, the negative effect on FVC lessened after the program, suggesting an improvement in coping with the restrictive effect of the brace. Further research showed that the use of a soft Boston brace did not impact negatively on the pulmonary mechanics and gas exchange in one group of children who had severe cerebral palsy and, in fact, decreased the work of breathing in some .
Special mention of boys who have Duchenne’s muscular dystrophy is warranted. Significant progression of scoliosis is unusual while the child remains ambulant. Rapid progression of scoliosis seems to be related to the loss of walking ability and commonly corresponds with a growth spurt in adolescence . The use of corticosteroids and orthotics, such as knee-ankle-foot orthoses , have been shown to prolong ambulatory ability. This intervention seems to significantly delay onset and decrease severity of scoliosis so that a much smaller proportion of boys who have Duchenne’s require surgical stabilization . Even without steroid treatment, not all boys who have Duchenne’s muscular dystrophy will need scoliosis surgery. It was recently recognized that up to 25% of nonambulant boys do not develop clinically significant scoliosis and therefore do not require surgical intervention . As with other neuromuscular disorders, the primary indication for bracing is to improve postural control and seating rather than prevent progression of curvature .
Surgery
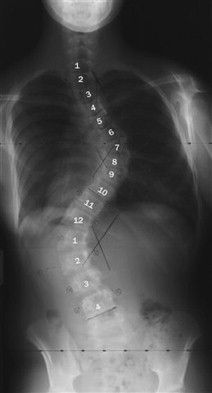
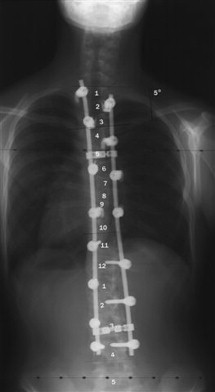
The goals of surgical stabilization for spinal deformity in neuromuscular disease include correcting the curvature, preventing significant progression of the curvature, improving the balanced position of the spine, and, therefore, improving quality of life. Indications for surgical intervention include progressive deformity that compromises ability to sit or stand, cardiac or pulmonary function, skin integrity, and ability to perform nursing cares, and causes pain ( Fig. 2 ). Reported outcomes of surgical intervention for neuromuscular scoliosis include improved Cobb angle, lung function, seating position and balance, and ability to perform activities of daily living, and decreased pain and time used for resting ( Fig. 3 ) . Self-esteem has also been shown to improve after surgery . In Duchenne’s muscular dystrophy, most data do not show a significant effect of scoliosis surgery on respiratory function or survival .
Various surgical techniques have been described and their merits debated. Surgical considerations include anterior and posterior fusion versus posterior-only fusion, one-stage versus two-stage procedures, various instrumentation techniques, and the extension of instrumentation across the lumbosacral junction and sacroiliac joint . From a surgical perspective, best results are achieved when the curve is progressive but not severe or rigid and when medical status is optimal .
Children who have neuromuscular scoliosis experience more complicated and costly hospitalizations from their scoliosis surgery than those who have idiopathic scoliosis. Before surgery, children who have neuromuscular disease are more likely to have gastrostomy tubes, failure to thrive, gastroesophageal reflux, and other medical diagnoses. Other challenges related to surgical procedures in children who have neuromuscular disease include curve severity that is characteristically worse and more rigid; osteoporosis; extension of deformity to include fixed pelvic obliquity; poor soft tissue coverage; deficiency of posterior spinal elements, such as in myelodysplasia; and tenuous neurologic status . Postoperatively, they experience a higher frequency of pneumonia, respiratory failure, mechanical ventilation, urinary tract infection, surgical wound infection, central line placement, transient or permanent neurologic loss, and failure of the surgical procedure or hardware .
Among children who had cerebral palsy who underwent scoliosis surgery, the number of days in the intensive care unit and the presence of severe preoperative thoracic hyperkyphosis negatively affected survival rate . Negative functional outcomes have been reported, such as loss of ability to roll, feed oneself, and walk .
Historically, children who have severe restrictive lung disease and an FVC of less than 30% of predicted have not been considered surgical candidates. However, several recent studies indicate that with aggressive team management by pulmonary, cardiac, anesthesia, and intensive care pediatric services, these children can safely undergo surgical spine stabilization without the need for tracheostomy or prolonged ventilation .
Rotational deformities of bone
Rotational malalignment of the lower extremities is a common outcome of neuromuscular disease. The spectrum of bony deformities has been referred to as lever arm disease . Rotational deformities often occur at the femur and tibia and have a deleterious effect on function and cosmesis. Muscle efficiency may be reduced because the skeletal lever arms are not aligned with the line of progression during gait. For example, in cerebral palsy, intoeing occurs commonly. The increased internal foot progression angle may place muscle groups at a mechanical disadvantage and be associated with poor foot clearance, tripping, and falling and a cosmetically poor gait pattern. Torsional deformities may also be associated with premature degenerative processes at the hip and knee .
Epidemiology
In a recent retrospective gait analysis study of 412 children who had cerebral palsy, 37% of intoeing gait had multiple causes. The most common contributors, either alone or in combination, were internal hip rotation in 55% and internal tibial torsion in 50%. Pes varus and metatarsus adductus also contributed . Although experts have previously suggested that spasticity of hamstrings and adductors contribute substantially to an internally rotated gait, more recent evidence suggests that intoeing in children who have cerebral palsy is almost universally associated with osseous deformity rather than hypertonia . The overall prevalence of excessive internal hip rotation in cerebral palsy is 27%, with prevalence higher in those who have diplegia than in those who have hemiplegia .
Etiology
Abnormalities of muscle strength and tone from neuromuscular disease are believed to be ultimately responsible for the development of rotational deformity. Femoral anteversion in able-bodied infants is not significantly different from that in infants who have cerebral palsy. The average newborn shows 30° to 40° of femoral anteversion. This decreases to 10° to 15° by adolescence in a typically developing population . However, children who have cerebral palsy are more likely to experience failure of the typical corrective lateral rotation that occurs with growth and development in their able-bodied counterparts . Persistent hip flexor spasticity and tightness are believed to contribute because they prevent normal extension of the hip and concomitant external rotation, thus the usual remodeling of the infant torsion cannot occur .
Similarly, remodeling and lateral derotation of the usual infant internal tibial torsion may not occur in neuromuscular disease. At birth, the malleoli are level in the frontal plane. In typically developing children, most normal external rotation of the tibia occurs by 4 years of age, with an additional degree per year occurring up until skeletal maturity for a final average of 28° of external rotation . Because of this lateral rotation of the tibia that occurs with normal growth, internal rotation abnormalities may improve with time. However, several factors, including muscle imbalance, soft-tissue contractures, associated congenital malformations, and mechanical abnormalities caused by habitually assumed posture over time, may impede this process causing internal tibial torsion to persist. In addition, other children, such as some who have myelomeningocele, may develop significant fixed external tibial torsion associated with valgus of the hindfoot, midfoot abduction, planus deformity, and genu valgum.
Evaluation of lower-extremity rotational deformity
Internal hip rotation, femoral anteversion, and medial femoral torsion all refer to an increased angle of the femoral neck relative to the transcondylar axis of the knee. In other words, the axis of the hip is anterior or external to that of the knee . Femoral anteversion may be assessed using physical examination, radiography, ultrasound, and CT scan and requires optimal positioning of the child for accurate measurement. The most commonly used physical examination maneuver (Craig’s test or the Ryder method) places the child prone with pelvis stable, hips extended, and knee flexed to 90°. The leg is then rotated outwardly with goniometric measurement of the angle between the shank and vertical. This angle is equal to the degree of femoral anteversion ( Fig. 4 ).
Tibial torsion is defined as the angle formed between the articular axes of the knee and ankle joint. Tibial torsion is often measured using an assessment of the thigh–foot angle. The child is placed prone with the knee flexed to 90° and the ankle supported in a neutral position. The axis of the foot is then compared with the long axis of the thigh. Alternatively, the degree of tibial torsion can be measured in a seated position, using a goniometer to measure the angle between the visualized bimalleolar axis and the femoral epicondylar axis.
Nonsurgical intervention for torsional deformities
Experts widely believe that traditional exercise, night splints, shoe inserts, twister cables, and other conservative options cannot reverse fixed femoral or tibial torsion . However, aggressive treatment of spasticity may help prevent development or slow the progression of torsional deformities. Short-term improvements in functional outcomes (gait, Gross Motor Function Measure, and clinical examination) using botulinum toxin injections have been reported, but evidence is limited regarding the effect of botulinum toxin treatment on the development of bony deformity. In a nested case-control design, Desloovere and colleagues reported an improved gait pattern characterized by fewer contractures at the level of the hip, knee, and ankle and decreased internal hip rotation at initial contact, toe-off, and mid-swing in children who had undergone multilevel botulinum A treatments. Botulinum injections were started at a young age and combined with common conservative treatment options. The authors concluded that children treated with multilevel botulinum A injections have a gait pattern less defined by bony deformity than their nontreated counterparts.
Surgery
Medial femoral torsion of greater than 40° to 45° that interferes with gait and function may be corrected surgically with a femoral derotational osteotomy ( Figs. 5 and 6 ). Both proximal and distal surgical techniques have been described. A proximal osteotomy may be beneficial when a child has both femoral torsion and hip subluxation to allow varus angulation of the femoral neck and ensure stability of the hip through proximal femur internal rotation and distal femur external rotation. However, when the hips are stable, distal osteotomies are reportedly less invasive, provide quicker recovery time, and are as effective as proximal surgery in functional and cosmetic outcomes . They also provide the added opportunity to correct a knee flexion contracture if needed. Long-term results indicate that partial recurrence of rotational deformity may occur in 0% and 33% of cases, with surgery before 10 years of age more likely to show deterioration . Some centers avoid postoperative casting and encourage early mobilization . Complications of femoral osteotomies include loss of fixation, delayed union, hardware failure, wound dehiscence or infection, and over- or undercorrection .
Tibial torsion can also be surgically corrected using a tibial derotational osteotomy ( Figs. 7–9 ). Various surgical techniques have been described, including proximal versus distal site of osteotomy, different shapes of osteotomy, various types of fixation, and possible simultaneous fibular osteotomy . Complications include delayed union, cross-union, or nonunion; wound dehiscence; osteomyelitis; late fracture; distal physeal closure; and neurovascular compromise . When combined with a split tibialis posterior tendon transfer for spastic equinovarus deformity, severe planovalgus or rigid equinovarus deformity has a higher rate of development presumably because of the increased difficulty in balancing the muscle forces across the spastic equinovarus foot .


Rotational deformities of bone
Rotational malalignment of the lower extremities is a common outcome of neuromuscular disease. The spectrum of bony deformities has been referred to as lever arm disease . Rotational deformities often occur at the femur and tibia and have a deleterious effect on function and cosmesis. Muscle efficiency may be reduced because the skeletal lever arms are not aligned with the line of progression during gait. For example, in cerebral palsy, intoeing occurs commonly. The increased internal foot progression angle may place muscle groups at a mechanical disadvantage and be associated with poor foot clearance, tripping, and falling and a cosmetically poor gait pattern. Torsional deformities may also be associated with premature degenerative processes at the hip and knee .
Epidemiology
In a recent retrospective gait analysis study of 412 children who had cerebral palsy, 37% of intoeing gait had multiple causes. The most common contributors, either alone or in combination, were internal hip rotation in 55% and internal tibial torsion in 50%. Pes varus and metatarsus adductus also contributed . Although experts have previously suggested that spasticity of hamstrings and adductors contribute substantially to an internally rotated gait, more recent evidence suggests that intoeing in children who have cerebral palsy is almost universally associated with osseous deformity rather than hypertonia . The overall prevalence of excessive internal hip rotation in cerebral palsy is 27%, with prevalence higher in those who have diplegia than in those who have hemiplegia .
Etiology
Abnormalities of muscle strength and tone from neuromuscular disease are believed to be ultimately responsible for the development of rotational deformity. Femoral anteversion in able-bodied infants is not significantly different from that in infants who have cerebral palsy. The average newborn shows 30° to 40° of femoral anteversion. This decreases to 10° to 15° by adolescence in a typically developing population . However, children who have cerebral palsy are more likely to experience failure of the typical corrective lateral rotation that occurs with growth and development in their able-bodied counterparts . Persistent hip flexor spasticity and tightness are believed to contribute because they prevent normal extension of the hip and concomitant external rotation, thus the usual remodeling of the infant torsion cannot occur .
Similarly, remodeling and lateral derotation of the usual infant internal tibial torsion may not occur in neuromuscular disease. At birth, the malleoli are level in the frontal plane. In typically developing children, most normal external rotation of the tibia occurs by 4 years of age, with an additional degree per year occurring up until skeletal maturity for a final average of 28° of external rotation . Because of this lateral rotation of the tibia that occurs with normal growth, internal rotation abnormalities may improve with time. However, several factors, including muscle imbalance, soft-tissue contractures, associated congenital malformations, and mechanical abnormalities caused by habitually assumed posture over time, may impede this process causing internal tibial torsion to persist. In addition, other children, such as some who have myelomeningocele, may develop significant fixed external tibial torsion associated with valgus of the hindfoot, midfoot abduction, planus deformity, and genu valgum.
Evaluation of lower-extremity rotational deformity
Internal hip rotation, femoral anteversion, and medial femoral torsion all refer to an increased angle of the femoral neck relative to the transcondylar axis of the knee. In other words, the axis of the hip is anterior or external to that of the knee . Femoral anteversion may be assessed using physical examination, radiography, ultrasound, and CT scan and requires optimal positioning of the child for accurate measurement. The most commonly used physical examination maneuver (Craig’s test or the Ryder method) places the child prone with pelvis stable, hips extended, and knee flexed to 90°. The leg is then rotated outwardly with goniometric measurement of the angle between the shank and vertical. This angle is equal to the degree of femoral anteversion ( Fig. 4 ).
Tibial torsion is defined as the angle formed between the articular axes of the knee and ankle joint. Tibial torsion is often measured using an assessment of the thigh–foot angle. The child is placed prone with the knee flexed to 90° and the ankle supported in a neutral position. The axis of the foot is then compared with the long axis of the thigh. Alternatively, the degree of tibial torsion can be measured in a seated position, using a goniometer to measure the angle between the visualized bimalleolar axis and the femoral epicondylar axis.
Nonsurgical intervention for torsional deformities
Experts widely believe that traditional exercise, night splints, shoe inserts, twister cables, and other conservative options cannot reverse fixed femoral or tibial torsion . However, aggressive treatment of spasticity may help prevent development or slow the progression of torsional deformities. Short-term improvements in functional outcomes (gait, Gross Motor Function Measure, and clinical examination) using botulinum toxin injections have been reported, but evidence is limited regarding the effect of botulinum toxin treatment on the development of bony deformity. In a nested case-control design, Desloovere and colleagues reported an improved gait pattern characterized by fewer contractures at the level of the hip, knee, and ankle and decreased internal hip rotation at initial contact, toe-off, and mid-swing in children who had undergone multilevel botulinum A treatments. Botulinum injections were started at a young age and combined with common conservative treatment options. The authors concluded that children treated with multilevel botulinum A injections have a gait pattern less defined by bony deformity than their nontreated counterparts.
Surgery
Medial femoral torsion of greater than 40° to 45° that interferes with gait and function may be corrected surgically with a femoral derotational osteotomy ( Figs. 5 and 6 ). Both proximal and distal surgical techniques have been described. A proximal osteotomy may be beneficial when a child has both femoral torsion and hip subluxation to allow varus angulation of the femoral neck and ensure stability of the hip through proximal femur internal rotation and distal femur external rotation. However, when the hips are stable, distal osteotomies are reportedly less invasive, provide quicker recovery time, and are as effective as proximal surgery in functional and cosmetic outcomes . They also provide the added opportunity to correct a knee flexion contracture if needed. Long-term results indicate that partial recurrence of rotational deformity may occur in 0% and 33% of cases, with surgery before 10 years of age more likely to show deterioration . Some centers avoid postoperative casting and encourage early mobilization . Complications of femoral osteotomies include loss of fixation, delayed union, hardware failure, wound dehiscence or infection, and over- or undercorrection .
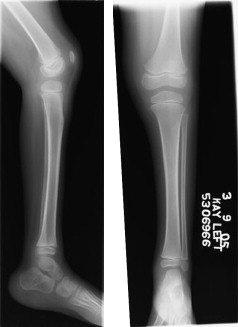
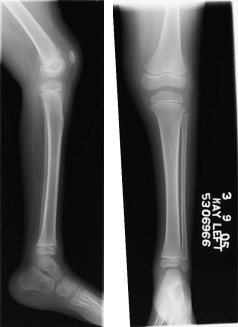
Tibial torsion can also be surgically corrected using a tibial derotational osteotomy ( Figs. 7–9 ). Various surgical techniques have been described, including proximal versus distal site of osteotomy, different shapes of osteotomy, various types of fixation, and possible simultaneous fibular osteotomy . Complications include delayed union, cross-union, or nonunion; wound dehiscence; osteomyelitis; late fracture; distal physeal closure; and neurovascular compromise . When combined with a split tibialis posterior tendon transfer for spastic equinovarus deformity, severe planovalgus or rigid equinovarus deformity has a higher rate of development presumably because of the increased difficulty in balancing the muscle forces across the spastic equinovarus foot .