Neurologic and Vascular Lesions
Walter G. Stanwood
Louis U. Bigliani
William N. Levine
Neurologic and vascular lesions around the shoulder in an athlete can present with signs and symptoms that may overlap with other causes and can be a diagnostic challenge. Often the patient’s complaints are vague and inconsistent. It is therefore imperative that the treating physician have a high index of suspicion when treating this patient population. This chapter outlines the diagnostic workup of the many neurologic and vascular lesions around the shoulder and presents both nonoperative and operative management of these challenging cases.
SUPRASCAPULAR NEUROPATHY
Historical Overview
Neuropathies of the shoulder are rare injuries and comprise less than 2% of all patients with pain and weakness in this region, which may lead to overlooking this diagnosis (1). In addition other diagnoses such as internal impingement, instability, and rotator cuff pathology may cloud the clinical picture in the overhead athlete.
Suprascapular neuropathy was first described by Andre Thomas in 1936 and was subsequently described as occurring at the suprascapular notch in the American literature by Kopella and Thompson (2,3). Initially repetitive motion was believed to be a primary etiologic factor. Since then numerous other causes of nerve injury have been described including tumors, ganglion cysts, traction injuries, and direct trauma (4, 5, 6).
Suprascapular neuropathy at the spinoglenoid notch was initially described by Ganzhorn and colleagues in 1981 and subsequently by Aiello and co-workers in 1982 (4,7). Volleyball players have been the subjects of the majority of spinoglenoid notch pathology (8, 9, 10, 11, 12), although suprascapular neuropathy has been described in baseball pitchers, archers, swimmers, weightlifters, football players, and tennis players (7,8,12, 13, 14, 15, 16).
Anatomy
The suprascapular nerve originates from the upper trunk of the brachial plexus, which is formed by the C5 and C6 roots. The nerve traverses the posterior cervical triangle, paralleling the omohyoid, and then under the trapezius muscle. It then passes through the suprascapular notch below the transverse scapular ligament. The suprascapular artery and vein parallel the nerve passing cephalad to the ligament. The variable anatomy of the suprascapular notch has been elucidated by Hrdlicka and others, which has theoretical implications in the development of symptoms at this site (5,17,18). Hypertrophy and calcification of the transverse scapular ligament has also been identified as sources of nerve injury (17,19,20).
After passing through the notch, the nerve begins to arborize, with a variable number of motor branches to the supraspinatus and sensory innervation to the glenohumeral joint, acromioclavicular joint, coracohumeral ligament, and coracoacromial ligament (21, 22, 23). Two thirds of the shoulder joint has sensory and sympathetic innervation from the suprascapular nerve (16). Additionally, a cadaveric study identified a cutaneous innervation of the nerve in the proximal-lateral one third of the arm in approximately 15% of the specimens (24).
An anatomic study by Bigliani and colleagues further defined the course of the suprascapular nerve, identifying two or more branches to the infraspinatus as it travels around the spinoglenoid notch (21). The presence of an inferior transverse scapular ligament at the level of the spinoglenoid notch has been reported with variable incidence of 3% to 80% in the literature (17,25,26).
Etiology of Injury
Overhead athletes continually put their arms in the extremes of motion that can create large torques about the shoulder. This can establish a cycle of repetitive microtrauma
to the nerve that can manifest itself in many ways. Injury can also be seen in the form of direct trauma to the nerve in the form of a fracture, dislocation, blunt trauma, or traction injury (4,5,27).
to the nerve that can manifest itself in many ways. Injury can also be seen in the form of direct trauma to the nerve in the form of a fracture, dislocation, blunt trauma, or traction injury (4,5,27).
Injury at the level of the suprascapular notch has been described by Rengachary and co-workers as well as others (5,28, 29, 30) as the sling effect, occurring with hyperabduction of the shoulder. A recent study demonstrated a correlation between increased shoulder range of motion and suprascapular nerve entrapment in symptomatic volleyball players (31). A vascular etiology for injury to this nerve has been discussed by Ringel and colleagues (14). They described an intimal injury to the axillary or suprascapular artery during the pitching motion that could cause microemboli to lodge in the vasa nervorum and cause an ischemic injury.
Feretti and associates have proposed a mechanism of injury by which an eccentric contraction of the infraspinatus during the overhead smash in volleyball creates tension on the nerve as it passes around the spinoglenoid notch (10). Alternatively, Sandow and others theorize that the supraspinatus in its confluence with the infraspinatus tendon compresses the nerve at the spinoglenoid notch in the position of maximal abduction and external rotation (9). This compressive effect is primarily produced by contraction of the supraspinatus muscle in this model.
Compression of the nerve by a ganglion cyst has been described with an incidence of 1% to 4.2% (17,32,33). Compression can occur at either the suprascapular notch or the spinoglenoid notch. Cadaveric and MRI studies have shown that the cyst commonly originates from labral pathology within the glenohumeral joint (17,32,33).
History and Physical Examination
Injury to the nerve along its course may produce varied symptoms. Patients may present after an acute event, but often they present after repetitive trauma that is subtler in onset. Most commonly, pain is the primary presenting symptom. It is usually localized to the posterior shoulder and can be characterized as a deep, dull ache that is exacerbated by their sports overhead shoulder motion. Ringel and associates revealed reproducible pain during the cocking and release phase of the pitching motion (14). A lesion at the level of the suprascapular notch is more likely to produce pain than a more distally based lesion (34,35). Accordingly, many patients may present with painless weakness of the affected shoulder (11,36). Numbness in the region of the posterolateral shoulder should also be considered as a presenting symptom (24,37).
Other important causes of shoulder dysfunction must be assessed. A complete physical examination rules out cervical spine disease, brachial plexopathy, glenohumeral pathology, and rotator cuff tears. Observation of atrophy within the supraspinatus or infraspinatus fossa can be helpful (Fig. 19-1). Diminution in abduction and external rotation strength may be demonstrated. Palpation at the apex of the clavicle and scapular spine may reproduce pain at the suprascapular notch. More distally based pathology may elicit symptoms at the spinoglenoid notch. A positive cross-body adduction test has been reported to be a useful diagnostic aid (29,35). With this test, the nerve is stretched at the level of the suprascapular notch, exacerbating the patient’s symptoms. Rose and Kelly have described a more invasive diagnostic test consisting of injection of local anesthetic into the notch. Resolution of symptoms can be helpful in confirming the diagnosis, but proper needle placement is imperative to prevent false-negative results (38).
Diagnostic Studies
All patients being evaluated for shoulder pathology should receive the standard shoulder series: anteroposterior (AP) in the scapular plane, scapular Y, and axillary radiographic views. To better assess the suprascapular notch, a Stryker notch view can be obtained. When osseous malformations or fractures have been excluded and the history and physical examination point to a nerve lesion, electrodiagnostic studies are a valuable adjunct in confirming the diagnosis. These studies are generally able to demonstrate neuropathy and its severity. Nerve conduction velocities show prolonged motor latencies from Erb’s point to the supraspinatus or infraspinatus, depending on the level of the pathology (34,35,39). Electromyography (EMG) shows fibrillations, positive sharp waves, decreased amplitudes, and polyphasics (16,34,40).
Magnetic resonance imaging (MRI) is a useful tool in imaging the soft tissues of the shoulder. It has been shown to be reproducible in identifying space-occupying lesions of the suprascapular nerve (6,33,41,42). Most commonly
these manifest as ganglion cysts. The course of the nerve is best seen on the T2-weighted sagittal oblique images (35). The supraspinatus and infraspinatus muscle bellies have been shown to demonstrate changes in their signal intensity with damage to the nerve (34). These include decreased muscle bulk, fatty degeneration, and altered signal intensity (6,9). However, these findings are nonspecific to denervation and can be seen independently in the face of rotator cuff tears (43,44).
these manifest as ganglion cysts. The course of the nerve is best seen on the T2-weighted sagittal oblique images (35). The supraspinatus and infraspinatus muscle bellies have been shown to demonstrate changes in their signal intensity with damage to the nerve (34). These include decreased muscle bulk, fatty degeneration, and altered signal intensity (6,9). However, these findings are nonspecific to denervation and can be seen independently in the face of rotator cuff tears (43,44).
Nonoperative Management
Nonoperative management of suprascapular nerve entrapment is indicated as the initial treatment modality. This has been successful in several studies, especially if the symptoms are not from a space-occupying lesion (36,40,45, 46, 47, 48). The true success of treatment is unknown because many of these studies were retrospective or case reports with a heterogeneous group of patients. It has been suggested that 6 to 12 months of nonoperative management is indicated before surgery should be considered. In a competitive overhead athlete, the compliance or tolerance for prolonged restricted involvement of activities is limited. Furthermore, these patients can have symptoms for 10 months to 2.8 years before presentation for surgery (8,40,49). In patients with advanced entrapment, there may be significant muscle wasting, which is often irreversible (16). This underscores the importance of a quick and accurate diagnosis to facilitate appropriate intervention.
Physical therapy is directed at preserving glenohumeral motion while strengthening the rotator cuff and deltoid, as well as providing scapular stabilization. Exercises directed toward scapular retraction and toward maintaining posture and strengthening of the trapezius, rhomboids, and serratus anterior are instituted (35). Local injections of steroids have also been described with limited success (50).
Operative Intervention
Decompression of the nerve at the level of the suprascapular notch has traditionally been performed through a posterior approach (51). The patient is typically in the semiprone or lateral position, although the beach chair position can be used (35). The incision is 10 to 12 cm and is parallel and cephalad to the scapular spine. The trapezius is elevated of the scapular spine superiorly. The supraspinatus is reflected posteriorly, exposing the notch. Once the suprascapular artery and vein have been retracted, the transverse scapular ligament is transected, while protecting the nerve beneath. Osseous malformations of the notch causing impingement of the nerve are also addressed at this time.
The posterior approach may also be used when addressing isolated pathology at the spinoglenoid notch. The incision is placed directly overlying the spine or just caudad to it. The deltoid is split in line with its fibers or may be taken down off of the spine. The infraspinatus belly is dissected off of the spine and retracted inferiorly. Judicious dissection through the vascular fibrous tissue overlying the notch reveals the nerve as it delivers branches to the infraspinatus (22). Hama and colleagues and Sandow and associates have illustrated a technique of deepening the spinoglenoid notch to address the suprascapular nerve at this level (9,52). Caution should be exercised with this technique, because removal of more than 1 cm may predispose to fracture at the acromial base. Both of these series deal with high-level volleyball players. All patients in both series had resolution of pain and return to their previous level of competition (9,52). Ringel and colleagues reported on a series of two professional pitchers who underwent decompression of the nerve (14). One patient had no visible area of compression at the suprascapular notch or the spinoglenoid notch. The second patient had an anomalous motor branch to the supraspinatus that traveled over the transverse scapular ligament. Both returned to pitching for their respective teams. Vastamaki and Goransson reported on a mixed population of laborers and those with athletic injuries (12). Overall, 72% had complete relief or minimal pain; 81% rated their result as excellent or good at a minimum of 5.6 years of follow-up. A recent study compared the outcomes of nonoperative versus operative treatment (40). Overall, there was improvement noted in both groups, but significantly more in the operative group. Patients with traumatic lesions improved with either nonoperative or operative management, but there was no significant difference between the two groups. Compressive lesions did significantly better with surgery than with nonoperative treatment.
Successful decompression of the nerve secondary to compression from a ganglion cyst has been reported with both open and arthroscopic means (4,53, 54, 55, 56, 57, 58, 59, 60, 61). However, an open approach to the nerve does not allow surgical repair of the labral pathology that is invariably present. This may account for the recurrences that have been documented (58,62). An open or arthroscopic approach to decompression of the cyst with concomitant arthroscopic management of the labrum has shown reproducible results (35,58,59,61). The one recurrence noted with this approach was thought to be secondary to unrecognized labral pathology at the index procedure (58).
Authors’ Preferred Method
The approach to open management of suprascapular nerve entrapment at our institution is similar to that of Post (51). A posterior approach with an incision parallel to the spine of the scapula is used. It is placed just cephalad or caudad to the spine, depending on whether the pathology is at the suprascapular or spinoglenoid notch, respectively. The trapezius muscle is not split; rather, elevation of the entire trapezius off the spine is performed to prevent injury to the spinal accessory nerve during retraction. Judicious dissection
of the fatty layer underlying the trapezius exposes the supraspinatus. Access to the suprascapular notch is facilitated with minimal retraction of the supraspinatus inferiorly. The transverse scapular ligament is defined with the use of a small sponge stick, while the overlying artery and vein are retracted. The nerve is protected below and the ligament is transected.
of the fatty layer underlying the trapezius exposes the supraspinatus. Access to the suprascapular notch is facilitated with minimal retraction of the supraspinatus inferiorly. The transverse scapular ligament is defined with the use of a small sponge stick, while the overlying artery and vein are retracted. The nerve is protected below and the ligament is transected.
If the nerve is involved at the level of the spinoglenoid notch, the supraspinatus is retracted superiorly and the infraspinatus inferiorly. The inferior transverse scapular ligament, if present, is transected and the notch is deepened with a high-speed burr. The osseous resection is limited to 1 cm to minimize potential iatrogenic fracture of the acromion base (9).
AXILLARY NERVE INJURY
Historical Overview
Axillary nerve injuries account for less than 1% of all nerve lesions, but are the most common peripheral nerve injury to the shoulder (63,64). It has been described as an injury in contact sports, with direct blunt injury, traction, and dislocation being the most common mechanisms (65, 66, 67). The quadrilateral space syndrome also involves the axillary nerve, in addition to the posterior humeral circumflex artery. This entity was originally described by Cahill and Palmer and is seen primarily as a noncontact injury and therefore is a more plausible etiology for dysfunction in the overhead athlete (68).
Anatomy
The axillary nerve is a terminal branch of the posterior cord of the brachial plexus arising from the C5 and C6 nerve roots. It courses along the subscapularis obliquely from superomedial to inferolateral, crossing 3 to 5 mm from the musculotendinous junction (69). It then passes through the quadrilateral space with the posterior humeral circumflex artery. This space is bound by the teres minor superiorly, the teres major inferiorly, the long head of the triceps medially, and the shaft of the humerus laterally. After exiting the space, the nerve forms two major trunks. The anterior trunk continues around the humeral shaft to give branches to the middle and anterior deltoid on the undersurface of the muscle. The posterior trunk supplies the posterior deltoid and the teres minor. The branch to the teres minor arborizes while in the quadrilateral space or just after exiting. Ultimately, the posterior trunk becomes the superior lateral brachial cutaneous nerve.
Etiology
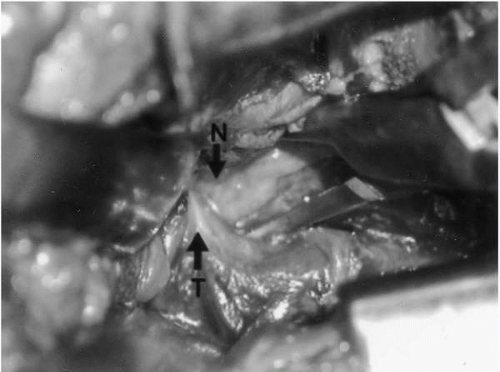
The overhead athlete who sustains an anterior shoulder dislocation is at risk for an axillary nerve injury, although this is relatively uncommon in persons younger than age 50 years (70,71). Direct blows to the lateral shoulder have been noted to cause axillary nerve injury in contact athletes (65,72). This mechanism of injury is less common in the overhead athlete. A more likely etiology in this subset of patients is the quadrilateral space syndrome. As the axillary nerve and posterior humeral circumflex artery traverse the space, it is possible that they can become compressed. Overuse of the extremity may cause the formation of fibrotic bands or hypertrophy of the long head of the triceps tendon causing compression (1,68,73). This triceps pathoanatomy has been demonstrated at our institution (see Fig. 19-1). Most of the recent cases of quadrilateral space syndrome have involved overhead athletes, providing additional support that repetitive motion is integral to the pathology (74, 75, 76, 77). This theory is further supported by the fact that the syndrome is rarely seen in the inactive elderly population (68,76,78).
History and Physical Examination
The overhead athlete, in the absence of acute trauma, may present to the clinician with vague complaints of easy fatigability of the arm while playing their sport, poorly localized pain in the posterior shoulder, and numbness to the lateral shoulder. Often, these patients are able to compensate for the loss of deltoid function for activities of daily living. In the overuse patient, symptoms can be insidious in onset and may have been undiagnosed or misdiagnosed.
Sensation over the deltoid should be assessed, noting any paresthesias. However, complete deltoid motor loss can occur in the face of minimal sensation loss. Atrophy of the deltoid and teres minor should be assessed. Squaring of the shoulder is observed with significant denervation of the deltoid. Muscle wasting can be more difficult to assess in incomplete lesions of the deltoid. These patients may retain full range of motion, but when the extremity is exercised they demonstrate abduction weakness (67). Delineating the function of the deltoid from the rotator cuff through extension of the shoulder has recently been proposed by two independent authors. Nishijima and colleagues have described the swallow-tail sign, wherein the injured shoulder is unable to extend fully with respect to the contralateral side (79). The deltoid extension lag sign has been described by Hertel and co-workers (80). When the arm is passively brought into full extension, the patient is unable to maintain this position when support is withdrawn and the arm drops.
In an athlete suspected of having quadrilateral space syndrome, palpation over the space reliably reproduces their pain (68,76,78). Placement of the arm in an abducted and externally rotated position for 1 minute may reproduce symptoms (68). Paresthesias were originally described as occurring in a nondermatomal pattern in the arm and forearm, although subsequent reports are variable in accounting for their presence.
Diagnostic Studies
Plain radiographs should be obtained to rule out any osseous pathology. Electrodiagnostic studies are an important part of the workup in a patient with a suspected nerve lesion. In the face of known blunt injury or dislocation, EMG is especially useful. These studies should not be performed before 3 weeks from the injury because fibrillation potentials are not evident until that time. Repeat studies should be performed 3 months after injury if no clinical improvement is noted, because electrical improvement in the nerve may be present despite the clinical picture.
In the case of the overhead athlete, acute trauma is less likely and the diagnosis of quadrilateral space syndrome should be considered. The use of EMG in this setting has been reported with variable success, but it may aid in confirmation (68,76, 77, 78,81).
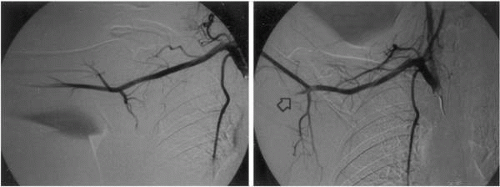
Although quadrilateral space syndrome has been described as primarily a lesion of the axillary nerve, arteriography is essential to its diagnosis. With the arm at the side, the posterior humeral circumflex artery is patent; when the arm is brought into abduction and external rotation, the artery occludes (Fig. 19-2). This finding has been described as pathognomonic for this syndrome (68,74,76, 82, 83, 84).
Atrophy and fatty degeneration have been described in the radiologic literature as useful findings on MRI (85,86). A case report of a paralabral cyst extending into the quadrilateral space has been documented on MRI (86). Despite these reports, support for its widespread use in this setting has not been subsequently substantiated.
Nonoperative Management
The body of literature that exists for nonoperative management of axillary nerve pathology in athletes is largely from a traumatic etiology. Perlmutter and co-workers reported on axillary nerve injury following a direct blow to the shoulder in 11 football players (72). Nonoperative treatment consisted of rotator cuff, deltoid, and periscapular muscle strengthening. Four of the 11 patients eventually required surgical exploration for persistent clinical and electromyographic deficiencies. Ten of the 11 ultimately returned to their prior level of participation. All patients had good to excellent manual muscle testing results, although cutaneous sensory abnormalities persisted in all of the patients.
In another series addressing peripheral nerve injuries in sports, there were six axillary nerve injuries. Five of six resolved with physical therapy alone. Redler and colleagues presented successful nonoperative management of a pitcher with quadrilateral space syndrome (75). Retraining from an overhead motion to three quarters was instituted. Additionally, internal rotation stretching of the shoulder joint, horizontal stretching in adduction, and rotator cuff strengthening have been advocated with quadrilateral space syndrome (82).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree