27 MUSCULOSKELETAL INJURIES
Management of traumatic musculoskeletal injuries rarely takes precedence during the initial phases of trauma care. The basic principles of trauma care stress resuscitation and therapeutic interventions for those life-threatening injuries most commonly associated with trauma. Musculoskeletal injuries are considered part of the secondary trauma survey unless those injuries result in significant hemodynamic instability, such as traumatic amputations and massive pelvic injuries. Musculoskeletal injuries require prompt recognition and appropriate management after stabilization of the cardiopulmonary and neurologic systems to maximize the patient’s full recovery.
ANATOMY AND PHYSIOLOGY
FUNCTIONS
The musculoskeletal system is composed of two systems: the skeletal system and the skeletal muscles. The skeletal system is composed of bones and joints, and its main functions are to provide support, protection, storage of mineral salts and fats, and hematopoiesis (red blood cell production). The skeletal system also provides the leverage needed by skeletal muscles to produce movement through contraction of skeletal muscles and bending and rotation at joints.1 Any injury to the musculoskeletal system that affects any of these functions may be detrimental to the patient.
STRUCTURES
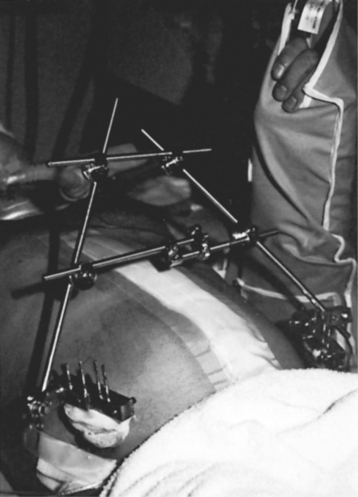
Figure 27-1 illustrates normal bone architecture, including articular cartilage, spongy bone, epiphysis, epiphyseal plate, compact bone, medullary cavity, diaphysis, and periosteum. There are two types of bone tissue: compact bone (cortical bone) and spongy bone (cancellous). Compact bone is organized, strong, and solid and contains structural units, called haversian systems. The haversian system, which contains bone cells called osteocytes, provides a vehicle for the major metabolic processes of compact bone, transporting nutrients to and removing wastes from the osteocytes.1 Spongy bone is less organized and does not contain haversian systems. Spongy bone is characterized by trabeculae, or plates, that branch out to form an irregular meshwork. Stresses placed on the bone form the pattern of trabeculae, and the spaces between the trabeculae are filled with red bone marrow.1
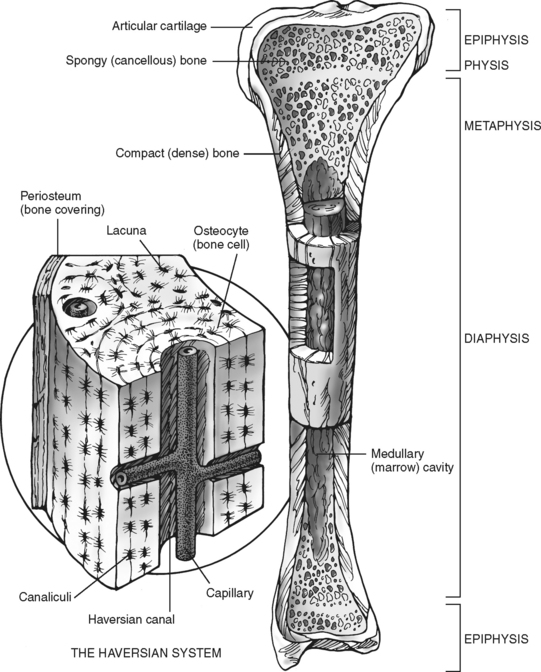
FIGURE 27-1 Diagram of longitudinal section of a long bone and Haversian system.
(From Ignatavicus DD, Bayne MV: Medical-surgical nursing: a nursing process approach, Philadelphia, 1991, W. B. Saunders, p 719.)
The periosteum is a fibrous membrane sleeve that covers the entire bone except for the cartilaginous ends. The inner osteogenic layer of periosteum consists of elastic fibers, vessels, and osteoblasts, which are responsible for new bone formation. The outer fibrous layer is made up of connective tissue and it houses blood and lymphatic vessels and nerves. Bone growth, repair, and nutrition depend to a large extent on an intact and healthy periosteum. This closely adherent covering is thickest where muscles surround the bone, such as at the diaphysis of the femur. Because it is a thin and tightly bound membrane in adults, it usually tears at fracture sites and occasionally separates from the bone. When a low- energy fracture occurs, one side of the periosteum may remain intact (the periosteal hinge). The remaining portion of intact membrane aids fracture reduction and maintenance and serves as an osteogenic covering that promotes healing. The degree to which the periosteum is damaged during a fracture event often determines the course of healing of the fracture.
BONE CELLS
Bone contains three types of cells: osteoblasts, osteocytes, and osteoclasts. Each type of cell plays a major role in the formation, repair, and cyclic remodeling of bone. Osteoblasts are bone-forming cells whose major function is to lay down new bone. Once this is accomplished, they become osteocytes. Osteocytes are osteoblasts that have become trapped in the bone matrix.1 Their major function is not well defined, but it is postulated that they function to maintain the bone matrix.1 Osteoclasts are the major resorptive cells of bone and function primarily during periods of growth and repair.1 Any process that interferes with the function of these bone cells can adversely affect the dynamic state of skeletal tissue. Approximately 18% of bone is removed and replaced every year in premenopausal women; after menopause this balance changes to an increase in bone resorption and a decrease in bone production, leading to the development of osteoporosis.
EPIDEMIOLOGY
Approximately 29 million musculoskeletal injuries occur annually, including 20 million fractures, dislocations, and sprains, with approximately 8,000 deaths.2 These deaths are directly attributed to musculoskeletal injuries and there are many more patients with multiple injuries where fractures contribute to overall injury load and risk of death. Musculoskeletal injuries account for almost half of all injuries, and those found in the trauma patient result from a variety of causes.2 The major causes of significant musculoskeletal injuries are vehicular crashes; falls; industrial, home, and farming incidents; and interpersonal violence. Musculoskeletal injuries are often associated with serious injuries to other body systems.2
RESUSCITATION PHASE
ASSESSMENT
Prehospital Database
A variety of energy sources can traumatize the musculoskeletal system. Each type of impact exerts a different amount of force on the body. The degree, direction, and duration of that force, along with the patient’s age and health history, determine the severity of the injury and its resulting morbidity.3
Information concerning the mechanism of injury should be obtained from the patient if possible and from the prehospital care providers. Important information to obtain is summarized in Table 27-1. Similar injuries can occur in different environments, and the sequelae of an open fracture can be very different if the injury occurred in a farming incident versus a fall at home. Pathogenic organisms found in soil can cause serious, even fatal, infections. Early identification of environmental factors can decrease complications if appropriate interventions are started early in the treatment phase.
TABLE 27-1 Prehospital Database
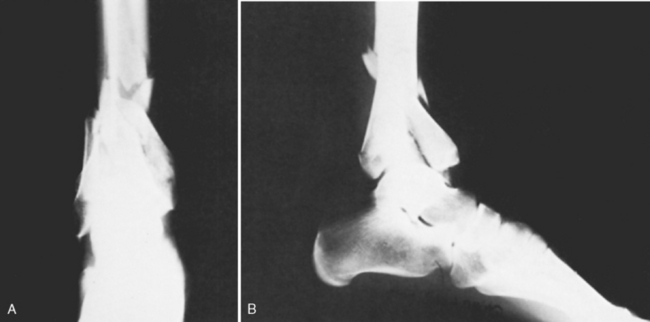
Each musculoskeletal injury is the result of absorbed and transferred energy. The fall victim who lands on his or her feet may have obvious ankle injuries, but other injuries often associated with this type of mechanism, such as pelvic and lumbar spine fractures, may be occult (Figure 27-2). Other patterns of energy absorption and transfer are demonstrated in Figure 27-3. Information concerning events of extrication, immobilization, and stabilization that occurred at the site of the incident is important and should be obtained from the prehospital care providers.3 Knowing the degree of angulation of a fracture, attitude of a joint, neurovascular status of the extremity at the scene, amount of exposed bone, and estimated blood loss heightens suspicion and helps determine the type of treatment necessary. Review Chapter 12 for further discussion of mechanism of injury.
Musculoskeletal Physical Assessment
Attention is directed toward the musculoskeletal system during the secondary survey. Any suspected or obvious musculoskeletal injuries require baseline assessment of neurovascular and motor status, proper immobilization of affected extremities, including splinting or traction, and application of sterile dressings to open wounds. Additionally, an unstable pelvic ring disruption (as identified on initial radiographs) with possible vascular injury may require application of a pelvic binder to prevent exsanguination.4,5 External fixators or pelvic C clamps may be used in rare situations when binders are ineffective. Other interventions are typically not initiated until the total patient evaluation has been completed and the patient is hemodynamically stable.
Areas of suspected musculoskeletal injury should remain immobilized to prevent further soft tissue, bone, nerve, or vascular damage. Whenever the patient requires turning or moving, one person assumes responsibility for the affected limb to maintain alignment and immobilization. This is critically important when caring for patients with suspected spinal column injuries because any motion at the fracture or dislocation site may result in spinal cord damage and dysfunction.6
Continuous monitoring is an important concept for emergency personnel. After primary and lifesaving measures are instituted, it is essential that providers reassess the patient’s status, especially the neurovascular function of extremities with obvious or suspected fractures. Physiologic events, such as muscle spasms, or environmental events, such as transports, can further displace fracture fragments and lead to serious neurovascular compromise of the affected extremity. If undetected, neurovascular compromise can cause permanent disability, loss of limb, or even death.
Inspection and Palpation.
Assessment of the musculoskeletal system in a systematic fashion decreases the chance of missing an injury. Assessment involves inspection and palpation.7 The position of the patient and the extremities should be observed. Note is made of any deformities such as angulation, shortening, or rotation; open wounds; obviously protruding bone ends; abrasions; and road burns.
The patient is examined for additional evidence of musculoskeletal injury:
• Ecchymosis: caused by vascular disruption with blood dispersing through soft tissue
• Muscle spasm: continuous muscle contraction over an area of injury; considered a protective mechanism of the muscle to splint the injured part
• Swelling: caused by injury to the soft tissue and interruption of the venous and lymphatic return system
• Extremity color: pale color indicates inadequate arterial blood supply; dusky, bluish color indicates venous congestion
• Capillary refill time: A filling time longer than 2 seconds is considered abnormal and may indicate vascular compromise. Factors such as ambient air temperature, patient’s core body temperature, and presence of shock may affect the capillary refill time.
• Pulses: Quality and equality are evaluated over the entire length of an extremity, not just distal to an obvious injury; results are compared with pulses in the unaffected extremity.
• Crepitus: A grating sound is heard and felt when fractured bone ends move.
• Muscle spasm: As noted above. Lack of spasms over an obvious fracture may indicate a neurologic lesion above the fracture, preventing contraction of the muscle.
• Movement: Range of motion, both passive and active, is assessed. Deviation from normal range or limitation of motion or muscle strength is noted. Obviously injured extremities should not be tested for range of motion because of the risk of increasing the damage to surrounding neurovascular structures.
• Sensation: Sensory perception in response to sharp and dull stimuli and proprioception are assessed. Absent or altered senstation may indicate neuronal compression or injury
• Pain: Pain is usually caused by injury to the periosteum (the only part of bone with sensory innervation), muscle spasm, soft tissue disruption, and swelling within fascial compartments.
Zone of Injury.
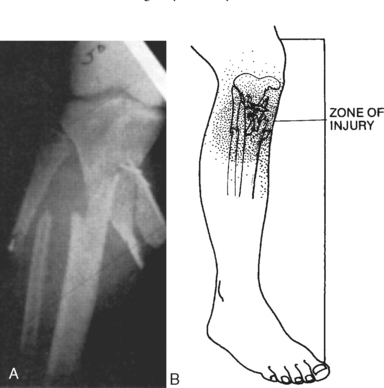
The zone of injury is the area affected by traumatic forces, as seen in Figure 27-4. Injuries to the skeletal system are always accompanied by some degree of soft tissue injury. Damage to the soft tissue structures is often greater than what is discovered on clinical assessment and radiologic examination. The exact zone of injury is often not fully appreciated until the time of operative intervention; therefore, continued physical assessment is important with close observation of areas both distal and proximal to any obvious or suspected musculoskeletal injury.
Diagnostic Studies.
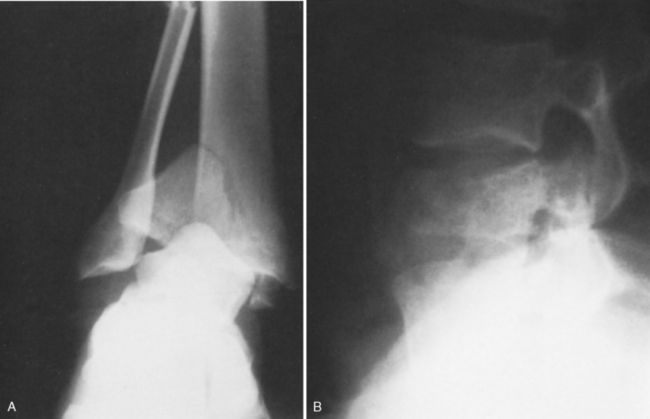
Various radiographic studies are used to confirm or exclude musculoskeletal injuries. For plain radiographic films, at least two views are required to determine the degree of angulation and displacement (Figure 27-5). Inlet and outlet views of the pelvis, taken from superior and inferior angles, can be done in the resuscitation room to further define significant pelvic injuries and aid clinicians in their early treatment. Surrounding anatomic structures or the structure of the bone or joint in question may reduce the effectiveness of plain films in diagnosing skeletal injuries and necessitate the use of other techniques such as computed tomography (CT) scans or magnetic resonance imaging (MRI). CT scans aid in confirmation of hidden or minimally displaced fractures in areas such as the cervical spine, pelvic ring, ankle, and knee. MRI studies are often performed to aid in the diagnosis of suspected soft tissue injuries such as herniated intervertebral disks or ligamentous disruption. Angiography may be helpful in assessing vascular injuries associated with musculoskeletal trauma.8
When diagnostic procedures are performed, the nurse is responsible for the following:
1. Assisting with explanation of the procedure to the patient and ensuring that consent is obtained when necessary
2. Ensuring that the patient has no known allergy to agents that are to be administered during the procedure
3. With the patient receiving contrast medium, adequately hydrating and, if prescribed, administering prophylaxis to prevent contrast-induced renal nephropathy
4. Assisting with safe patient positioning during and after the procedure to prevent further injury- or procedure-related complications. For example, after an angiogram in which the femoral artery is cannulated, hip flexion is restricted for 6 to 8 hours to prevent further bleeding at the insertion site.
5. Protecting the patient from unnecessary radiation exposure by shielding with a lead-lined apron whenever possible
6. Constantly monitoring the patient’s overall status, including potential reaction to contrast media
7. Documenting the procedure, patient response, and follow-up evaluation
Patient Health History.
Eliciting a specific patient health history is an important part of the patient assessment. Information concerning the health history can be obtained from the patient or, when necessary, from family members or friends. The nurse should determine whether the patient has ever had an allergic reaction to any medication or contrast material and the type of reaction that occurred. Previous reactions to pharmacologic agents can alter the choice of diagnostic studies or the choice of medications used for treatment. Current or recent use of medication and the reason, dose, and frequency are ascertained if possible. Learning whether the patient has taken any anticoagulants, antiplatelet agents, nonsteroidal anti-inflammatory drugs, or other medication is essential. The patient’s tetanus immunization history is also important. Other helpful information includes previous hospitalizations and surgeries, anesthesia-associated problems, and any specific health problems. Previous fractures, ligamentous or soft tissue injuries, thromboembolic disease, neurologic disorders, smoking history, and problems with infection or delayed healing potentially affect the patient’s treatment and recovery.7 The importance of obtaining an AMPLE (Allergies, Medications, Past medical history, Last meal, Environment) history during the initial assessment cannot be overemphasized because this history guides the clinician’s assessment and treatment of the trauma patient (Table 27-2).
| A | Allergies |
| M | Medications currently used (including herbals and over the counter) |
| P | Past medical illnesses/pregnancies |
| L | Last meal |
| E | Environment/events of incident (mechanisms of injury) |
Source: American College of Surgeons’ Committee on Trauma: Advanced trauma life support, 7th ed, Chicago, 2004, American College of Surgeons.
Classification of Injuries
Extremity Fractures.
The classification of a fracture is based on several factors: (1) type of fracture line (spiral, transverse, oblique), (2) whether the fracture is linear or comminuted (number of fracture fragments), (3) anatomic location (distal, middle, proximal third of the shaft, intra-articular), (4) type of displacement (angulation, translation, impaction, distraction), and (5) position of the displacement in relation to other fragments9 (Figure 27-6).
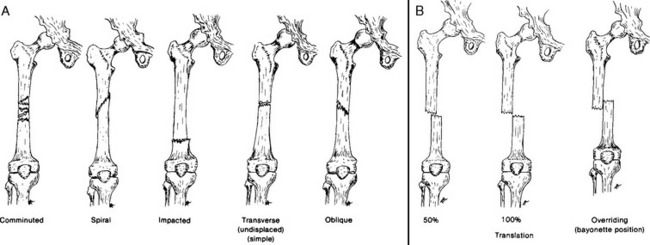
FIGURE 27-6 A, Types of fractures. B, Translation.
(From Stearns HC: Principles of lower extremity fracture management. In Hilt N, editor: Assessment and fracture management of the lower extremities [monograph], Pitman, NJ, 1984, National Association of Orthopaedic Nurses.)
A fracture with associated interruption in skin integrity is an open fracture. An open fracture is further classified according to the degree of soft tissue involvement and the amount of disruption in skin integrity. A type I open fracture is small with minimal (less than 1-cm wound) soft tissue damage and a low-energy fracture pattern. A type II open fracture is larger (1- to 10-cm wound) with a moderate amount of soft tissue injury. A type III open fracture is associated with significant soft tissue damage and possible neurologic or vascular involvement. All open fractures with high-energy fracture patterns are considered type III open fractures regardless of actual wound size. Type III fractures are further subclassified as IIIA, IIIB, or IIIC depending on the degree of soft tissue loss and the presence of vascular injury requiring repair9 (Table 27-3).
TABLE 27-3 Classification of Open Fractures
| Type | Description |
|---|---|
| I | |
| II | |
| III | |
| IIIA | |
| IIIB | |
| IIIC | Any open fracture associated with arterial injury that must be repaired regardless of degree of soft tissue injury |
Modified from Snyder P: Fractures. In Maher AB, Salmond SW, Pellino, TA, editors: Orthopaedic nursing, Philadelphia, 2002, W. B. Saunders.
Certain mechanisms of injury automatically classify an open fracture as type III, such as a shotgun injury, a high-velocity gunshot wound, an open fracture occurring in a farm environment, and a crushing injury from a fast-moving vehicle. The time elapsed from open injury to operative debridement of open fractures also influences fracture classification. However, the relationship between time to operative debridement and infection risk is unclear for most fracture types (Figure 27-7).
Traumatic Amputation.
Traumatic amputations are associated with soft tissue, nerve, and vascular injury. The zone of injury is important to clinical decision making regarding treatment plans for managing these injuries.10
The advent of newer and more sophisticated microsurgical techniques used for reattachment of severed limbs has made it imperative that all prehospital and hospital personnel correctly care for the amputated limb until a determination can be made regarding the feasibility of surgical reattachment. Amputated parts should be placed in a plastic bag and then placed in another bag containing ice water and transported with the patient. Direct contact with iced solutions can cause freezing and crystallization with subsequent rupture of tissue cells, thus making successful reattachment less likely. Dry ice should never be used as a cooling agent because it increases crystal formation. Amputations caused by crush or avulsion injuries have a low reattachment success rate; therefore, the procedure is usually not attempted.
Dislocation.
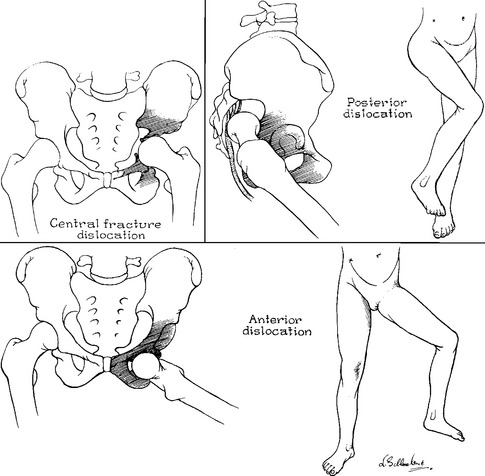
A dislocation occurs when articulating surfaces are no longer in contact because of joint disruption. Movement can be limited or impossible. The dislocation is described in terms of the position of the distal component relative to the proximal component. For example, a dislocation of the elbow involving the radius alone can be anterior, posterior, or lateral. Hip dislocations may be classified as anterior, posterior, or central (Figure 27-8). The incidence of neurovascular injuries associated with major joint dislocations is high; thus, careful assessment of distal neurovascular function is necessary. The ligamentous structures surrounding the dislocated joint may be severely stretched or completely disrupted, leaving the joint unstable. Immobilization is essential to prevent or limit the neurovascular compromise often found with these injuries. Dislocations are often easily recognized clinically without the aid of diagnostic studies. A dislocation may also occur at the time of impact and then either reduce spontaneously or during application of an immobilization device at the scene of the incident. For this reason, it is important to obtain a history from either the patient or the prehospital care providers concerning any “popping” or “snapping” of a joint that may have been felt or heard.
Pelvic Ring Disruption.
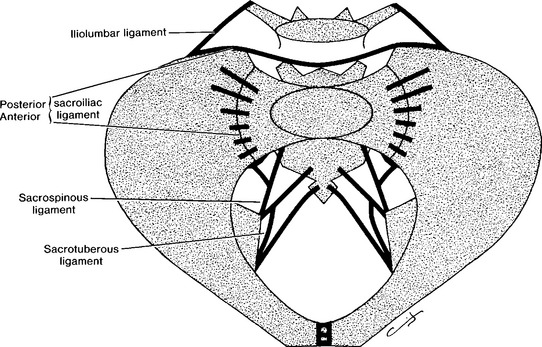
The pelvis is composed of three bones held together and stabilized by a ligamentous network. Anteriorly the symphysis pubis, a strong ligamentous structure, acts as a band to prevent anterior pelvic widening, and it has little to do with weight bearing. The major stabilizing force in the pelvis is the posterior tension band that includes the following ligaments: iliolumbar, posterior sacroiliac, anterior sacroiliac, sacrospinous, and sacrotuberous (Figure 27-9).
Pelvic ring disruptions are commonly associated with fatal motor vehicle crashes.11 These disruptions to the pelvic ring are clinically described as stable or unstable. Two thirds of pelvic ring disruptions are stable.12 Although fewer in incidence, the unstable injuries are potentially more life threatening and debilitating because they are often accompanied by many additional structural disruptions and complications. These may include massive to exsanguinating blood loss resulting from venous or arterial injury, genitourinary trauma, sepsis, chronic pain, and long-term disability. Injuries to the pelvic ring may be closed or open, as with an associated laceration or puncture of the skin, rectum, or vagina. The mortality rate associated with open pelvic fractures has been reported to be as high as 70%.12,13
Various systems exist for classification of pelvic injuries, such as those described by Trunkey et al,14 Pennal et al,15 and Young and Burgess.16 One commonly used classification system, described by Tile,17 categorizes pelvic ring disruptions by their mechanism of injury and their degree of stability. The four major types of injury are anteroposterior compression, lateral compression, vertical shear, and complex. Subdivisions exist within some categories; however, this chapter addresses only the four major categories.
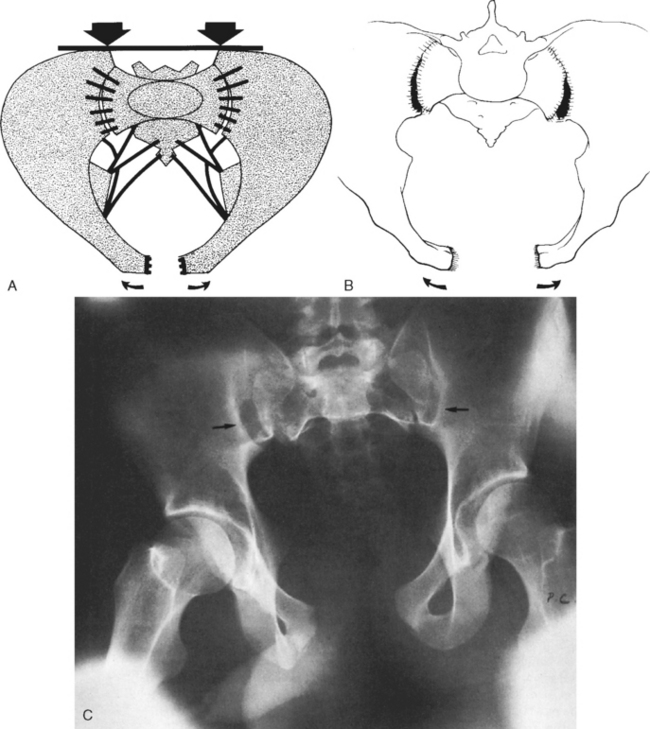
An anteroposterior compression injury (Figure 27-10), or external rotation injury, may occur when an anterior- to posterior-directed force causes the anterior pelvic ring to open. Continued external rotation causes rupture of the anterior sacroiliac and sacrospinous ligaments. As widening continues, the sacroiliac ligaments or posterior bony structures may be injured.
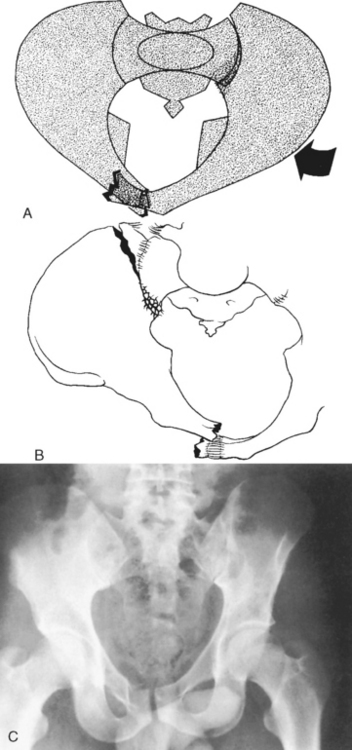
Lateral compression (Figure 27-11), or internal rotation, is the most common type of pelvic injury. Direct pressure to an iliac wing causes an internal rotation injury that crushes the anterior sacrum and fractures the pubic rami anteriorly. Pressure on the greater trochanter causes the femoral head to disrupt the pubic rami, which can extend into the anterior acetabulum. The ipsilateral sacroiliac complex may also be injured by this force. This injury typically causes bone impaction in the sacrum or ilium, which may result in loss of stability of the pelvic ring.
Most anteroposterior and lateral compression injuries are considered stable disruptions because the posterior sacroiliac complex remains intact or because the bone is impacted, thus preventing further disruption. However, the magnitude of the injuring force may be great enough to cause extensive soft tissue injury, leading to further bony instability. Injuries that are generally stable are associated with fewer long-term problems and have low morbidity and mortality rates.
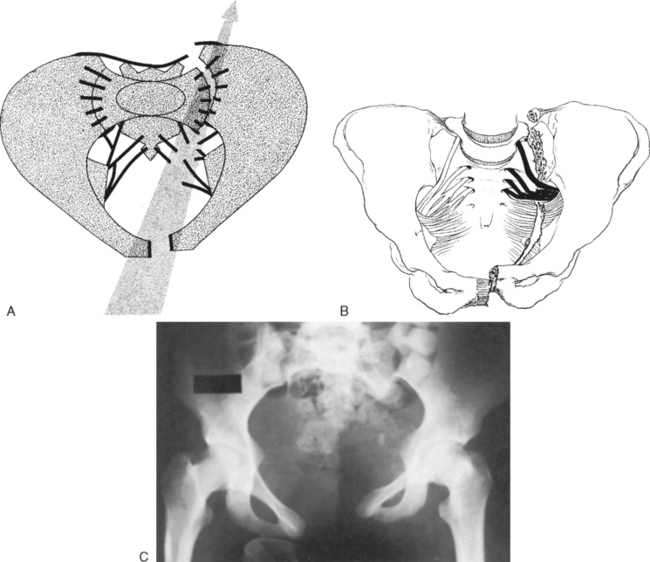
Vertical shear (Figure 27-12) is an unstable injury associated with bone and soft tissue disruption. This type of injury is usually caused by a great force, such as that from falls and crush mechanisms exerted in a vertical plane and usually shearing in nature. Fractures may be unilateral or bilateral, the latter representing the more destructive type of unstable disruption. Anterior and posterior ring disruptions and injuries to the sacrotuberous and sacrospinous ligaments are present. Anterior injuries may involve disruption of the symphysis pubis and two to four ramus injuries. Posterior lesions involve the sacrum, sacroiliac joints, or the ilium. Skin and subcutaneous tissue may be torn as well. Vertical shear disruptions are similarly unstable to anteroposterior disruptions but are associated with lower mortality rates and fewer organ system injuries.18
Pelvic ring disruptions such as widely displaced anterior posterior compression injuries should alert the admitting team to the severity of injury sustained and the need for a comprehensive team approach to resuscitation. The patient’s hemodynamic status must be continually monitored because the incidence of severe vascular injury is high with these types of fractures.19
BONE AND JOINT CONTINUITY MANAGEMENT PRINCIPLES
Early immobilization represents the first step in management of musculoskeletal injury. Immobilization helps to preserve what function currently exists and prevents further injury. By minimizing muscle spasms, proper immobilization also decreases the risk of angulation and overriding of bone ends, helping to prevent closed fractures from becoming open fractures. Application of traction in the field in conjunction with immobilization may help align bone ends in a near-anatomic position. Bone realignment often restores neurovascular and lymphatic function, which reduces further soft tissue injury and decreases pain.6
Immobilization techniques and devices applied before admission should remain in place until appropriate radiographic studies have been completed. Frequent monitoring of neurovascular status is required despite the presence of an immobilization or traction device. Compartment syndrome of the foot has been reported with use of splint-balanced immobilization devices.20 Monitoring the immobilization device is necessary to ensure proper placement and effectiveness. After radiologic evaluation, definitive immobilization modalities may be initiated.
Angulated Fractures
Realignment of a severely displaced fracture by a nonphysician depends not only on the presence or absence of vascular compromise and the amount of pain associated with realignment but, more important, on the established local emergency medical services policies governing treatment of such an injury. When realignment is not possible, the injured area is immobilized in the position in which it is found. The neurovascular status of the affected limb should be closely monitored until the limb is properly aligned and immobilized.21 In general, restoration of length and alignment before transport is preferable and less likely to lead to secondary soft tissue injury.
Extremity Fractures
Proper immobilization of a fracture includes immobilizing the joints both above and below the site of injury. Manufactured devices such as the Thomas ring splint, Hare traction splint (Figure 27-13), or Sager emergency traction device are useful for stabilizing fractures of the femur. These devices allow application of traction and immobilization of the affected area. Positioning of these devices usually requires two people, and established policies outline the specific procedure to ensure safe, rapid application. The affected extremity must be monitored for swelling, especially when traction and preformed splints are in use. Splints may require loosening of straps and padding to prevent further injury, such as compartment syndrome, which can occur when edematous tissue meets the resistance of such devices. Air splints or premolded rigid splints are useful for immobilizing feet, ankles, and upper extremities. They decrease edema by applying pressure over the injured area and simultaneously provide tamponade of open, bleeding wounds.
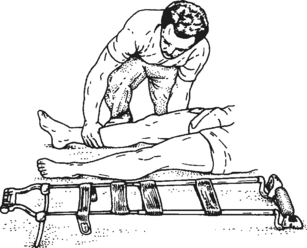
FIGURE 27-13 Hare traction splint.
(From The Maryland Way: EMT—a skills manual, Baltimore, 1985, Maryland Institute for Emergency Medical Services System [MIEMSS])
Tissue ischemia can develop if a splint remains in place for an extended time and becomes too tight, acting as a tourniquet. The length of time required to cause ischemia varies with each patient and is dependent on multiple variables. Distal pulses cannot be palpated with certain types of immobilization devices in place; therefore, visual assessments of the splinted extremity are essential. The inflatable splint should be replaced with another device as soon as possible. When an air-filled splint that has been applied outdoors in a cold environment warms with indoor temperatures, the splint tightens and may cause neurovascular deterioration. Direct pressure on an inflatable splint should result in some degree of depression, indicating that the splint is not overinflated.
Pelvic Ring Disruption
Initial evaluation of the trauma patient may not reveal obvious clinical evidence of a pelvic injury, such as extremity rotation, limb shortening, or abnormal movement on downward or inward compression of the iliac wings. However, any signs or symptoms indicative of pelvic ring disruption require patient immobilization before transport to minimize the risk of further neurovascular injury. Suspected pelvic injuries may be effectively immobilized with a pneumatic antishock garment (PASG) or pelvic binder.22 These devices provide a tamponade effect and bony immobilization. The use of the PASG is contraindicated in patients with head injuries because it can cause critical elevations in intracranial pressure (ICP). It also is contraindicated in patients who are pregnant and those with pulmonary edema, congestive heart failure, penetrating abdominal trauma, or chest injury such as tension pneumothorax or cardiac tamponade.13 Obvious pelvic injuries with associated hip dislocations or blow-out injuries to the acetabulum often require creative techniques to achieve initial immobilization and stabilization. Injuries that cause shortening, rotation, or frog-leg positioning require support and stabilization of the patient’s lower extremities in the position in which they are found. A long wooden backboard with pillows, rolled sheets, or blankets secured and taped under the patient’s knees supports extremity position and ensures immobilization during transport. The patient with an unstable pelvic ring disruption may require binder application during the early phase of resuscitation to prevent exsanguination. Use of more invasive devices such as an external fixator (Figure 27-14) or a C-clamp is rarely necessary.4 Caution is essential whenever moving a patient with a pelvic injury because disruption of the retroperitoneal tamponade can cause rapid additional blood loss.
GENERAL MANAGEMENT PRINCIPLES AND COMPLICATIONS
Hypovolemia
Any musculoskeletal injury results in blood loss. The degree of hemorrhage and its effect on the patient’s overall hemodynamic status depend on the type, location, and number of injuries. Generally, musculoskeletal injuries receive attention after stabilization of the cardiopulmonary and neurologic systems. However, there are times when musculoskeletal injuries become priorities and necessitate early, aggressive intervention. Two injuries associated with marked large-volume blood loss, traumatic amputations and massive pelvic injuries, require priority care with a coordinated team approach to facilitate restoration and maintenance of physiologic stability.8 Other bony and soft tissue injuries can usually wait for definitive care, but the patient still requires adequate volume replacement to treat hypovolemia related to blood loss.
It is difficult to estimate accurately the actual amount of blood lost, especially in patients with multiple extremity or pelvic fractures and soft tissue injuries. Table 27-4 approximates possible blood loss with open and closed fractures. Significant blood loss, as indicated in Table 27-4, can occur within an extremity even though a specific fracture has been classified as closed. The areas surrounding and distal to the fracture site become swollen, and the skin tightens from the accumulation of blood within the soft tissue. An open fracture can cause blood loss of three or more units, in addition to the amounts listed in Table 27-4. Not only does blood loss become apparent externally, but it also continues internally within the soft tissue. Hypovolemia should be anticipated in patients with these injuries, and measures to restore and maintain hemodynamics must be instituted.
TABLE 27-4 Blood Loss Caused by Fractures*
| Fracture | Blood Loss (ml) |
|---|---|
| Humerus | 500-1,500 |
| Elbow | 250-750 |
| Radius/ulna | 250-500 |
| Pelvis | 750-6,000 |
| Femur | 500-3,000 |
| Tibia/fibula | 250-2,000 |
| Ankle | 250-1,000 |
Note: One unit of whole blood equals approximately 500 ml.
* Data from Roth MS: First aid; fractures. Student BMJ 13:265-308, 2005.
Exsanguination represents the primary cause of early death after an unstable pelvic fracture.5 As previously mentioned, the pelvis receives a rich blood supply through the arteries and venous plexus of the iliac system (Figure 27-15). This vascular network can easily be injured because of its close approximation to the bony structures. The retroperitoneal space can hold large volumes of blood before spontaneous tamponade occurs, making it difficult to determine actual blood loss. Patients with pelvic injuries are also at increased risk for hemorrhage from common associated injuries, such as intra-abdominal viscera injury, which compounds the blood loss from bony and vascular injuries.23 Hypovolemic shock must be anticipated in patients with massive pelvic injuries, and early interventions to restore hemodynamic stability and tissue perfusion are required. Refer to Chapter 14 for further discussion.
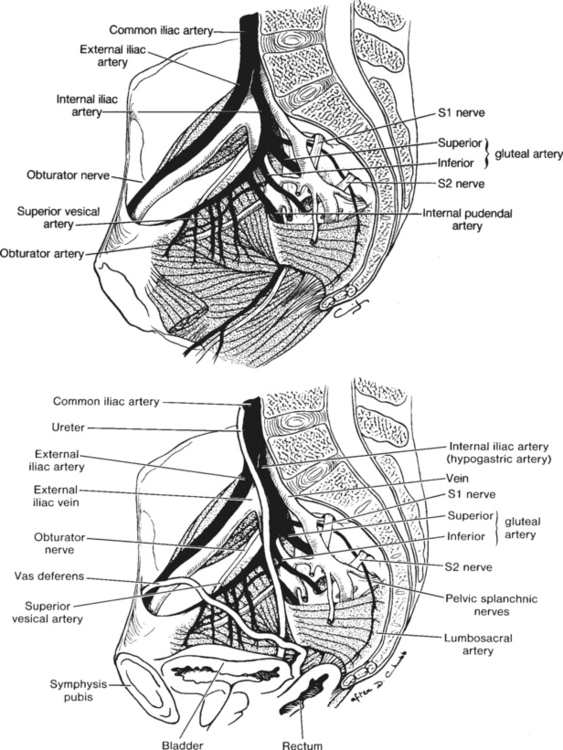
FIGURE 27-15 The internal iliac system of arteries and veins showing the position of the pelvic viscera.
(From Tile M: Fractures of the pelvis and acetabulum, Baltimore, 1984, Williams & Wilkins.)
Any patient with actual or potential intravascular volume deficits requires vigilant observation and frequent re-evaluation for the clinical indicators of shock. Patients with major musculoskeletal injuries such as traumatic amputations, multiple fractures, and unstable pelvic ring disruptions require close monitoring and should only be transported out of the resuscitation area if accompanied by qualified personnel. These patients can and do rapidly and unexpectedly deteriorate into severe hemorrhagic shock from massive blood loss. Thus constant monitoring, especially during transport, is essential. For example, the retroperitoneal hematoma associated with a massive or unstable pelvic ring injury can be disrupted during transfer of the patient to the radiography table. The sudden release of the tamponade precipitates rapid cardiovascular deterioration.24
Administration of adequate fluid by using colloids, crystalloids, or blood products is integral to successfully replete intravascular volume. Early and adequate blood transfusions help prevent deterioration and the sequelae of late shock that is a result of massive blood loss (see Chapters 13 and 14. The blood bank should be notified early and updated regarding needs.25 The team may need to consider transferring the patient to a major trauma center for this reason alone.
Obvious sources of external hemorrhage require immediate application of direct pressure and pressure dressings to obtain control. Options include a figure-eight bandage or a bandage wrapped in a spiral fashion starting at a point distal to the wound and wrapped proximally. Pressure dressings minimize damage to soft tissue and neurovascular structures while achieving hemostasis.26 Properly applied pressure dressings almost always provide adequate control of hemorrhage, even for traumatic amputations. A tourniquet is rarely appropriate and should be a last resort for massive, uncontrollable hemorrhage because it may increase the extent of the injury on amputated parts by causing ischemic damage to nerves and vessels.27
The benefits from the use of PSAGs remain controversial, specifically concerning translocation of blood.13,14,19,22,26 Their value includes immobilization and compression effects. PASGs provide external tamponade for major hemorrhage and afford stability so that resuscitation procedures can be carried out.27
Infection
All open orthopedic injuries are considered contaminated and place the patient at risk for wound infections, osteomyelitis, and, rarely, gas gangrene and tetanus.28,29 Contaminants can enter the wound in the prehospital environment or within the hospital where exposure to an antibiotic-resistant organism may occur. Wound and bone infections are potentially devastating complications associated with increased morbidity. These infections can lead to delayed union, nonunion, or acute or chronic osteomyelitis, increasing the patient’s financial burden and possibly resulting in loss of the affected extremity.30–32 Therefore, measures aimed at eliminating further wound contamination and preventing microbial growth are essential and important during early resuscitation.31–33
During resuscitation, gross contaminants are removed from the wound and exposed soft tissue and bone are covered with a wet, sterile saline solution dressing. It is important to prevent re-entry of a dirty bone end or soft tissue into the wound. Should re-entry occur, it is imperative that the orthopedic specialist be notified. Saline solution–soaked dressings are recommended rather than those saturated with iodine-based solutions.34 Soft tissue absorbs some of the solution, and iodine has been found to cause additional local tissue injury, decreasing the tissue’s resistance to infection. Additionally, iodine can interfere with fibroblast activity, which is important in stabilizing wound beds.34 Saline solution has also replaced iodine solutions during surgery and in postoperative wound management. Dressing changes should be performed as prescribed by using appropriate techniques to minimize wound contamination. Appropriate technique and attire for wound dressing changes is dependent on the risk of the procedure and the area of the hospital where the procedure is performed.
Ideally, patients with open fractures should proceed rapidly to the operating suite for wound irrigation, debridement, and definitive care. If a delay prevents this from occurring, early, aggressive wound irrigation in the emergency care area may be beneficial. The optimal method of irrigation includes use of large volumes of saline solution and low-pressure pulse lavage systems because high-pressure lavage has been shown to have a negative impact on bone and soft tissue healing.35,36
Trauma patients with multisystem and musculoskeletal injuries, especially open fractures and traumatic amputations, are at high risk for infection and therefore should receive prophylactic antibiotics during the resuscitative phase.37–40 Wound cultures before debridement are of little value. Environmental factors surrounding the incident may help direct antibiotic therapy, but the choice of single-agent gram-positive coverage or broad-spectrum coverage is largely based on surgeon preference.
Surgical prophylaxis requires adequate concentrations of the antibiotic in the area of bone or soft tissue injury or at the operative site. From the time the antibiotic is administered intravenously, it requires approximately 20 to 30 minutes or longer to achieve saturation in the interstitial fluid of a healthy bone matrix.41,42 Antibiotics are most beneficial when they are administered at the peak of bacterial wound contamination, when they satisfactorily invade the bone injury or wound, and when they are chosen specifically for the most likely contaminating organisms.42 For these reasons, administration of intravenous antibiotics begins in the resuscitative phase (or approximately 30 minutes before an elective operative orthopedic procedure) to achieve maximal antimicrobial effects.42
The use of prophylactic antibiotics in patients undergoing open reduction of closed fractures should be limited to the perioperative period. Prolonged use of prophylactic antibiotics may cause bacteria to develop antibiotic resistance. Many studies related to prophylactic antibiotic use predominantly focus on elective orthopedic surgery. In the multiple trauma patient the risk of infection increases as the number of systems involved rises.43 Studies also have shown that operative procedures lasting longer than 90 minutes have a higher incidence of infection.
Neurologic and Vascular Compromise
Any musculoskeletal injury affecting bone or soft tissue can be associated with neurologic or vascular compromise. Muscle and nerve tissues are easily damaged because of their close proximity to the bony structures. Vascular disruption decreases tissue perfusion, causing ischemia. After prolonged ischemia, reperfusion causes muscle tissue to become edematous as a result of increased capillary permeability. Edema increases pressure on the capillaries and eventually causes secondary collapse. The progression from ischemia to muscle necrosis occurs rapidly. Within 6 to 8 hours the nerves, muscles, and vascular structures may sustain irreversible damage both locally and distally.44 Understanding the mechanism of injury and the specific types of injuries that carry the highest incidence of neurovascular compromise is important.
Dislocations.
Dislocations represent orthopedic emergencies when they are associated with compromise of nearby vessels or nerves. For example, dislocations of the elbow or knee frequently require urgent intervention by an orthopedist because of the extremely high incidence of associated neurovascular disruption. The nerve injury resulting from a dislocation may be a true transaction but more frequently results from compression, blast effect, traction, or stretch mechanisms. Clinical findings indicative of a physiologic nerve injury may resolve spontaneously after the joint has been reduced and properly aligned. Symptoms may, however, remain longer depending on the severity of the injury and the length of time that elapsed before treatment. Vascular disruption may result from laceration, compression, crush, traction, or stretch mechanisms. Resolution of vascular insuffiency depends on the specific injury, the ischemic time, and the ability of collateral circulation to restore and maintain blood flow. Table 27-5 correlates joint dislocations with the potential neurovascular branches involved.
TABLE 27-5 Neurovascular Structures at Risk for Involvement in Joint Dislocation
| Joint | Nerve/Vessel |
|---|---|
| Shoulder | Brachial plexus/axillary artery |
| Elbow | Ulnar nerve/brachial artery |
| Wrist | Median nerve |
| Hip | Sciatic nerve |
| Knee | Tibial and peroneal nerves/popliteal artery and vein |
| Ankle | Tibial artery |
Fractures.
Neurovascular compromise associated with fractures results from causes similar to dislocations. Injury to the neurovascular supply of the extremities may occur from actual laceration or tearing of vessels or nerves, compression between fractured bone ends, and stretching from limb malalignment.
Pelvic Injuries.
The pelvis has a rich vascular supply, as seen in Figure 27-15. Oxygenated blood enters the pelvis through the common iliac artery. A venous plexus, consisting of valveless, thin-walled veins that allow bidirectional blood flow, drains the pelvic basin. Collateral networks exist on both the arterial and venous sides. The sciatic nerve arising from the lumbosacral plexus innervates the pelvis and the lower extremities. Any disruption of the bones or ligaments of the pelvis or hips can potentially cause severe neurovascular complications. Massive pelvic ring disruptions are considered potentially lethal injuries because of the major vascular disruption with which they are frequently associated.
Brachial Plexus Injury.
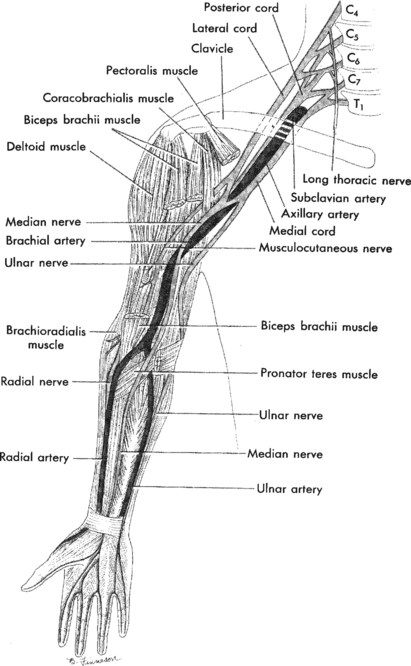
The brachial plexus, which incorporates the roots of the fifth cervical vertebra to the first thoracic vertebra, subdivides to form the axillary, musculocutaneous, median, ulnar, and radial nerves (Figure 27-16). These nerves provide motor and sensory control for the arm, elbow, forearm, wrist, and hand.
Traumatic injury to the brachial plexus may occur from blunt or penetrating mechanisms. Blunt injuries can result from excessive forces that initially injure the nearby muscle and its fascia and then cause extreme stretching of the nervous network, usually the nerve roots.45 Associated injuries that often accompany brachial plexus injuries include closed head injuries, subclavian and axillary artery and vein injuries, and shoulder dislocations.45 Frequently, blunt mechanisms that result in a plexus injury involve the patient’s ejection from a car or off a motorcycle with a landing such that the head is distracted from the affected shoulder and upper extremity.
Blunt brachial plexus injuries are subdivided into upper root and lower root classifications.46 The upper roots, C5 to C7, may sustain injury when the head has significant lateral bending away from the shoulder and when the shoulder itself is forcefully depressed downward. Upper root injuries typically affect the shoulder and elbow more than the hand. The sensory deficit usually affects the deltoid muscle, arm, and forearm. A lower root injury involving C8 to T1 may occur when the arm is forcefully extended over the head. The shoulder and elbow maintain motor function, but the forearm and hand are impaired. Any injury to the brachial plexus may be complete or incomplete. Incomplete injuries often present confusing clinical pictures because the patient has unusual patterns of sensory or motor dysfunction. A complete lesion of the brachial plexus results in paralysis and sensory loss throughout the arm and hand.46
Accurate and complete evaluation of the functional status of the brachial plexus in the critically injured multisystem trauma patient is a challenge. Often alterations in the patient’s level of consciousness and sensory responses make assessment difficult if not impossible. Differentiation of this injury from a cervical spinal cord injury and from the flaccidity seen with devastating head injuries may be difficult. The patient should be assessed for Horner’s syndrome, or Horner’s pupil, which can occur with spinal cord injuries above T1 that interrupt the cervical sympathetic chain or its central pathways, causing loss of sympathetic innervation to and constriction of the ipsilateral pupil. The affected pupil remains reactive to light and is usually accompanied by ptosis of the eyelid and possibly loss of facial sweating on the same side. If the patient has associated arm weakness, a brachial plexus injury may have occurred. More specific neuromotor checks to evaluate the nerves branching off of the brachial plexus include the following (Figure 27-17):
1. The musculocutaneous nerve is tested by evaluating the patient’s biceps function and sensation over the lateral portion of the forearm.
2. The radial nerve primarily serves a motor function assessed by evaluating the ability to extend the wrist. Evaluate sensation on the dorsal aspect of the web of skin between the thumb and index finger (Figure 27-18).
3. An intact median nerve allows apposition of the thumb to the little finger. Sensory function is evaluated by stimulating the palmar surface of the thumb and index finger and the radial half of the long finger (see Figure 27-18).
4. Motor function of the ulnar nerve is assessed by requesting the patient to abduct and adduct the fingers. Evaluate sensation on the volar surface of the small and ring fingers and the ulnar half of the long finger (see Figure 27-18).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree