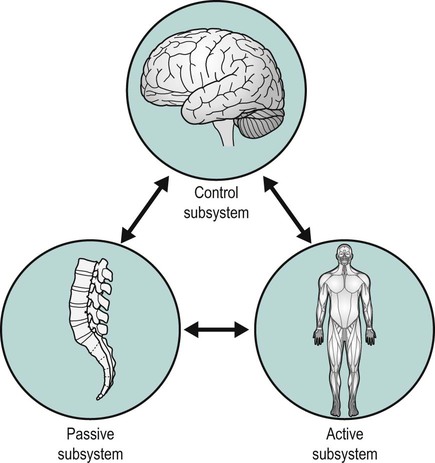
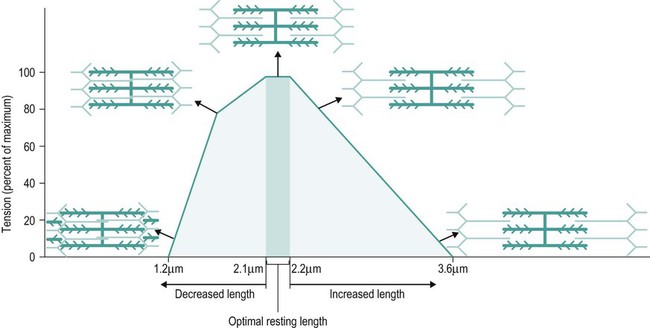
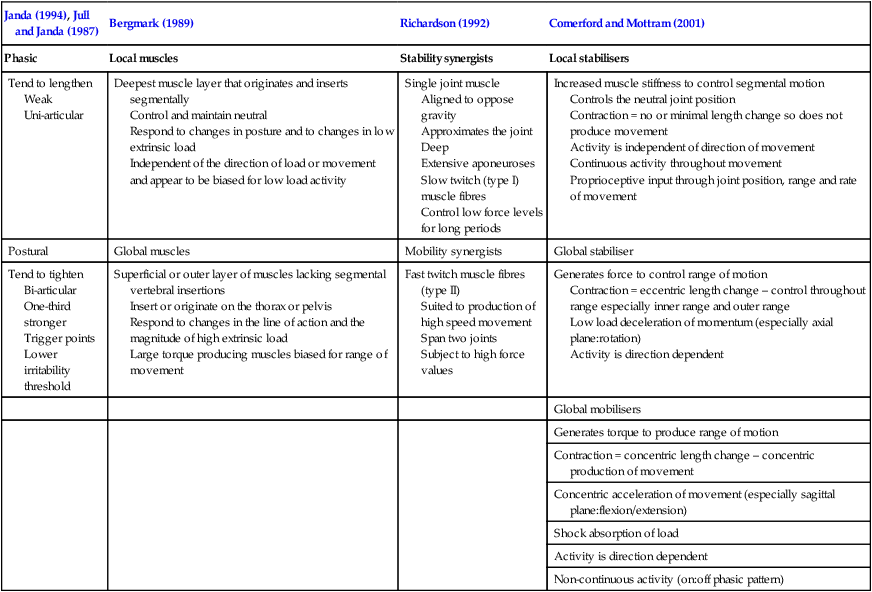
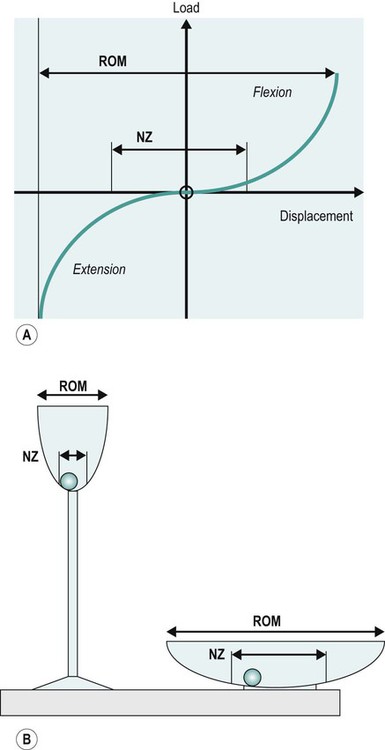
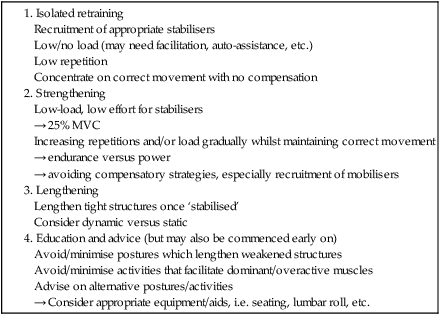
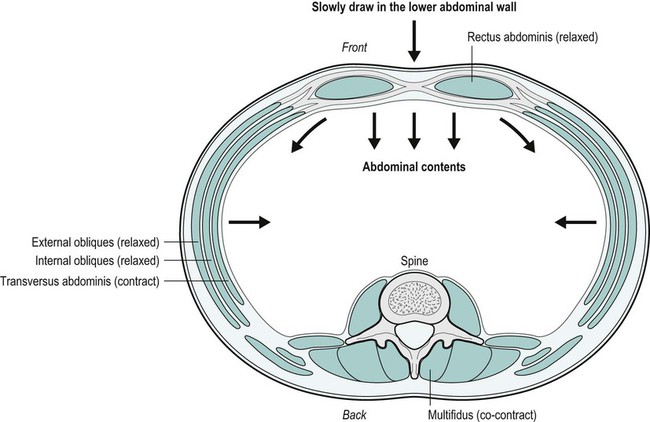
The concept of muscle imbalance (and balance) is not new. This is evidenced through over 60 years of texts involving muscle testing and function (Kendall et al. 2005) and has evolved over the most recent of those years through work from the likes of Janda (1983), Sahrmann (1987), Richardson (1992), Jull et al. (1999) and others. Clearly, alterations in muscle balance cannot be considered in isolation, but must be considered as part of movement control, where the differentiation of the factors leading to movement dysfunction is essential and part of the holistic assessment and management of individuals with musculoskeletal pain. • the micro- and macro-anatomical structure and physiology of muscle and associated tissue; • micro- and macrostructure related to function; • macro-anatomy or gross anatomy of muscles and muscle groups, along with their relationships to each other and other tissue structures, such as bones, joints, connective tissue, viscera, neural and vascular tissue; in other words, what lies deep, superficial, superior, inferior, medial and lateral to the structure being considered. In order to contain this subject within the limits of a manageable chapter, only the more commonly affected – and/or those deemed clinically important – muscle groups will be discussed, utilising select key clinical examples. However, the principles described in this chapter should be transferrable to any region in the body. In addition, when considering cause, effect and recovery, the Specific Adaptation to Imposed Demand (SAID) principle should be applied, as originally proposed by Selye (1951). Example case scenarios will be illustrated using the subjective, objective, analysis, plan and evaluation (SOAPE) process, familiar to physiotherapists from a plethora of texts and institutions (Baxter 2003). As physiotherapists, we need to be able to differentiate between what is considered a ‘normal’ (or ‘expected’) range of motion (ROM) and that which is deemed ‘abnormal’ – either hypo- or hypermobility – along with which structures may produce or restrict the range of motion. It must be noted that there may also be an underlying predisposition – or pathology – for hypo-/hypermobility, as in the case of connective tissue conditions, such as ankylosing spondylitis and hypermobility syndrome (see Figure 14.1) (as distinct from a joint demonstrating hypermobility), or neurological conditions, such as multiple sclerosis. However, it is outwith the scope of this chapter to discuss these specific pathological causes. Muscle imbalance can be either ‘passive’ or ‘active’; passive being identified by muscle length and strength being either less or more than the ideal, and active being identified when one of a synergistic pair of muscles predominates during the movement (Sahrmann 1987). The resultant functional and structural changes in the muscle appear to be reversible, suggesting that exercise to facilitate muscle length changes will be useful in the management of movement dysfunction (Gossman et al. 1982). These descriptions are all well and good, but, unfortunately, prove rather inadequate when it comes to explaining more dynamic, complex movements. Therefore, further classification of the role of muscles has been attempted by various authors according to their anatomy, architecture, fibre type and function, as summarised in Table 14.1. To simplify, some muscles exhibit a tendency to be more stabilising (i.e. multifidius in the spine) or mobilising in their function (i.e. erector spinae), although there are also some that demonstrate characteristics of both and can ‘multitask’ their role depending on the demands placed upon them at the time. Examples of the latter include the vasti muscles of the quadriceps and soleus. Throughout this chapter, muscles will be discussed in relation to their functional role as local and global stabilisers, or global mobilisers. Table 14.1 Summary of the different classifications of muscle roles Adapted from Comerford and Mottram (2001) and Norris (1995). Problems may occur when, for example, a predominantly stabilising muscle is injured or dysfunctional, leading to instability and altered joint biomechanics, increased strain on structures, such as joint surfaces, and pain. Muscles with a predominantly mobilising role can be used as temporary stabilisers, but as their anatomy and physiology does not lend themselves to this, this may lead to overuse, fatigue and pain. It has been suggested that myofascial trigger points (taut, irritable bands within muscles resulting from overuse) may develop as a result (Simons et al. 1999; Fernández-de-las-Peñas et al. 2006) and which can perpetuate the muscle imbalance through further pain and resultant inhibition. Additionally, the term ‘stability’, particularly ‘core stability’, has also become synonymous with approaches to dealing with muscle imbalance of the spine, especially in the lumbar spine. Confusion can arise with this term, particularly when used very specifically by one group of professionals to be more than merely a descriptive state; when is someone or something stable or unstable, what makes someone or something stable/unstable? For example, an orthopaedic surgeon may well be focussing on the bony congruency or ligamentous support at a spinal segment and any trauma or pathology associated with this (as in spondylolithesis) as the cause of instability. Conversely, a physiotherapist, unless assessment suggests otherwise, may be concerned with the quality of the spinal movement, any associated/compensatory movements and the support of the muscles to stabilise the movement. Therefore, the stability of the spine, in this example, is dependent on a number of factors. Figure 14.2 demonstrates a basic model of stability that considers the interplay of the principal systems involved (Panjabi 1992a, 1992b, 2003). Panjabi (1992a, 1992b, 2003) additionally discusses control of the neutral zone: the area (or zone) around the segment’s neutral position where there is little resistance offered by the passive restraints in response to a small range of displacement (see Figure 14.3). Although originally related to the spine, this model can be applied equally to the appendicular, as well as the axial skeleton, when considering the interplay of the subsystems. This control of the neutral zone can be disturbed locally by the dysfunction of recruitment and motor control of the deep segmental stabilisers, and globally by an imbalance between the mono-articular stabilising muscles and the bi-articular mobilising muscles (Comerford and Mottram 2001). It is hypothesised that an increase in the size of the neutral zone (therefore decreased ‘stability’ or increased ‘instability’, if you like) correlates with pain and dysfunction (and possibly could be caused by either); correspondingly, decreasing the neutral zone may decrease pain and dysfunction (Panjabi 2003). However, it must be noted that the clinical reality is rarely this straightforward and is usually multifactorial (see Chapter 17)! Stabilisation requires automatic recruitment of the muscles surrounding the joint. This requires appropriate co-activation of muscles, the application of appropriate levels of force for the task in hand and appropriate timing of the muscles (Richardson 1992). Normally, the mono-articular stabilisers should activate earlier than the multi-articular mobiliser synergists – a feed-forward mechanism. This co-ordinated activity involves sensory strategies through feedback from the joint and ligament afferents, and muscle spindle activity, along with biomechanical, motor processing strategies and learned behaviour that anticipates change (Comerford and Mottram 2001). Motor units (the motor neurone and the muscle fibres it innervates) contain the same type of fibre so that there are, pragmatically, two main types: slow (tonic, type I fibres) motor units and fast (phasic, type II fibres) motor units. Therefore, slow motor units have a slow speed of contraction, low contraction force and are fatigue resistant compared with fast motor units. Slow motor units are recruited primarily at low loads of less than 25% of maximum voluntary contraction (MVC) and fast motor units are recruited at higher loads (Gibbons and Comerford 2001). Therefore, the recruitment of slow motor units, and use of muscles with high proportions of these is necessary for optimal stabilisation. When mobiliser muscles, which contain high proportions of fast motor units are utilised as compensation for stabiliser dysfunction, degradation of the fine control results along with fatigue and potentially pain and spasm if then over-used. However, biased recruitment of shortened muscles can be a problem. It is suggested that short muscles are recruited more easily than their lengthened synergists (Sahrmann 1987). This may be owing, mechanically, to the increased overlap of actin and myosin (as in the sliding filament theory, below) leading to an increase in the intrinsic ‘stiffness’ of the muscle and readiness for activation, and owing, neurologically, to the increased excitability of the alpha motor neurone pool facilitated by the increased tension and activity of the muscle spindle afferents (Comerford and Mottram 2001). There is evidence to suggest that the reduction of proprioceptive input during sustained low-load contractions from the muscle spindle changes the recruitment order of the motor neurones and the normal dominance of the local stabilisers (Grimby and Hannerz 1976, cited in Comerford and Mottram 2001). Janda (as discussed by Comerford and Mottram (2001)), identified and quantified recruitment and sequencing differences between synergistic muscle groups in functional movement. From this, he was able to identify a consistent recruitment pattern in asymptomatic individuals and also characteristic abnormal patterns in symptomatic individuals. Similar evidence has been identified by several authors in relation to individuals with impingement symptoms of the shoulder (Ludewig and Cook 2000; Cools et al. 2003), cervicogenic headaches (Jull et al. 1999) or patellofemoral pain (McConnell 1996). It is suggested that stretch weakness occurs when a muscle is maintained in an elongated position beyond its neutral physiological rest position but not beyond the normal range of muscle length (Gossman et al. 1982). Examples of this may be weakness of the dorsiflexors in a bedridden patient when held in a lengthened position owing to the weight of the bed clothes holding the foot in a plantar flexed position. Equally, prolonged postural strain, such as drooping shoulders with elongation of the middle and lower trapezii, can lead to stretch weakness. When a muscle is immobilised in a lengthened or shortened position, the muscle adapts in order to either increase or decrease the number of sarcomeres respectively. This change in number allows for a change in sarcomere length to one that gives maximum overlap of actin and myosin for optimum cross bridge formation and the ability of the muscle to achieve maximum tension in the immobilised position (Williams and Goldspink 1978). These adaptations appear to differ with age, occurring primarily in the tendon in young people rather than muscle (Gossman et al. 1982), such that immobilisation in a lengthened position leads to elongated tendon and shorter muscle belly with a reduction in the number of sarcomeres in the muscle belly. Williams and Goldspink (1984) also demonstrated changes in the connective tissue of the muscle when a muscle was immobilised in a shortened position. It is generally thought that muscle has a parallel elastic component (primarily from the perimyseum, but also the epimyseum) to the active contractile element. This parallel elastic component is thought to distribute forces associated with the passive stretch of the muscle and maintain the relative position of the fibres. In a muscle immobilised in a shortened position the increase in connective tissue is likely to result in an increase in muscle stiffness and reduced elasticity of the muscle. Similar changes may occur when a muscle works at a shorter length (Williams and Goldspink 1984) and it should be noted that normal, transient changes in muscle length, as part of movement and positioning, will affect the tension that can be developed, as demonstrated by the sliding filament theory and the muscle length tension curve (Figure 14.4). ‘Relative stiffness’ as described by White and Sahrmann (1994) in one segment will require flexibility in an adjacent area to gain functional movement. This relative stiffness can occur as discussed above in a shortened muscle, but also when the passive structures around the joint (capsule and ligament) or the joint surfaces themselves become restricted in their movement. An example of this might be an adhesive capsulitis of the glenohumeral joint; restriction of the capsule around the joint causes limitation of abduction resulting in hypermobility of the scapulo-thoracic joint to gain movement and hence lengthening of the stabilising muscles of the scapula on the chest wall. Similarly, ‘relative flexibility’ (White and Sahrmann 1994) can occur where mono-articular muscles are unable to adequately shorten, so are lengthened, strained or weak and allow excessive motion at the joint they act upon. This increase in mobility has obvious implications on initiating pathology. This relative stiffness and flexibility gives rise to the concept of ‘give and restriction’, as discussed by Comerford and Mottram (2001). The examination and assessment process is required to determine whether muscle imbalance is a causal factor of the patient’s symptoms. Recognition of postures that deviate from the expected normal (see Kendall et al. 2005) and of physiological movement dysfunction patterns (as detailed in Table 14.2) is essential to this. Table 14.2 The physiological parameters already discussed should inform your treatment decisions. Table 14.3 provides an overview of management principles. Table 14.3 Overview of management principles The lumbo-pelvic region has seen a significant amount of research and debate as to the role of the muscles in relation to lower back pain, which should not be surprising considering how common lower back pain is. However, it remains a complicated area and so it is beyond the scope of this chapter to consider all muscles and potential permutations of imbalance. As transversus abdominis (TrA) has received considerable interest both in the literature and clinical environment, this will be the focus as a template approach for the physiotherapist to consider in practice. Table 14.4 lists the main muscles acting on the lumbo-pelvis with their respective primary functional role. Table 14.4 The main lumbo-pelvic mobiliser and stabiliser muscles The concept of ‘core stability’ and muscular stabilisation of the lumbar spine has derived from Panjabi’s (1992a, 1992b, 2003) model of the three subsystems described previously. With reference to the passive subsystem, the lumbar spine appears to be at a disadvantage, ‘sandwiched’ between the inherently more stable thoracic spine (via the rib cage) and pelvis (see Figure 14.5). Therefore, whilst the lumbar vertebrae and intervertebral discs are the largest and strongest in the spine, further support and control is required, but, as you will see in Figure 14.5, TrA, along with the multifidus, diaphragm and pelvic floor, appear to form a ‘box’ (or more aptly, a corset). The diaphragm and pelvic floor appear to contribute mainly through increasing intra-abdominal pressure and restricting the movement of the viscera (Richardson et al. 2004). TrA is the deepest of the abdominal muscles (Figure 14.6). The direction of the muscle fibres runs horizontally medially from the lateral attachments of the internal surface of the six lowest ribs, the thoracolumbar fascia, internal surface of the iliac crest and the lateral third of the inguinal ligament to the sheath of rectus abdominis (Ombregt et al. 2003; Standring 2005). It can be seen from the attachments how contraction can mechanically increase intra-abdominal pressure and thus stabilise the lumbar spine, although it does not act alone, as co-contraction with multifidus is also thought to occur (Richardson et al. 2002, 2004). When considering this action, it is easy to understand how dysfunction may lead to pathological signs and symptoms, and subjects with low back pain have been shown to demonstrate delay and inhibition of contraction compared with asymptomatic subjects (Richardson et al. 2002, 2004). It is widely accepted that TrA provides support for the abdominal contents and it has been demonstrated through research that it provides indirect stability for the lumbosacral spine and sacroiliac joints (Richardson et al. 2002, 2004). The associated levers of the pelvis and spine arising from these joints must be remembered together, with further consideration when relating TrA structure to its function and the stabilising of the pelvic postero-anterior lever in neutral; in other words, maintaining an antero-posteriorly neutral pelvic level. Mechanically, transversus abdominis may have a direct role in maintaining pelvic neutral, producing a cephalic force on the anterior pelvis owing to the lower fibres of the muscle curving inferiorly and medially to attach to the pubic crest and pectineal line, along with the aponeurosis of internal oblique (Standring 2005). Further to this, if, on contraction, it places tension on the rectus abdominis, which in turn attaches to the costal cartilages and ribs superiorly and pubis inferiorly, it can be mechanically argued that transversus abdominis has an indirect role in stabilising and maintaining the pelvis in neutral relative to the spine. This, therefore, helps prevent anterior tilt of the pelvis. An anterior tilted pelvis can therefore present as a sign of transversus abdominis weakness and, from clinical experience, has been supported or accompanied by poor palpable contraction of the muscle. The same anterior tilted pelvis may be the causal link for increasing the lumbar lordosis and therefore be a source for causing mechanical back pain, for example through increased facet joint irritation from the resultant increased compression force production. It is not only weakness that can lead to an anterior tilted pelvis. The lower fibres of TrA and all the fibres of rectus abdominis may adaptively lengthen over time, such as during pregnancy in women, for example. Also, through prolonged, repeated and sustained static posture in sitting there can be an over-compensatory posture with an anterior tilted pelvis and hyper-lordosis of the lumbar spine in an attempt to maintain a normal lumbar lordosis. This would be considered to be the adverse effects of the SAID principle (Selye 1951). In other words, unwanted adaptation to adverse imposed demand, such as lengthening of the abdominal muscle fibres and the anterior longitudinal ligament of the spine. Before considering further theory and research, the physiotherapist must also understand that it has also been argued in the literature (Richardson et al. 2002, 2004) that TrA can become non-functional as an inhibitory response to problems, such as mechanical low back pain. It is considered here that this may not be the order of events in all mechanical low back pain and it is difficult to research the order of events, as it would be necessary to have otherwise healthy subjects induce mechanical low back pain in order to determine if this is the point TrA switches off. Nevertheless, the physiotherapist can only treat what presents and in the presence of a non-functioning TrA the challenge is to rehabilitate the muscle. As described above, the SOAPE process will be used for further illustration. Symptomology may occur in secondary areas both proximally and distally affecting the thoracic and cervical spine and upper and lower quadrants owing to the altered alignment of the lumbar spine posture and its knock-on effect on posture elsewhere. Signs and symptoms will need to be addressed but, equally, the other causations of an anteriorly tilted pelvis or associated and secondary lumbo-pelvic-hip complex problems would need investigating and correcting as necessary (see some examples in the non-exhaustive list in Table 14.5). Table 14.5
Muscle imbalance
Introduction
What is muscle imbalance?


Janda (1994), Jull and Janda (1987)
Bergmark (1989)
Richardson (1992)
Comerford and Mottram (2001)
Phasic
Local muscles
Stability synergists
Local stabilisers
Tend to lengthen
Weak
Uni-articular
Deepest muscle layer that originates and inserts segmentally
Control and maintain neutral
Respond to changes in posture and to changes in low extrinsic load
Independent of the direction of load or movement and appear to be biased for low load activity
Single joint muscle
Aligned to oppose gravity
Approximates the joint
Deep
Extensive aponeuroses
Slow twitch (type I) muscle fibres
Control low force levels for long periods
Increased muscle stiffness to control segmental motion
Controls the neutral joint position
Contraction = no or minimal length change so does not produce movement
Activity is independent of direction of movement
Continuous activity throughout movement
Proprioceptive input through joint position, range and rate of movement
Postural
Global muscles
Mobility synergists
Global stabiliser
Tend to tighten
Bi-articular
One-third stronger
Trigger points
Lower irritability threshold
Superficial or outer layer of muscles lacking segmental vertebral insertions
Insert or originate on the thorax or pelvis
Respond to changes in the line of action and the magnitude of high extrinsic load
Large torque producing muscles biased for range of movement
Fast twitch muscle fibres (type II)
Suited to production of high speed movement
Span two joints
Subject to high force values
Generates force to control range of motion
Contraction = eccentric length change – control throughout range especially inner range and outer range
Low load deceleration of momentum (especially axial plane:rotation)
Activity is direction dependent
Global mobilisers
Generates torque to produce range of motion
Contraction = concentric length change – concentric production of movement
Concentric acceleration of movement (especially sagittal plane:flexion/extension)
Shock absorption of load
Activity is direction dependent
Non-continuous activity (on:off phasic pattern)
Stability
Neurophysiological components of muscle balance
Motor control
Stretch weakness
Positional weakness and length associated changes
Relative flexibility and relative stiffness
Examination and assessment principles
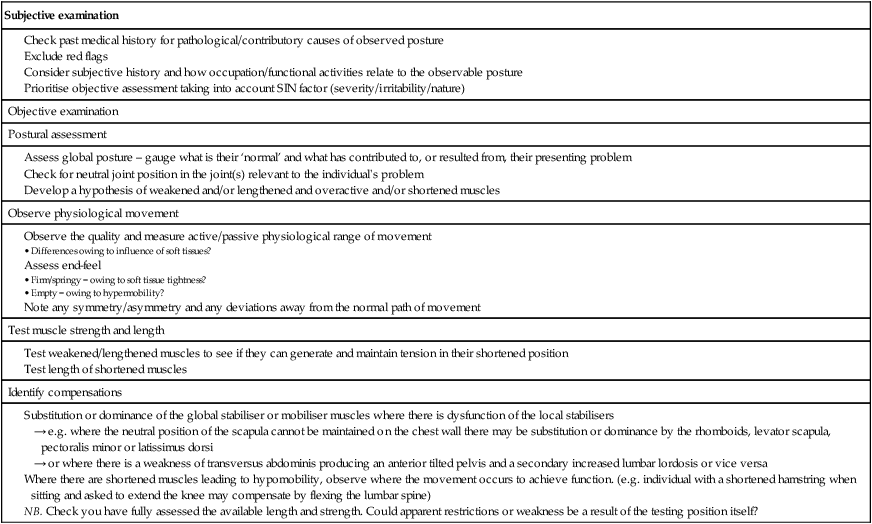
Treatment, intervention and management principles
The Lumbo-pelvic region
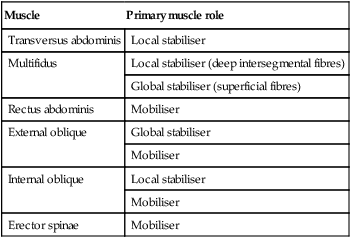
Muscle
Primary muscle role
Transversus abdominis
Local stabiliser
Multifidus
Local stabiliser (deep intersegmental fibres)
Global stabiliser (superficial fibres)
Rectus abdominis
Mobiliser
External oblique
Global stabiliser
Mobiliser
Internal oblique
Local stabiliser
Mobiliser
Erector spinae
Mobiliser

Transversus abdominis (TrA)
Subjective examination
Muscle
Problem
Additional associated/secondary problems
Iliopsoas
Too short/passive insufficiency causing anterior tilted pelvis
Increased lumbar lordosis and lumbar spinal dysfunctional restriction of lumbar flexion range of movement (ROM)
Hip lateral rotational dysfunctional restriction of ROM, and shortening of internal rotators and adductors of the hip
Hip extension dysfunctional restriction of ROM
Shortening of other hip flexor, rectus femoris
Shortening of other muscles of quadriceps femoris
Medial knee joint stresses
Quadratus lumborum
Too short/passive insufficiency causing an increased lumbar lordosis and an anterior tilted pelvis
All of the above
Plus, unilateral imbalance may cause rotation/torsion or lateral pelvic tilt
Multifidus
Weakness/lengthening or over-activity/shortening
Although acknowledged as segmental stabilisers, collectively they can contribute to the maintenance of abnormal posture if dysfunctional, such as hyperlordosis and therefore predispose to anterior tilt
NB: It should also be noted that muscles involving the lower limb, which also act on the pelvis need consideration, such as rectus femoris and the hamstrings (see Kendall et al. (2005) and others regarding postures such as the pelvic-crossed syndrome). ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Muscle imbalance