Mortality After Total Hip Arthroplasty
Wadih Y. Matar, Armin Aalami Harandi and Javad Parvizi
Key Points
• Most deaths are related to cardiorespiratory complications.
• Advanced age, revision surgery, and comorbidities have been associated with increased death rates.
• Most reported intraoperative deaths are related to cemented THA.
Introduction
Although total hip arthroplasty (THA) is generally considered to be a safe and effective procedure, it can be associated with a number of complications. Perioperative mortality is the most devastating and feared of these complications.1–5 Most of these deaths occur during the early postoperative period and most are the result of cardiorespiratory complications such as myocardial infarction and pulmonary embolism. Intraoperative death can also occur and represents the most dramatic event facing the adult reconstructive hip surgeon.6 Cementing during THA has traditionally been considered to be the main factor associated with intraoperative death.6–8 However, with more contemporary cementing techniques, the incidence of cement-related intraoperative deaths has decreased drastically.9,10
Mortality Rates
In the United States, rates of primary and revision THA are projected to increase significantly over the coming decades.11,12 Improvements in surgical and anesthesia techniques, including better perioperative monitoring and postoperative protocols, allow the arthroplasty surgeon to offer THA to the older patient, who is at higher risk for perioperative complications.13 Theoretically, this could lead to a higher mortality rate if not offset by the expected concomitant increase in demand for THA in the younger, healthier patient population.14,15
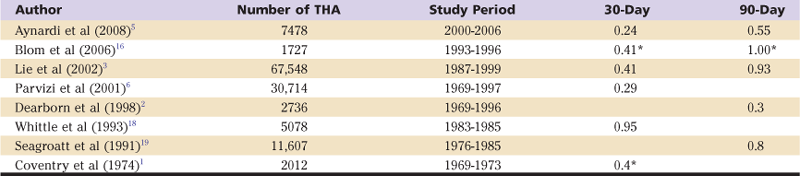
Most studies show that the immediate postoperative period represents the highest risk of death following THA.1–3,5,16–19 Studies looking at 30-day mortality report rates between 0.24% and 0.95%. Studies looking at 90-day mortality report rates between 0.3% and 1.0% (Table 25-1).
Table 25-1
Sample Studies of Early Mortality After Total Hip Arthroplasty
Over the long term, the survival rates of patients who have undergone THA are generally better than those reported for the general population, suggesting a possible beneficial effect of the procedure in prolonging patients’ lives.5,18,20-22 Barrett and associates investigated whether improved survival was directly attributable to THA, or whether it was due to other factors.23 By studying 28,469 primary THA Medicare patients over a 6-year period and matching them 5 : 1 to a control group, the authors used proportional hazards regression analysis for three postoperative periods. THA patients had a higher mortality rate in the immediate postoperative period; however, by 3 months, THA patients had a lower mortality rate than matched controls. From 3 months to 5 years, the mortality rate of THA patients was only two-thirds that of the control group after adjustments were made for sex, age, Medicaid eligibility, and other comorbidities. Beyond 5 years, mortality rates started to converge.
In a more recent study, Aynardi and colleagues reported on the mortality rate following 7478 consecutive elective primary and revision THAs between 2000 and 2006.5 The overall reported mortality rate at 30 days was 0.24% (18 of 7478), with the vast majority of deaths occurring in the hospital (13 of 18). The 90-day mortality rate was 0.55% (41 of 7478). The authors noted that death rates increased with increasing age in this patient cohort. Patients younger than 65 years undergoing primary THA had the lowest death rate (0.03%), and patients older than 85 years had the highest death rate (4.91%). These findings have been corroborated by other authors.2,5,18 After studying mortality rates in elective THA in nonfracture patients, Whittle and coworkers showed an 11-fold increase in the mortality rates of older patients (age 85 years or older) when compared with a group of patients between the ages of 66 and 69 years.18
In addition to age at the time of surgery, the type of surgery performed seems to have an impact on perioperative mortality. Aynardi and coworkers reported higher mortality rates following revision THA compared with primary THA (1.24% vs. 0.41%).5 In fact, patients older than 85 years undergoing revision THA had the highest death rate among all groups at 6.25%. Using 2003 nationwide U.S. data, Zhan and associates reported on death rates among 200,000 primary THAs and 36,000 revision THAs.24 The in-hospital death rate was 0.33% for primary and 0.84% for revision THA. The authors associated advanced age and comorbidities with worse outcomes.
Simultaneous bilateral THA has been associated with increased perioperative complications, prompting the arthroplasty surgeon to reserve this procedure for a select group of young and healthy patients. Tsiridis and associates performed a meta-analysis of all studies that compared the results of THA in unilateral and simultaneous bilateral THA and reported no statistically significant difference in the rate of pulmonary embolism, deep venous thromboembolism (DVT), or instability between the two groups.25 Simultaneous bilateral THA had a shorter overall hospital stay when compared with staged unilateral THA, but the bilateral group required more blood transfusions. The reported mortality rate following simultaneous bilateral THA appears to be as low as that reported for unilateral THA.26,27 However, the selection bias of younger patients without major comorbidities poses a challenge in extrapolating these results.26
Causes of Death Following Total Hip Arthroplasty
Causes of mortality following THA can be separated into those that occur intraoperatively and those that occur postoperatively.*
Intraoperative Mortality
Sudden intraoperative death is the most feared complication of THA. The occurrence of this phenomenon has greatly diminished over time with advancements in anesthesia techniques, cementing techniques, and the use of uncemented femoral stems.5,6,9,10,31 Parvizi and colleagues reported 23 intraoperative deaths in a series of more than 29,000 patients undergoing hip arthroplasty.6 All deaths occurred in cemented arthroplasties. Although approximately half of these cases occurred in elderly hip fracture patients with preexisting cardiovascular disease undergoing hemiarthroplasty, the other half of these cases occurred in the setting of elective THA. The authors identified irreversible cardiorespiratory disturbance during cementing as the cause of death in all patients. Microemboli were identified in the lungs of 11 of 13 patients during autopsy. Notably, no intraoperative deaths were reported in more than 15,000 patients undergoing uncemented arthroplasties performed in the same time period, suggesting that cementing is a major risk factor for sudden intraoperative death during THA.
Several causes of intraoperative mortality during cementation have been proposed. These include bone marrow and fat emboli,9,32 polymethylmethacrylate (PMMA)-induced myocardial depression,33 vasodilatation secondary to PMMA,34,35 autonomic reflexation effects,36 thromboplastin generation,37 and prostaglandin-induced vasodilatation.38 The term bone cement implantation syndrome, which can encompass varying degrees of systemic hypotension, pulmonary hypertension, cardiogenic shock, hypoxemia, cardiac arrhythmias, and even cardiac arrest, has been used to describe events that can occur within minutes of cementing of prosthetic components.6,10,32,39 Embolization of fat and marrow contents during THA can be detected and quantified using transesophageal echocardiography.9 Even though embolization of marrow occurs with impaction of uncemented components, emboli following cementation can be greater in number, size, and duration, probably because of the higher intramedullary pressures produced by cementing the stem.32,39,40
Postoperative Mortality
Many studies have investigated the causes of postoperative death following THA.* As noted previously, age has been shown to be a significant risk factor, as perioperative mortality rates increase with increasing age.2,5,18 Conditions afflicting the cardiovascular system such as acute coronary syndrome, cardiopulmonary arrest, stroke, arrhythmia, and pulmonary embolism are the leading causes of mortality following THA.5,16,26,30 Respiratory conditions, sepsis, and malignancy are the other common conditions that may be responsible for early postoperative mortality.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







