Modular Stems
David A. Mattingly
INDICATIONS
While useful in most hips requiring primary total hip arthroplasty (THA), modular femoral stems are especially indicated in conditions with abnormal acetabular and/or femoral anatomy (1). Elements of developmental dysplasia of the hip (DDH) and deformity occur frequently in primary THA (2,3,4,5,6,7). A review of 75 hips with a diagnosis of idiopathic osteoarthritis revealed proximal femoral deformity in 40% of hips and acetabular dysplasia in 39% of hips (5). The variable shape of the femoral canal (canal/flare index; proximal/distal mismatch) may cause difficulty in achieving proximal and distal fit and fill with standard femoral components (8).
Other frequent conditions producing distorted anatomy include prior surgery (e.g., osteotomy), posttraumatic deformity, secondary osteoarthritis (e.g., Legg-Calve-Perthes disease, slipped capital femoral epiphysis, and sepsis), as well as coxa vara and coxa valga deformities. Less common conditions include small femoral canals (e.g., juvenile rheumatoid arthritis, dwarfism, spondylope-ripheral dysplasia), large femoral canals (Dorr Type C bone (9), ankylosing spondylitis, rheumatoid arthritis, and alcoholic bone disease), and Paget disease.
CONTRAINDICATIONS
Contraindications to the modular femoral stems are rare but might include extreme femoral canal deformity where cemented or custom stem fixation is more easily achieved. The direct anterior approach is contraindicated when using a modular femoral stem.
PREOPERATIVE PLANNING
Detailed history, physical, and radiographic evaluation are required for any patient undergoing primary THA. The history should focus on prior treatments, surgeries, and complications. The patients’ disabilities (leg length, fatigue, limp, etc.) and pain pattern should be thoroughly discussed.
Physical examination will often reveal abnormalities in size, range of motion (stiffness or laxity), leg lengths, and prior incisions, which can make surgery more difficult. Surgeries to the contralateral limb (e.g., epiphysiodesis) should be noted. Leg lengths are assessed by tape measure and blocks under the short limb to determine exact discrepancies and what length appears to best balance the pelvis. Thorough preoperative assessment of femoral and sciatic nerve function is essential.
Plain radiographs should include an anteroposterior (AP) projection pelvis and AP and Lauenstein lateral x-rays of the involved hip. Radiographic magnification markers taped to the involved hip allow for an accurate estimate of x-ray magnification, permitting precise femoral canal sizing and templating. Computer tomography (CT) scans are rarely indicated but can provide more accurate assessment of anteversion, femoral canal dimensions, and acetabular bone stock assessment. Scanograms may be useful to more accurately assess limb length inequalities.
TECHNIQUE
The patient is positioned in the lateral decubitus position with the affected side up. The underlying leg is paced in flexion to reduce the degree of lumbar lordosis. The trunk and pelvis are appropriately stabilized while the operated leg is prepped. We drape the operated leg free over a radiolucent table to permit possible fluoroscopic evaluation.
Anterolateral, direct lateral, and posterior approaches may be used with modular stems. I prefer the posterior approach to avoid scars from prior anterior surgeries (common in DDH), minimize damage to the abductors, and easily identify, protect, and monitor the sciatic nerve. The posterior approach can be easily converted to a trochanteric or subtrochanteric osteotomy for a stiff hip, distorted anatomy, or high-riding DDH cases (see Fig. 18-1).
For thin, flexible hips requiring less than 1-cm limb lengthening, a small incision is made from the midpoint of the vastus tubercle extending proximally and posteriorly for 4 to 6 inches (see Fig. 18-2). The incision is extended further proximally and distally for larger and stiff patients, especially those requiring trochanteric or subtrochanteric osteotomy or limb lengthening greater than
1 cm. The fascia lata and gluteus maximus are divided in line with the incision. The sciatic nerve is identified by palpation but not dissected. Partial or full release of the gluteus maximus tendon at the linea aspera may be performed to prevent tethering of the sciatic nerve during manipulation of stiff hips or lengthening of greater than 1 cm. The piriformis tendon is released from its fossa to expose the inferior capsular recess. Other external rotators are released as needed and reflected posteriorly to further protect the sciatic nerve, which may be scarred or displaced in cases with distorted anatomy. Cobra retractors are then placed superiorly under the gluteus minimus muscle and in the inferior capsular recess. While posterior capsulotomy and repair are performed in most cases, including Crowe I and II DDH hips (see Fig. 18-3), capsulectomy may need to be performed in selected stiff hips, especially those requiring further exposure or significant limb lengthening (e.g., Crowe III and IV DDH hips). A smooth 7/16-inch Steinman pin can be placed into ischium at the level of the transverse ligament for limb length assessment prior to dislocation and after trial reduction.
1 cm. The fascia lata and gluteus maximus are divided in line with the incision. The sciatic nerve is identified by palpation but not dissected. Partial or full release of the gluteus maximus tendon at the linea aspera may be performed to prevent tethering of the sciatic nerve during manipulation of stiff hips or lengthening of greater than 1 cm. The piriformis tendon is released from its fossa to expose the inferior capsular recess. Other external rotators are released as needed and reflected posteriorly to further protect the sciatic nerve, which may be scarred or displaced in cases with distorted anatomy. Cobra retractors are then placed superiorly under the gluteus minimus muscle and in the inferior capsular recess. While posterior capsulotomy and repair are performed in most cases, including Crowe I and II DDH hips (see Fig. 18-3), capsulectomy may need to be performed in selected stiff hips, especially those requiring further exposure or significant limb lengthening (e.g., Crowe III and IV DDH hips). A smooth 7/16-inch Steinman pin can be placed into ischium at the level of the transverse ligament for limb length assessment prior to dislocation and after trial reduction.
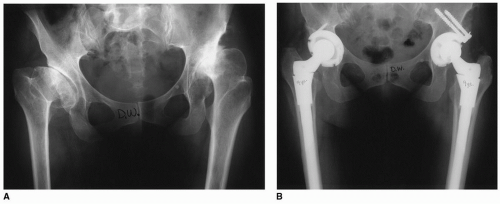
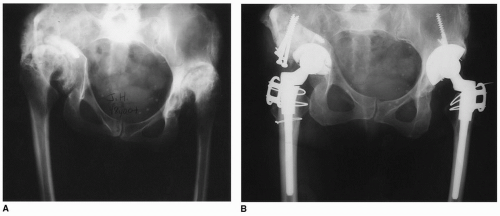 FIGURE 18-1 Preoperative (A) and postoperative (B) AP pelvis x-ray demonstrating transtrochanteric approach required for marked stiffness from prior bilateral iliac osteotomies. |
The hip is dislocated posteriorly if not already severely subluxed or dislocated (Crowe III and IV hips) (3). The greater and lesser trochanters and femoral head are used as landmarks in conjunction with preoperative templates to determine the level of femoral neck osteotomy (see Fig. 18-4). When subtrochanteric osteotomy (12) is performed to help reduce high-riding Crowe III and IV hips, the femoral canal is prepared distally and proximally and a trial sleeve is positioned in the proximal
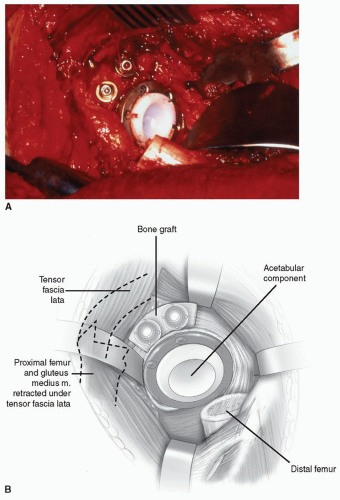
femur (see Fig. 18-5). The vastus lateralis is then reflected from the vastus tubercle distally for 6 to 10 cm. The linear aspera is identified, and rotation marks are made on the femur prior to the osteotomy. The iliopsoas tendon is sectioned just proximal to its insertion at the lesser trochanter. The transverse osteotomy is then made distal to the sleeve and approximately 3.5 cm distal to the lesser trochanter (see Fig. 18-6). The acetabulum is then easily exposed by complete capsulectomy
and anterior displacement of the proximal femoral fragment and attached abductors (see Fig. 18-7). If subtrochanteric osteotomy is not performed, then the capsule is dissected inferiorly until the transverse ligament and true socket are identified. The acetabulum is then prepared and positioned. Acetabular bone deficiencies may require cup placement more medial, superior, or in more abnormal version than desired in cases with distorted anatomy. The advantage of the modular stem in this setting is that it can easily accommodate to these abnormal socket positions by increasing offset, neck length, or independent version of the stem from the sleeve to maximize myofascial tension, leg length, and stability, while avoiding implant impingement.
femur (see Fig. 18-5). The vastus lateralis is then reflected from the vastus tubercle distally for 6 to 10 cm. The linear aspera is identified, and rotation marks are made on the femur prior to the osteotomy. The iliopsoas tendon is sectioned just proximal to its insertion at the lesser trochanter. The transverse osteotomy is then made distal to the sleeve and approximately 3.5 cm distal to the lesser trochanter (see Fig. 18-6). The acetabulum is then easily exposed by complete capsulectomy
and anterior displacement of the proximal femoral fragment and attached abductors (see Fig. 18-7). If subtrochanteric osteotomy is not performed, then the capsule is dissected inferiorly until the transverse ligament and true socket are identified. The acetabulum is then prepared and positioned. Acetabular bone deficiencies may require cup placement more medial, superior, or in more abnormal version than desired in cases with distorted anatomy. The advantage of the modular stem in this setting is that it can easily accommodate to these abnormal socket positions by increasing offset, neck length, or independent version of the stem from the sleeve to maximize myofascial tension, leg length, and stability, while avoiding implant impingement.
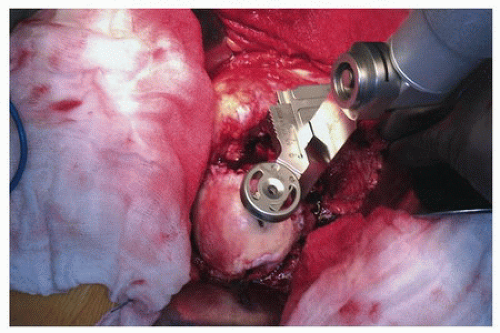 FIGURE 18-4 A femoral neck resection template for stem size, neck length, and offset determines the level of initial femoral neck osteotomy. |
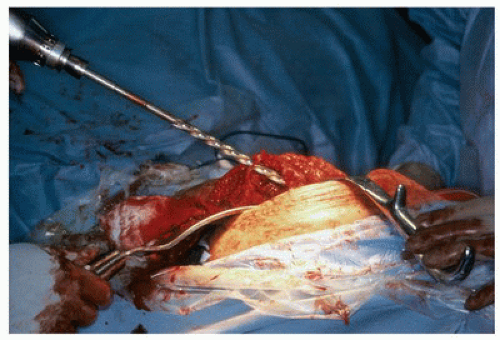
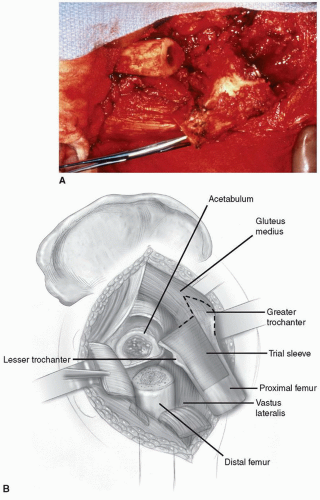 FIGURE 18-6 Initial transverse osteotomy distal to the trial sleeve, approximately 3.5 cm distal to the lesser trochanter. |
Each modular stem has its unique nuances. I use the S-ROM stem (DePuy, Warsaw, IN). The following technique applies to this stem. The femoral canal is identified with a box osteotome and canal finder. A three-step milling process then prepares the femoral canal. Step one involves cylindrical diaphyseal reaming until firm endosteal cortical contact is achieved to prepare the distal femur
(see Fig. 18-8). In small femoral canals or Type A bone, begin with the smallest diameter reamer and increase in 0.5- to 1.0-mm increments. The final reamer should match or be 0.5 mm greater than the minor diameter of the chosen stem. If subtrochanteric osteotomy has been performed, reamers can be placed into the distal bone fragment through the osteotomy site to a depth matching or exceeding the final stem placement after excision of the subtrochanteric fragment.
(see Fig. 18-8). In small femoral canals or Type A bone, begin with the smallest diameter reamer and increase in 0.5- to 1.0-mm increments. The final reamer should match or be 0.5 mm greater than the minor diameter of the chosen stem. If subtrochanteric osteotomy has been performed, reamers can be placed into the distal bone fragment through the osteotomy site to a depth matching or exceeding the final stem placement after excision of the subtrochanteric fragment.
The proximal femur is prepared in two steps. A shaft pilot, matching the minor stem diameter, directs proper placement of the proximal reamers. Conical metaphyseal reamers in 2-mm increments are placed until firm AP proximal diaphyseal and metaphyseal contact is obtained without excessive thinning of the proximal endosteal cortex (see Fig. 18-9). Calcar miller reamers are then used to mill




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree