Richard D. Scott
Minor Bone Defect Management in Revision Knee Arthroplasty
DEFINITION OF MINOR BONE DEFECTS
TIBIAL MINOR DEFECT RECONSTRUCTION TECHNIQUES
SURGICAL TECHNIQUE FOR MODULAR TIBIAL AUGMENTATION
DEFINITION OF MINOR DEFECTS—FEMUR
FEMORAL MINOR DEFECT RECONSTRUCTION TECHNIQUES
Bone defects are commonly encountered in revision total knee arthroplasty. The variability in the size and location of these defects has led to the development of many techniques aimed at restoring the physical integrity of the knee and supporting revision prosthetic replacement. We recognize three goals in the management of these defects. First is to achieve a reconstruction that allows immediate weight bearing. When immediate weight bearing is allowed, rehab protocols, which facilitate optimal range of motion, can be employed. Second, reconstructive options should ensure long-term implant stability. And third, when feasible, bone stock restoration should be prioritized. The options available to a reconstructive surgeon for management of these minor defects include bone grafting via allogeneic and occasionally autologous sources, simple defect fill with polymethylmethacrylate, reinforced cement with screens or screws, modular augmentation associated with the reconstructive prosthesis, impaction grafting techniques, or possibly custom prosthetic repair. This chapter defines both the techniques and reported experience in the management of minor defects about the knee in revision knee arthroplasty.
DEFINITION OF MINOR BONE DEFECTS
Patterns of bone loss vary extensively in revision total knee arthroplasty. Many series discussing revision total knee arthroplasty outcomes fail to specify defects encountered at the time of reconstruction in a manner that adequately addresses this variability. Unfortunately, “minor defects” encountered by a surgeon who frequently performs revision arthroplasty may be considered relatively “major defects” to surgeons or centers who have less familiarity with revision surgery. The classification system proposed by the Anderson Orthopaedic Research Institute (AORI) is a system best represented in the literature and provides a classification guideline for the evaluation of bone defects at the time of revision knee arthroplasty (Table 45.1).1
TABLE 45.1 The AORI Classification of Bony Defects
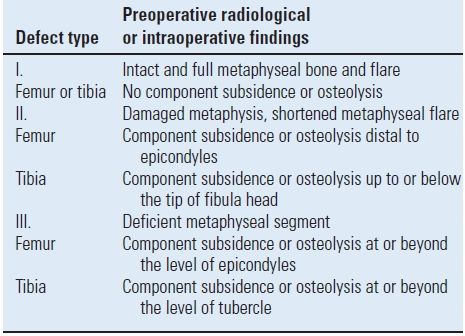
This chapter will focus on Type I and Type II defects. A Type I defect is a minor defect present when, after removal of the implants, the metaphyseal bone remains intact. This situation is commonly found in the absence of significant prior components subsidence or osteolysis. A Type II defect Definition of Minor Bone Defects includes bone loss extending into the metaphyseal flare of the knee. On the femoral side, Type II bone loss is defined by bone loss distal to the epicondyles. On the tibial side, Type II bone loss is defined as proximal tibial bone destruction, which may extend as low as, but not below, the tip of the proximal fibula. When the bone loss extends proximally or distally beyond these boundaries, by definition, major bone loss is present (Type III and Type IV), and reconstructive options are discussed elsewhere in this text. The significance of the AORI classification system is that it suggests a strategy for management options based on the degree of bone loss. This classification system lacks, unfortunately, consideration of other factors that impact reconstructive choices including ligament stability and endosteal bone integrity, both of which have implications with regard to prosthetic constraint and stem selection.2
Most reconstructive surgeons begin the revision process by reconstruction of the proximal tibia, a foundation for both implant orientation and gap balancing. The failure mechanisms leading to minor bone loss on the tibia typically include infection, aseptic loosening, and/or osteolysis. When the prosthetic bond to the patient is lost, there is a relatively linear observed relationship between the time that the implant remains in situ and the amount of bone lost.3 Additionally, after the prosthetic bond is abrupted, angular subsidence of the implant can occur, particularly if preexisting varus or valgus angulation is present (Fig. 45-1). In such situations, the cortical rim of the proximal tibia is in jeopardy. Loss of the proximal cortical rim may lead to uncontained defects and hence the loss of circumferential support for the next reconstruction. When these cortical rim defects occur at a level <10 to 15 mm from the native joint line, they may simply be resected and replaced with a new revision tibial tray with a thicker polyethylene insert.2,4,5 However, the anatomy of the proximal tibia results in rapid tapering in a metaphyseal flare. Resection of the base of the defect may result in significantly reducing the area of the proximal tibia and hence the size of the revision tibial tray that can be used to cap the tibia without overhanging the edges of the proximal bone, a condition that can lead to soft tissue irritation and pain. Many revision knee systems link the size of the femoral implant to that of the tibial implant. Consequently, significant reduction in the size of the tibial base plate can compromise prosthetic options on the femoral side of the reconstruction.
FIGURE 45-1. Angular subsidence of a loose implant or wear, as in this case, can lead to the loss of cortical bone and an uncontained defect. (Reproduced with permission from Engh GA, Rorabeck CH. Revision Total Knee Arthroplasty. Baltimore, MD: Williams & Wilkins; 1997.)
TIBIAL MINOR DEFECT RECONSTRUCTION TECHNIQUES
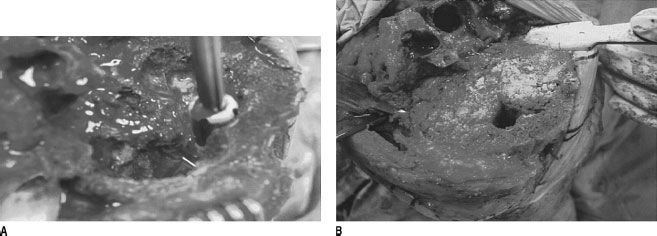
In situations where minor defects are cavitary or contained, bone grafts can be used to achieve all three reconstructive goals. Impaction of cancellous bone graft has several distinct advantages including ready availability in most OR theatres, relatively low cost, reliable incorporation, and general ease of surgical employment.6–11 In the revision setting, allograft is typically selected over autograph due to host availability. Occasionally, however, bone resection slivers, metaphyseal cancellous bone, or iliac crest graft can be utilized. The ready availability of processed allograft sources makes this graft option more commonly used. Because particulate bone graft is readily incorporated, even deep cavitary defects with intact proximal cortical rim can be successfully managed provided diaphyseal engaging stems accompany the reconstruction12,13 (Fig. 45-2A,B).
FIGURE 45-2. A: Large cavitary defects of the proximal tibia may be managed with impaction of allograft bone. The stem position is maintained with trials. B: Cancellous chips are density packed with a contained defect. (Reproduced with permission from Engh GA, Rorabeck CH. Revision Total Knee Arthroplasty. Baltimore, MD: Williams & Wilkins; 1997.)
The depth of resection of the proximal tibia in the face of cortical bone loss is dependent upon a number of factors including the size of the cortical defect, the width of the defect as a percentage of the total circumference of the proximal cortical tibial flare, as well as the age and activity level of the patient. Generally speaking, however, transverse tibial resections to the base of the defect above the level of the proximal fibula are well tolerated. This allows for a stable cortical rim for tibial base-plate abutment and can be performed without potential compromise to the extensor mechanism anteriorly or the lateral fibular collateral ligament. If the cortical defect, however, extends below the level of the proximal fibula, resection to the base of such defect may have several negative consequences. The first of these relates to the rapidly tapering nature of the proximal tibia. The surgeon will be forced to use a smaller tibial base plate with a deeper resection level, which may have consequences as mentioned above in the selection of the femoral implant. Another consequence is the potential for thicker polyethylene (Fig. 45-3). Extreme thicknesses of polyethylene may result in impingement anteriorly of the patella tendon and patella in deep flexion.14 Thicker polyethylene may also present problems for modular tray locking mechanisms long-term as increased polyethylene thickness has been associated with increased micromotion and backside wear in modular tibial trays.
FIGURE 45-3. Medial and lateral modular augments may be used to reduce the height of the tibial polyethylene insert. (Reproduced with permission from Engh GA, Rorabeck CH. Revision Total Knee Arthroplasty. Baltimore, MD: Williams & Wilkins; 1997.)
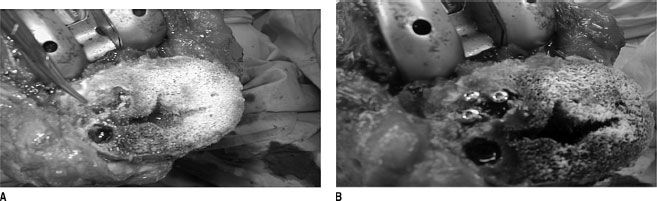
Uncontained proximal tibial defects, which account for <25% of the circumference of the cortex tibial intact, can generally be managed with any of the previously mentioned techniques provided a stem is used to bypass the defect and engage the metadiaphysis15,16 (Fig. 45-4A,B).
FIGURE 45-4. A: Small uncontained defects are frequently encountered on this tibia. B: One strategy is cement fill with screw support. (Reproduced with permission from Engh GA, Rorabeck CH. Revision Total Knee Arthroplasty. Baltimore, MD: Williams & Wilkins; 1997.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree