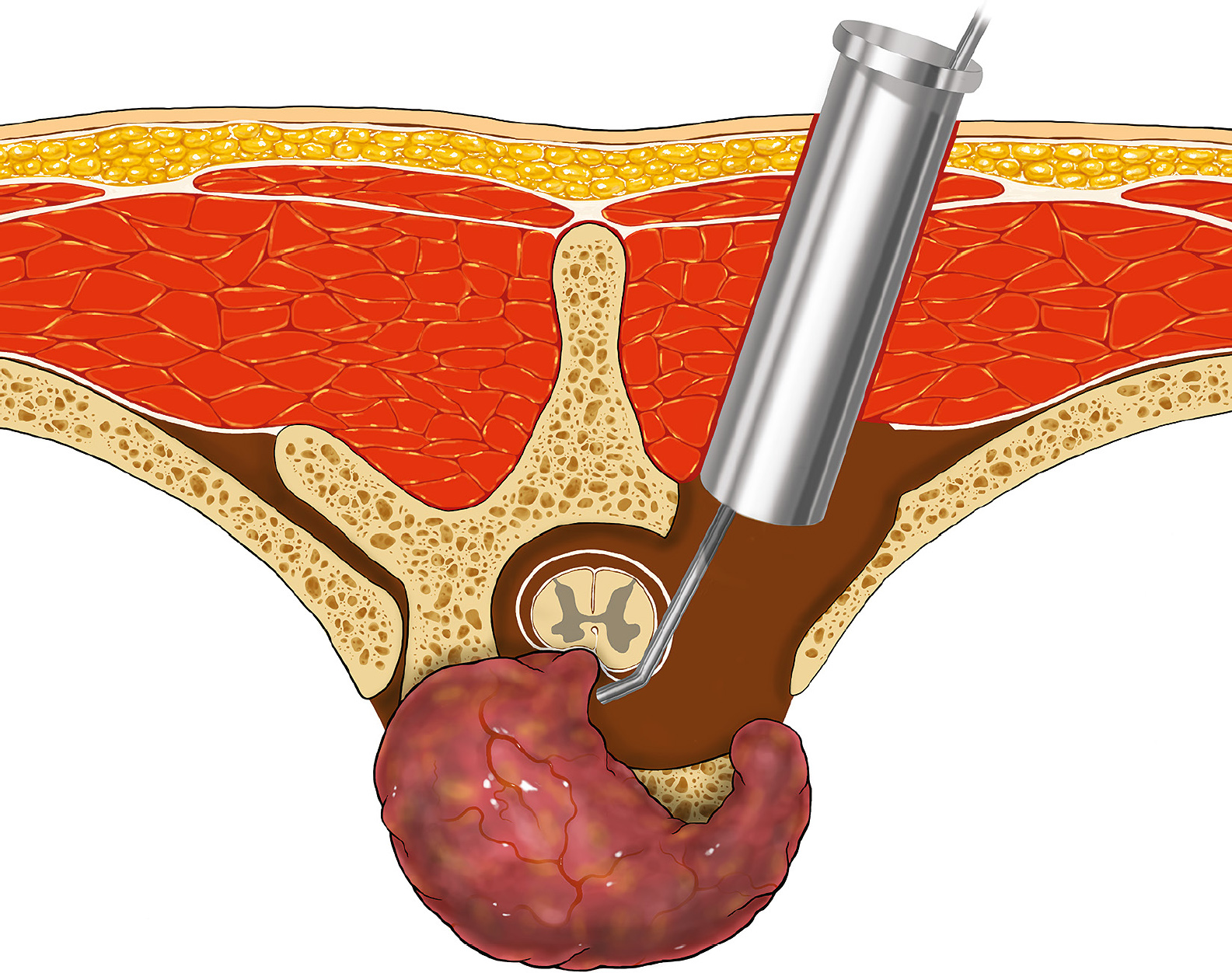
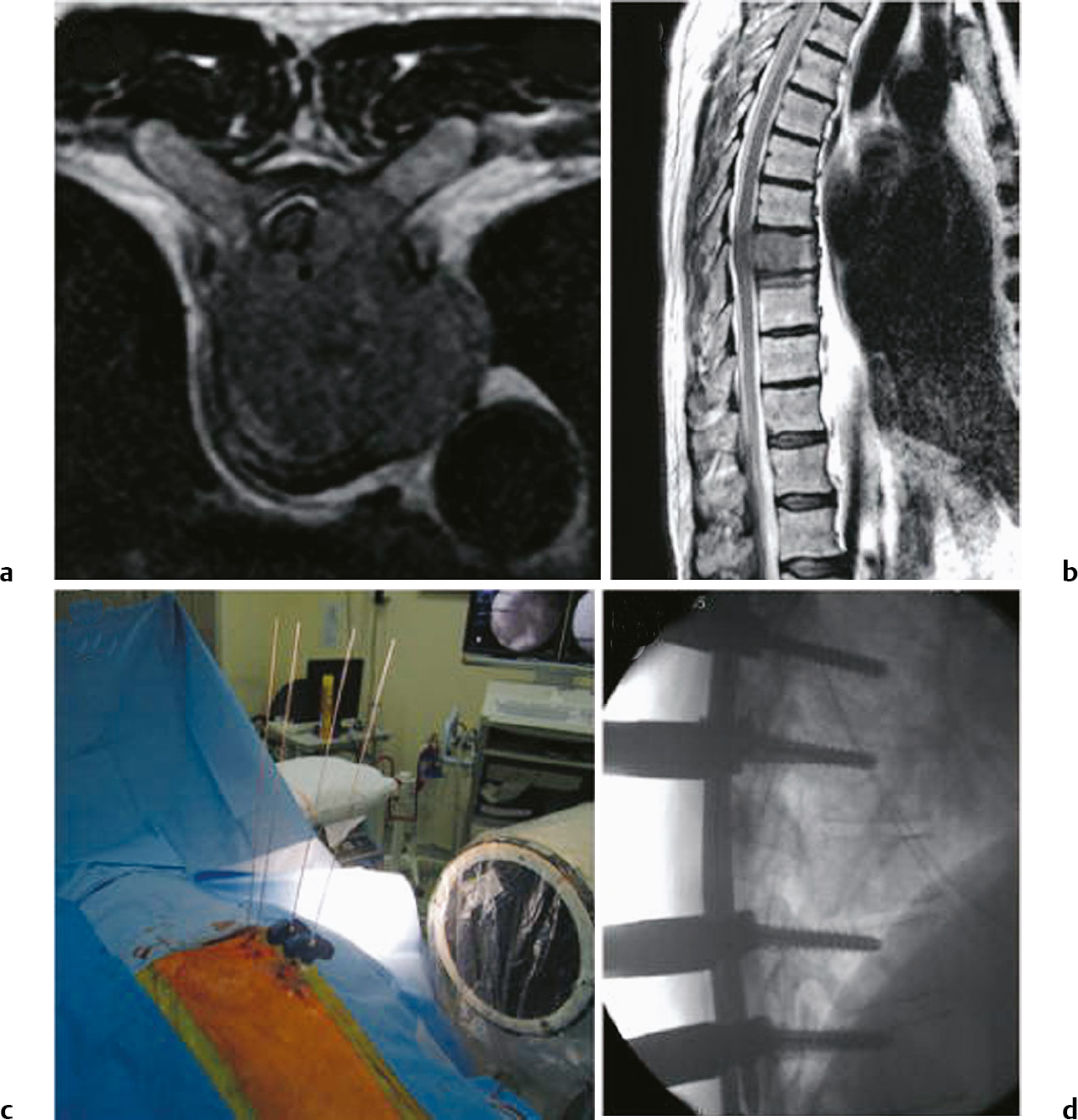
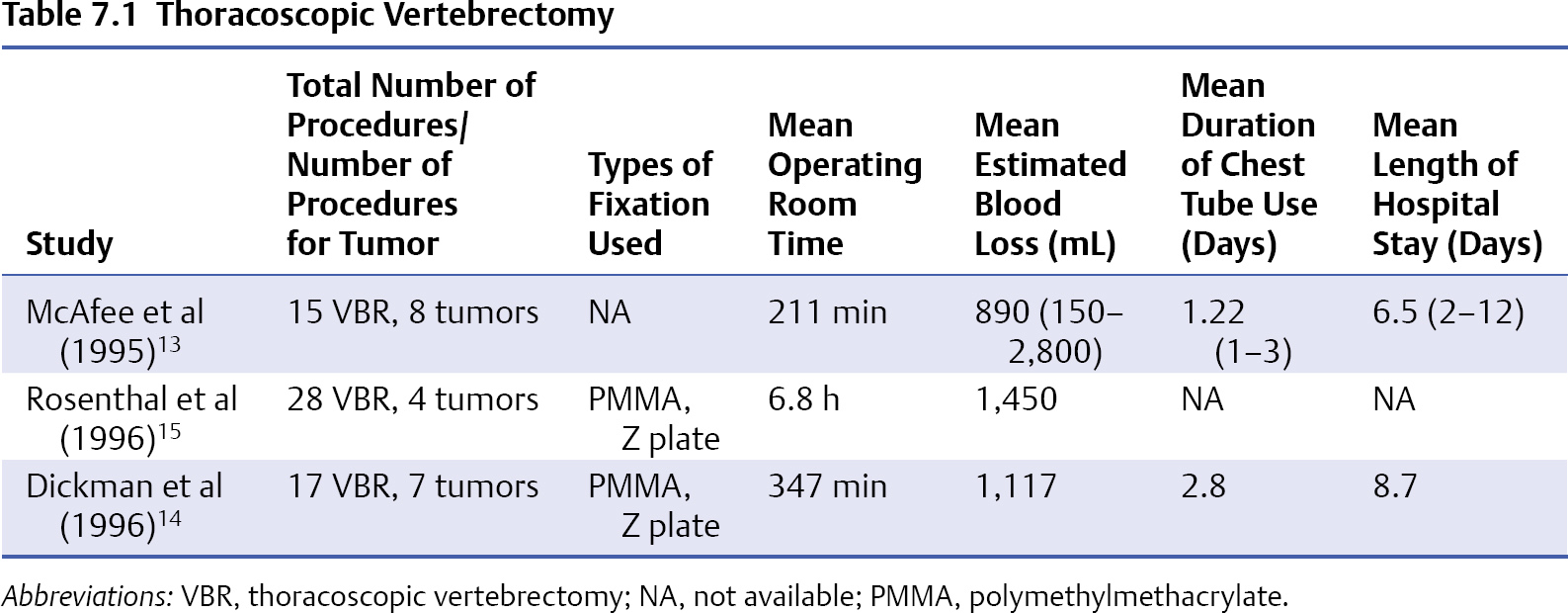
7 Minimally invasive treatment (MIT) of spinal tumors is becoming increasingly complex, and multiple specialties are contributing to bring their techniques to the fore.1 These modalities include percutaneous techniques (e.g., image-guided biopsy, embolization, cement augmentation, radiofrequency ablation) and minimally invasive surgery (MIS) techniques. Current MIS techniques are key components of MIT for the treatment of metastatic spine disease. This chapter defines MIS, discusses the MIS techniques that can be used in addition to traditional open techniques, examines potential criteria for the use and evaluation of MIS techniques, and provides an overview of posterior and anterior surgical MIS techniques, focusing on the thoracoscopic approach for tumor resection via corpectomy, followed by reconstruction and stabilization. Although a precise definition of the term minimally invasive is elusive, most authors agree that MIS involves surgical techniques that reduce collateral tissue damage most commonly associated with surgical access (approach).2 MIS can potentially decrease access-associated morbidity such as postoperative wound infection, reduce the need for blood transfusion, and enable faster recovery by allowing for earlier postoperative adjuvant treatment (e.g., radiation, chemotherapy). Minimally invasive surgery can also entail doing less surgery at the target site under the principle that “less is more.” If a better outcome would be expected from adjuvant treatment after an initial surgery, that option should be considered. For example, decompressing the spinal cord without removing all the tumor tissue might be sufficient if the patient is a suitable candidate for radiation after surgery.3 In that sense, MIS can entail doing less surgery to achieve the equivalent or better outcome compared with more extensive surgical resection. For example, Laufer et al3 recently published a series of 186 patients treated with “separation surgery” followed by adjuvant hypofractionated or high-dose single-fraction radiosurgery. Although minimal access techniques were not used in this series, “separation surgery” conceptually shows that less surgery can achieve equal or better results for palliative care of metastatic spine disease. It involves decompression of the thecal sac by a limited posterior lateral tumor resection and posterior segmental instrumentation, followed by postoperative cytotoxic radiosurgery doses that spare the spinal cord. The results show that local tumor control was achieved in the majority of patients, with a cumulative incidence of local progression 1 year after radiosurgery of 16.4%. Only four patients required reoperation. Thus, it is difficult to reach a consensus on a definition of MIS, which can have different meanings for different authors. It is similarly difficult to define the added value of MIS based on quality and cost measures. The Text Box lists some of the criteria I use to evaluate and justify MIS procedures including those undertaken for metastatic spine disease. Although by no means a complete list, these criteria can be used to analyze and compare various surgical approaches including open, mini-open, endoscopic, and percutaneous techniques. Criteria for minimally invasive spine surgery to be meaningful and valuable 1. Minimizing surgically induced tissue damage a. Smaller, cosmetically appealing skin incision b. Minimal muscle dissection c. Less bone removal 2. Measurable clinical benefit a. Decrease in surgical morbidity and mortality i. Cerebrospinal fluid leak, neurologic worsening, less instability b. Lower intraoperative blood loss i. Less need for blood transfusion ii. Less need for cell saver c. Shorter stay in the hospital i. Fewer days in intensive care unit ii. Shorter overall stay iii. Lower readmission rate d. Resumption of activities i. Less need for rehabilitation ii. Less need for physical therapy iii. Faster return to work e. Lower infection rates f. Lower reoperation rates g. Earlier initiation of postoperative therapies i. Physical therapy, radiation, chemotherapy 3. Clinical effectiveness a. MIS must achieve the intended surgical goal i. Decompression, reconstruction b. MIS must have equivalent or better clinical outcomes i. Neurologic improvement and pain outcome c. MIS must have equivalent or better imaging outcomes i. Fusion rate ii. Spinal canal decompression 4. Favorable socioeconomic effect a. MIS must improve quality i. Increase in quality measures listed above (criteria 1–3) b. MIS must be cost effective i. Upfront cost must be balanced with downstream cost savings ii. Imaging cost associated with MIS c. MIS must be valuable i. Value = quality/cost Posterior surgical approaches are used for laminectomies and transpedicular decompression. More extensive posterolateral approaches like the lateral extracavitary approach allow for extensive posterior and anterior decompression including more complete corpectomy and en bloc resection.4 Because of the extensive soft tissue trauma associated with these traditional approaches, MIS techniques were developed to take advantage of the access trajectory of the approaches by minimizing the incision.5–7 Deutsch et al6 applied the MIS technique using a tubular retractor to access spinal metastasis to the thoracic spine in eight patients (Fig. 7.1). Through unilateral or bilateral 3-cm incisions they performed intralesional, transpedicular vertebrectomies for spinal cord decompression with limited reconstruction using methylmethacrylate. None of the patients underwent spinal stabilization using instrumentation. The mean operative time and mean blood loss were 2.2 hours and 270 mL, respectively. The mean length of stay was 4 days. Postoperatively, 62.5% of patients had improved neurologic function and pain control. All patients underwent postoperative radiation therapy. No complications related to surgery were noted. Zairi et al7 described 10 patients with metastasis to the thoracic spine who were treated with decompressive corpectomy using a tubular retractor. No anterior column reconstruction was performed after transpedicular corpectomy; however, the authors used percutaneous pedicle screw fixation to stabilize the spine (Fig. 7.2). They reported a mean operative time of 170 minutes and mean estimated blood loss of 400 mL. No patient required a blood transfusion. The mean length of stay was 6 days. The only complication reported was a postoperative urinary tract infection. Eighty percent of patients improved by at least one Frankel grade. Fig. 7.1 Illustration of exposure for minimally invasive transpedicular vertebrectomy. The tubular retractor facilitates the lateral exposure so that the anterior portion of the spine can be visualized. (Courtesy of the Department of Neurosurgery, University of Utah.) Both series demonstrated excellent radiographic and clinical results but involved only a small number of patients. It is important to note that in both series patients with overt neo-plastic spinal instability (i.e., kyphosis) were excluded. A major disadvantage of any approach with a posterior incision is the risk of infection, which is particularly high in cancer patients, who are frequently immunocompromised and have often had prior radiation therapy. Infection can be a life-threatening event in oncology because of the limited capacity of patients to fight it despite antibiotic therapy. In addition, infections frequently disqualify patients from adjuvant radiation, chemotherapy, and experimental protocols. Prior studies indicate that the risk of a posterior wound infection in a cancer patient is approximately 12 to 32%, depending on the timing of radiation.8 These initial studies on posterior MIS techniques in cancer patients have not yet clearly demonstrated a lower infection risk compared with standard open posterior and anterior approaches. Fig. 7.2a–d Axial (a) and sagittal (b) T2-weighted magnetic resonance imaging (MRI) depicting spinal cord compression due to a metastasis at T7. (c) The operative photograph shows insertion of the wires on the right side. (d) Lateral fluoroscopy shows the spine after bilateral pedicle screw insertion and the introduction of the rods. (From Zairi F, Arikat A, Allaoui M, Marinho P, Assaker R. Minimally invasive decompression and stabilization for the management of thoracolumbar spine metastasis. J Neurosurg Spine 2012;17(1):21. Reproduced with permission.) Although resection of metastatic spine tumors was historically performed via a posterior laminectomy approach, it frequently resulted in unsatisfactory outcome and neurologic worsening. The most common reason for therapeutic failure is related to the fact that most metastases originate in the vertebral body and are associated with a degree of spinal instability that can be worsened by an indirect decompression with a simple laminectomy. At the same time, anterior open thoracotomy and thoracoabdominal approaches were demonstrating improved outcomes by more effectively addressing the goals of tumor resection, neural decompression, and anterior reconstruction. Transpleural thoracotomy allows for direct access to the spinal canal for decompression, anterior column reconstruction, and stabilization. Thoracotomy can be extended to include the upper lumbar spine by incising the diaphragm (thoracolumbar approach). Several published case series document the excellent outcomes of thoracotomy for pain control, neurologic improvement, and spinal stability for metastatic disease. Gokaslan et al9 reported one of the largest series of patients who underwent traditional thoracotomy for metastatic disease at M.D. Anderson. Seventy-two patients with metastatic spine tumors underwent thoracotomy for transthoracic vertebrectomy, decompression, reconstruction with polymethyl methacrylate, and anterior plate fixation; supplemental posterior fixation was used in seven patients. The study found that 76% of patients had improved neurologic function and 77% of nonambulatory patients regained the ability to walk. Spinal pain decreased in 92.3% (60/65) of patients who initially presented with pain. It is important to note that pain was assessed at 1-month follow-up to allow incisional pain to resolve. Although the risk of wound infection in this series was < 1% (a fraction of the infection risk compared with any posterior incision surgery), the morbidity related to thoracotomy access, including post-thoracotomy pain, was approximately 17%. In many patients, the postthoracotomy pain was severe enough to require narcotics for pain control. Because these thoracotomy techniques still involved access morbidity, several MIS techniques for anterior access have been developed for spine surgery (see Text Box). Minimally Invasive Surgery Approaches and Techniques for Metastatic Spine Disease Mini-thoracotomy and thoracoscopic approaches have been used in cardiothoracic surgery to minimize the access morbidity, and over the years both techniques have been adopted for spine pathologies such as thoracic disk herniation, spine fracture, and tumors. The goal of both anterior MIS techniques is to decrease the access morbidity without compromising the safety and efficacy of the spinal procedure to be performed. At the target disease site, the MIS technique needs to enable a corpectomy to decompress the spinal canal, followed by interbody reconstruction and stabilization. Current anterior mini-open MIS approaches use either a retropleural or transpleural approach. Most patient series are small and retrospective evaluations, but they demonstrate the feasibility of the mini-open approach. Huang et al10 reported a retrospective series of 46 patients with spine metastases: 29 underwent mini-thoracotomy and 17 underwent standard thoracotomy for anterior corpectomy and reconstruction. Clinical and surgical outcomes were similar with the two techniques; however, only 6.9% of mini-thoracotomy patients required a stay as long as 2 days in the intensive care unit compared with 88% of the standard thoracotomy group. Uribe et al11 reported their experience of a mini-open retropleural approach for thoracic tumor removal in 21 patients, although the majority of tumors were not metastatic but rather other primary intra- and extradural lesions. Operating time, estimated blood loss, and length of stay were 117 minutes, 291 mL, and 2.9 days, respectively. I prefer to use a table-mounted retractor system for mini-open thoracotomy (SynFrame, DePuy Synthes, West Chester, PA). Payer and Sottas12 reported a case series of 37 patients in whom the SynFrame was used. Eleven patients had metastatic spine lesions. The mean operating time and mean blood loss were 188 minutes and 711 mL, respectively. Two patients had complications. Neurologic and pain improvement were excellent. The major advantage of the mini-open thoracotomy is that it enables the surgeon to use the microscope or loupes for a three-dimensional view of the spine. In addition, the lung does not need to be deflated or at least can be partially ventilated during surgery. Disadvantages of the mini-open approach are the relatively longer incision and the partial removal of the rib that is necessary. This rib resection can cause pain in the postoperative period and can affect the patient’s ability to breathe. Another disadvantage of the mini-open technique is the difficulty with using appropriate surgical tools. Because of the long working distance from the chest wall to the spine, many traditional micro-tools are too short. In addition, many tools used for thoracoscopic surgery are too long to fit under the microscope easily and they interfere with direct visualization of the target site. This problem can be circumvented by either using surgical loupes or a microscope with long focal length. Alternatively, a hybrid technique using both loupes and the endoscope, which gives more room to use longer tools, can be employed.
Minimally Invasive Surgery for Metastatic Spine Disease
 Introduction
Introduction
 What Is Minimally Invasive?
What Is Minimally Invasive?
 Posterior and Posterolateral Approaches
Posterior and Posterolateral Approaches
 Anterior and Anterolateral Approaches
Anterior and Anterolateral Approaches
Traditional Thoracotomy
 Posterior/posterolateral
Posterior/posterolateral
 Percutaneous/mini-open pedicle screw fixation
Percutaneous/mini-open pedicle screw fixation
 Tubular access for decompression
Tubular access for decompression
 Anterior/anterolateral
Anterior/anterolateral
 Mini-open thoracotomy (transpleural, retropleural)
Mini-open thoracotomy (transpleural, retropleural)
 Video-assisted thoracoscopic surgery
Video-assisted thoracoscopic surgery
Mini-Open Thoracotomy
< div class='tao-gold-member'>
Minimally Invasive Surgery for Metastatic Spine Disease
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree